What is the therapeutic range of heparin?
- The anti-Xa assay is now available on many automated coagulation analyzers.
- Unlike the PTT, the anti-Xa assay is not affected by under-filled collection tubes—a common preanalytic problem.
- The anti-Xa assay is not susceptible to interference from elevated concentrations of factor VIII or fibrinogen that result from acute phase reactions.
When should heparin injections start?
Heparin should not be injected into a muscle. Heparin is sometimes injected one to six times a day and sometimes given as a slow, continuous injection into the vein. When heparin is used to prevent blood clots from forming in intravenous catheters, it is usually used when the catheter is first put in place, and every time that blood is drawn ...
Can aspirin prevent a DVT?
Low-dose aspirin can help prevent pre-eclampsia, a pregnancy complication that can be very harmful to mother and baby.The condition can cause increased blood pressure, damage to the liver and kidneys, blood clots and pulmonary edema. It can result in pre ...
Can Lovenox be administered with heparin?
When heparin and Lovenox® are administered, heparin can be given either intravenously or subcutaneously — under the skin. Lovenox® is only injected subcutaneously. Frequent monitoring of blood clotting ability is required when the patient is using heparin, but with Lovenox® the monitoring can be much less frequent.

Usual Adult Dose For Deep Vein Thrombosis
The manufacturer provides the following dosing guidelines based on clinical experience:Continuous IV infusion:-Initial dose: 5000 units by IV injec...
Usual Adult Dose For Cardiothoracic Surgery
Initial dose: At least 150 units/kg; frequently, 300 units/kg is used for procedures estimated to last less than 60 minutes or 400 units/kg for tho...
Usual Adult Dose For Blood Transfusion
Addition of 400 to 600 USP units per 100 mL of whole blood is usually employed to prevent coagulationUse: Anticoagulant use in blood transfusions.
Usual Adult Dose For Patency Maintenance of Indwelling Intravenous Devices
6 units/hr (using 2 units/mL formulation) has been found to be satisfactoryComments: Rate of infusion depends upon age, weight, clinical condition,...
Usual Pediatric Dose For Thrombotic/Thromboembolic Disorder
Neonates:Systemic to pulmonary artery shunt thrombosis: 50 to 100 units/kg IV bolus; consideration should be given to ongoing infusion.Central veno...
Is heparin safe for deep vein thrombosis?
Optimal dosing of subcuta neous unfractionated heparin for the treatment of deep vein thrombosis. Twice-daily, inpatient, subcutaneous unfractionated heparin is at least as effective and safe as continuous intravenous unfractionated heparin for the treatment of acute deep vein thrombosis.
Is heparin a subcutaneous unfractionated heparin?
Subcutaneous unfractionated heparin therefore may be suitable for outpatient treatment of deep vein thrombosis. The purpose of this study was to develop a dosing nomogram for a dose each 12 hours (2 doses per day) 12-hourly subcutaneous unfractionated heparin that is suitable for outpatient treatment of acute deep vein thrombosis.
What is the therapeutic range of heparin?
The CAP suggests the one-time establishment of a heparin concentration-derived aPTT therapeutic range. The cumulative summation method is suggested for range re-evaluation following reagent/instrument change. When anti-Xa monitoring is used, a therapeutic target of 0.3–0.7 units/mL is suggested.
How much heparin should I infuse for VTE?
In 1993, Raschke et al. compared weight based heparin dosing (80 units/kg followed by 18 units/kg/h) to a standard regimen (5000 units followed by 1000 units/h) in 115 patients with venous or arterial thrombosis [6]. A five-fold reduction in recurrent VTE was observed with weight-based dosing (95 % CI 1.1–21.9). Nevertheless, most VTE treatment trials incorporated a fixed dose initial heparin infusion regimen of 5000 unit bolus followed by infusion of approximately 1300 units /h [7]. In 1992, the ACCP VTE treatment guidelines suggested a 5000–10,000 unit bolus followed by a fixed heparin infusion of 1300 units/h (31,200 units/day) and in 1995 and 2004 they endorsed either a fixed regimen or the Raschke weight based regimen [8–10]. For a 70 kg patient, the Raschke regimen translates into a heparin bolus of 5600 units followed by infusion of 1260 units/h. The 2012 version of the guidelines do not address UFH dosing in the VTE treatment chapter [11]. However, in the chapter on parenteral anticoagulants, UFH dosing recommendations are similar to those in 1995 and include either a weight based regimen (Raschke regimen) or a fixed regimen of 5000 unit bolus followed by a continuous infusion of at least 32,000 units/day [12].
