Should I try complementary treatments for multiple myeloma?
Before you try any complementary treatments for multiple myeloma, talk to your oncologist. They can tell you whether the therapy is safe for you, if it will interact with your cancer treatments, and if it’s likely to be effective.
What are the side effects of multiple myeloma treatment?
It may be especially helpful in treating myeloma patients with kidney problems. It’s injected into a vein (IV) or under the skin, once or twice a week. Common side effects of this drug include nausea and vomiting, tiredness, diarrhea, constipation, fever, decreased appetite, and lowered blood counts.
Which drugs generate deep responses in multiple myeloma?
For example, in a single-arm phase II trial, Dr. Kazandjian and his colleagues found that treatment with lenalidomide, dexamethasone, and carfilzomib (Kyprolis®) generated deep responses in patients with newly diagnosed multiple myeloma.
How is multiple myeloma treated with plasmapheresis?
Plasmapheresis Plasmapheresis can be used to remove myeloma protein from the blood. It’s helpful when certain myeloma proteins build up, thicken the blood, and interfere with circulation (called hyperviscosity). Most often, this procedure is done through a large catheter (tube) placed in a vein in the neck, under the collarbone, or in the groin.
What toxic chemicals cause multiple myeloma?
People who have been exposed to radiation or to asbestos, benzene, pesticides, and other chemicals used in rubber manufacturing may be at higher risk for developing myeloma. People often exposed to wood products, such as carpenters, furniture makers, and paper makers, are also at higher risk.
Which immunoglobulin is affected in multiple myeloma?
Quantitative immunoglobulin (Ig) test A high level of one of these immunoglobulins is often present in multiple myeloma. IgG and IgA are the immunoglobulins most often found in high amounts in people with multiple myeloma.
What vitamins help multiple myeloma?
Vitamin B-12 works together with folate to form red blood cells. A deficiency in B-12 can further decrease the bone marrow's ability to make and maintain red blood cells in people with multiple myeloma.
Why do multiple myeloma patients take dexamethasone?
Dexamethasone and the other steroids are useful in myeloma treatment because they can stop white blood cells from traveling to areas where cancerous myeloma cells are causing damage. This decreases the amount of swelling or inflammation in those areas and relieves associated pain and pressure.
What are the symptoms of high IgG?
The most common antibody is Immunoglobulin G (IgG). People with hypergammaglobulinemia most often have increased levels of IgG....Symptoms to watch forincreased blood count of gamma globulins.deficiencies of certain antibodies.inflammation.swollen lymph nodes.fatigue.stiffness.
How high is IgG in myeloma?
Serum M-protein levels were higher in patients with IgG (median, 33 g/l; range, 0–97 g/l) than in those with IgA (median, 21 g/l; range, 0–87 g/l), while lowest levels were recorded in patients with IgD MM (median, 3 g/l; range, 0·01–45 g/l).
What foods should I avoid with myeloma?
Since multiple myeloma makes your immune system weaker, you'll need to steer clear of any foods that could make you sick, including:Raw meat or fish.Runny eggs.Unpasteurized drinks.Sushi.Unwashed fruits and vegetables.
Is coffee good for multiple myeloma?
Overall, our findings showed no significant association between coffee or green tea consumption and the risk of malignant lymphoma or multiple myeloma for both sexes.
Can you take vitamin D if you have myeloma?
There is no specific recommendation about vitamin D supplements for myeloma patients. However, it is recommended that all adults in the UK consider taking a daily supplement containing 10 micrograms of vitamin D during the autumn and winter.
What side effects does dexamethasone have?
Dexamethasone may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:upset stomach.stomach irritation.vomiting.headache.dizziness.insomnia.restlessness.depression.More items...•
What is the newest treatment for multiple myeloma?
The latest approval is for the combination of daratumumab plus hyaluronidase-fijh (Darzalex Faspro) plus carfilzomib (Kyprolis) and the steroid dexamethasone for the treatment of adults with relapsed or refractory multiple myeloma who received one to three prior treatments.
What happens when you stop dexamethasone?
Too rapid a withdrawal of dexamethasone may cause symptoms such as bone and muscle pain, fatigue, weight loss, nausea, and vomiting. Delay the administration of "live vaccines" for several months after dexamethasone treatment has stopped.