How often should heparin be monitored?
We suggest using anti-Xa level monitoring in patients with heparin resistance, a prolonged baseline aPTT or altered heparin responsiveness. We suggest the aPTT or anti-Xa level be checked every 6 h until two consecutive therapeutic results are obtained, after which the frequency of monitoring can be extended to once daily.
Is heparin anti-XA better than aPTT?
A recent review identified the potential advantages of the heparin anti-Xa level over the aPTT for heparin monitoring. Advantages included fewer monitoring tests, fewer dose changes and a shorter time to obtain therapeutic anticoagulation [20]. Large VTE trials evaluating patient outcomes with heparin anti-Xa level monitoring are not available. Although both the aPTT and the anti-Xa level can be used to monitor heparin, paired results within individual patients are often discordant [21]. In a recent trial in which clinical outcomes of aPTT versus anti-Xa monitoring were evaluated, a disproportionate prolongation of the aPTT relative to the anti-Xa level was the most common discordant pattern [22]. Patients with relatively high aPTT to anti-Xa levels had higher rates of major bleeding and death compared to patients with concordant paired test results. National guidelines for heparin monitoring recognize the limitations of both approaches without recommending a preferred approach [23].
Is heparin used for venous thromboembolism?
Heparin has been a component of the initial treatment of venous thromboembolism (VTE) for decades. Despite its long history, various aspects of the practical use of unfractionated heparin (UFH), whether delivered intravenously (IV) or subcutaneously (SC), continue to challenge clinicians. In 1998, the US FDA approved the low molecular weight heparin (LWMH) enoxaparin (Lovenox) for VTE treatment, followed by approval of the synthetic heparin-like compound fondaparinux (Arixtra) in 2004. In 2007, the LMWH dalteparin (Fragmin) was approved for VTE treatment in patients with cancer. These agents, intended for subcutaneous administration, offer practical advantages over unfractionated heparin, yet present their own challenges, particularly in special populations. This chapter will address the practical use and management of the parenteral heparin anticoagulants available in the US when used in the treatment of VTE.
Is anti-XA level monitored with heparin?
Direct anti-Xa level monitoring is recommended in those with heparin resistance (see subsequent section), baseline aPTT elevation from a lupus anticoagulant or contact factor deficiency or those with markedly elevated levels of fibrinogen or factor VIII [24].
What is the primary objective of heparin therapy?
The primary objective of initial heparin therapy in such patients is to prevent recurrent venous thromboembolism.
How long does heparin stay in your system?
Heparin is continued for 7-10 days, overlapped with warfarin sodium during the last 4-5 days. Multiple randomized clinical trials indicate that this approach is highly effective. An alternative approach is to commence heparin and oral anticoagulants together at the time of diagnosis, and to discontinue heparin on the fourth or fifth day. ...
What is the treatment for pulmonary embolism?
Heparin therapy for venous thrombosis and pulmonary embolism. Intravenous heparin is the initial treatment of choice for most patients with acute pulmonary embolism or proximal deep vein thrombosis. The primary objective of initial heparin therapy in such patients is to prevent recurrent venous thromboembolism.
How long does it take for a heparin thrombosis to develop?
The central clinical feature of HIT is thrombocytopenia that typically occurs 5 to 10 days after heparin exposure, although it may develop more rapidly in patients previously exposed to heparin within the preceding 100 days. 44 In 90% of cases, the platelet count decreases to <150 · 10 9 /L, but a decline of 50% from the baseline platelet count should raise clinical suspicion. 44 Thrombosis is a common complication and is more frequently venous than arterial. In the absence of alternative anticoagulant therapy, 25% to 50% of patients without thrombosis at the time of HIT subsequently develop thrombotic complications, despite cessation of heparin. Skin reactions and systemic reactions to heparin injections are less common manifestations. 44
What is heparin induced thrombocytopenia?
Heparin-induced thrombocytopenia (HIT) is a clinicopathological syndrome; 44 its diagnosis is based on characteristic clinical events and concurrent laboratory detection of HIT antibodies in the setting of recent heparin therapy. The pathogenic antibodies are directed against multimolecular complexes of platelet factor 4 (PF4) and heparin, and stimulated by neoepitopes expressed on PF4 in response to heparin binding. 44 Interaction of the antigen/antibody complex with platelets and binding of antibody to platelet Fc receptors result in platelet activation and aggregation. 45 The end result is increased thrombin generation, which may be associated with arterial or venous thrombosis. 44
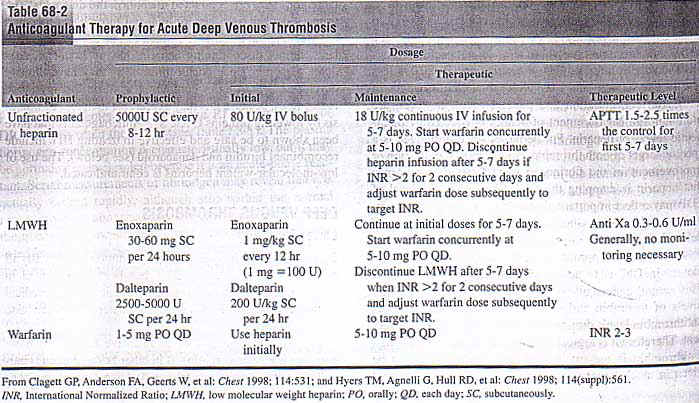
What is the standard of care for acute VTE?
Anticoagulant therapy is the standard of care in patients presenting with acute VTE. Inpatient treatment with IV UFH is being replaced by outpatient therapy with LMWH as the most commonly used anticoagulant regime. Following is a review of the efficacy, safety, and appropriate dosage of both UFH and LMWH.
What is the treatment for uncomplicated PE?
Treatment of patients with uncomplicated PE or DVT involves similar anticoagulant regimens, 4 in part because asymptomatic PE occurs frequently in patients with symptomatic proximal DVT, 5,6 and vice versa. 7,8 This review describes the initial treatment of VTE, including: (1) initiation of anticoagulant therapy with either unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH); 9 (2) potential complications of anticoagulant therapy; (3) initiation of warfarin therapy; (4) indications for systemic thrombolytic therapy; and (5) management of VTE in pregnancy.
What anticoagulant is used for HIT?
For patients with HIT, even those without VTE at diagnosis, an anticoagulant other than heparin is recommended. 44 LMWH is not an optimal alternative to UFH because of a high risk of clinically significant cross-reactivity with the HIT antibodies. Three anticoagulants have been found effective in cohort studies for treatment of HIT, the direct thrombin inhibitors lepirudin and argatroban ( Table 3 ), and danaparoid sodium, a heparinoid, which, however, is no longer available in the United States. There is also anecdotal evidence supporting use of bivalirudin, a hirudin analogue. 44 Because of the risk of precipitating venous limb gangrene, warfarin therapy should be delayed until resolution of thrombocytopenia, particularly in patients with VTE at diagnosis. 45
What is heparin resistance?
Heparin resistance, defined as a requirement of >35 000 U per day of UFH to achieve a therapeutic aPTT, occurs in up to 25% of patients with VTE. 13 In an important randomized trial, 19 monitoring therapy by assessing anti–factor Xa levels (targeted range, 0.35 to 0.67 U/mL) in such patients proved as effective and safe as dose adjustments based on aPTT results, and resulted in a lower mean daily dose of UFH. It is therefore recommended that anti-Xa levels be used to guide UFH therapy in patients with heparin resistance. Consideration should be given to checking for AT deficiency when heparin resistance is associated with recurrent or progressive thrombosis. However, in the majority of cases, decreased AT levels are caused by the heparin therapy itself rather than a primary deficiency state. 13
How long does it take to measure aPTT?
An initial bolus of 5000 U of UFH is usually given, following which the aPTT should be measured 6 hours later. Because physician-directed heparin therapy often results in inadequate dosing, the use of validated nomograms is recommended ( Table 1 ). 20,27 These have been shown to reduce the time required to achieve therapeutic aPTT results 20,27 and to improve patient outcomes. 20 It may be necessary to adapt published nomograms for local use, depending on the sensitivity of institutional aPTT reagents and measuring devices.