What is the best treatment for low red blood cell count?
Epoetin (Procrit) and darbepoetin (Aranesp) are drugs that can help improve low red blood cell counts and reduce the need for blood transfusions in some patients who are getting chemotherapy .
Can multiple myeloma cause sinus infections?
Patients with multiple myeloma often have low levels of the normal antibodies (immunoglobulins) needed to fight infection. This can lead to problems with lung and/or sinus infections that keep coming back.
Can you get anemia from multiple myeloma?
Some patients develop low red blood cell counts ( anemia) from multiple myeloma or its treatment. They might feel tired, lightheaded, or short of breath while walking. Anemia that’s causing symptoms can be treated with blood transfusions. These are often given on an outpatient basis.
Does plasmapheresis kill myeloma cells?
Although plasmapheresis lowers the abnormal protein level and can relieve symptoms for a time, it does not kill the myeloma cells.
What is the treatment for multiple myeloma?
Treatments for MM include corticosteroids, alkylating agents, anthracyclines, proteasome inhibitors, immunomodulatory drugs, histone deacetylase inhibitors and monoclonal antibodies. Survival outcomes have improved substantially due to the introduction of many of these drugs allied with their rational use. Nonetheless, MM patients successively relapse after one or more treatment regimens or become refractory, mostly due to drug resistance. This review focuses on the main drugs used in MM treatment and on causes of drug resistance, including cytogenetic, genetic and epigenetic alterations, abnormal drug transport and metabolism, dysregulation of apoptosis, autophagy activation and other intracellular signaling pathways, the presence of cancer stem cells, and the tumor microenvironment. Furthermore, we highlight the areas that need to be further clarified in an attempt to identify novel therapeutic targets to counteract drug resistance in MM patients.
What is the treatment for MM?
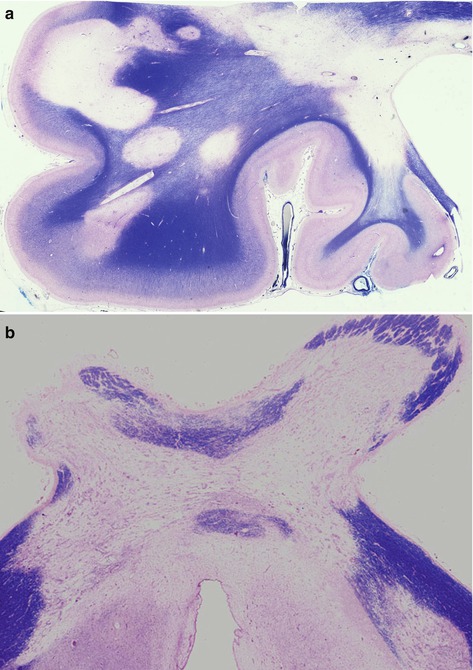
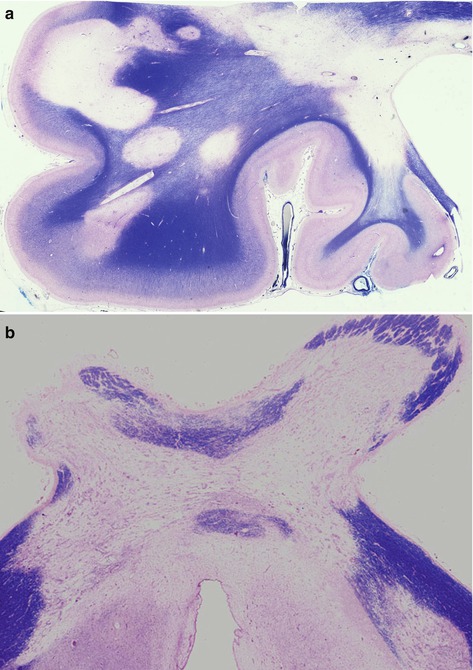
Treatment of MM usually includes different combinations of drugs having different mechanisms of action—corticosteroids, alkylating agents, anthracyclines, proteasome inhibitors (PIs), immuno-modulatory drugs (IMIDs), histone deacetylase inhibitors (iHDACs), monoclonal antibodies (mAbs), nuclear export inhibitors and high-dose chemotherapy rescued by autologous stem cell transplantation (ASCT) [27,28]. Most of these therapeutic options are represented in Figure 2. For many years, therapies were based on cytotoxic drugs, mainly melphalan, an alkylating agent (Figure 2a), and prednisone, a corticosteroid [29]. Later, high-dose chemotherapy (HDT) with melphalan rescued by ASCT was introduced, resulting in extended overall survival for younger patients when compared with conventional chemotherapy [30]. For elderly patients, the most used treatment consisted of the oral combination of melphalan and prednisone. Nonetheless, over the last two decades, new drugs such as thalidomide, bortezomib and lenalidomide were included in the treatment of these patients [31]. The use and optimization of combinations of these drugs allowed improving the overall survival of MM patients – the median survival was of 2.5 years prior to 1997, 4 years in the following decade and over 7 years more recently [5,8,32]. However, resistance to these agents has been observed and MM patients who became refractory to both first generation IMIDs and PIs have significant worse outcomes [33]. Furthermore, next generation IMIDs and PIs were developed and introduced in the therapy of relapsed and refractory patients, and more recently, regimens combining the use of mAbs and iHDACs were also approved for MM treatment [34,35]. Consequently, the selection of the primary treatment has changed over time. Patients are usually stratified by age, performance status and comorbidities, in order to evaluate potential candidates for ASCT [9,36,37]. Advanced age and frailty of patients are life-threatening factors [38]. Nonetheless, age should not limit the access to new drugs or treatment modalities. Elderly fit patients also benefit from ASCT, as younger patients do [37,39]. Disease aggressiveness, namely cytogenetics and extramedullary manifestations, also guide the choice of the best treatment approach. Patients with high-risk features [del17p, t(14;16) and t(4;14)] have a median overall survival of 2 to 3 years, even with ASCT, while MM patients without these features have better survival prognosis, of 6 to 7 years [40,41]. Therefore, patients with high-risk myeloma receive denser and more intense treatments [42,43].
What is bortezomib used for?
Bortezomib was the first PI approved for the treatment of NDMM patients and for relapsed and refractory MM (Figure 2b) [51,52,53]. The introduction of this PI represented a breakthrough in the treatment of MM, by preventing pro-apoptotic proteins degradation and leading to the apoptosis of malignant cells [52]. Additionally, by blocking the degradation of inhibitor kappa B (IκB), the inhibitor of nuclear factor B (NFκB), bortezomib suppresses the NFκB signaling pathway preventing the activation of numerous anti-apoptotic genes involved in MM progression [52,53]. Bortezomib also leads to the upregulation of NOXA, a pro-apoptotic member of the B-cell lymphoma 2 (Bcl-2) protein family, which interacts with the anti-apoptotic proteins of the same family [B cell lymphoma-extra large (BCl-XL) and Bcl-2], inducing the apoptosis of the myeloma cells [52]. Bortezomib also inhibits osteoclasts and stimulates osteoblasts, thereby increasing bone formation [54].
What is MM ontogeny?
MM ontogeny is characterized by different stages of disease. The first stage, called monoclonal gammopathy of undetermined significance (MGUS), presents a low rate of plasma cell (PC) proliferation, low immunoglobulin burden and no clear related symptoms [21,22]. Patients with MGUS may develop MM, at a rate of 1% per year at 20 years [23]. In some patients, it is also possible to identify an intermediate stage classified as smoldering multiple myeloma (SMM), with higher immunoglobulin (Ig) burden but likewise asymptomatic [24]. When patients become symptomatic, the disease is referred to as MM, which may be either intramedullary or extramedullary [1,2]. The extramedullary disease is associated with a worse prognosis, mainly the widespread stage called plasma cell leukemia, in which we can find high levels of malignant PCs circulating in the peripheral blood [25,26].
What is the first oral PI approved for the treatment of relapsed and refractory MM?
Ixazomib is the first oral PI approved for the treatment of relapsed and refractory MM. As the other PIs, ixazomib promotes caspase-dependent induction of apoptosis and inhibition of cell cycle, inhibits the NF-κB pathway in MM cells and inhibits tumor-associated angiogenic activity [61]. The addition of ixazomib to lenalidomide and dexamethasone significantly increased the progression-free survival of patients treated with this regimen, when compared with those who received lenalidomide plus dexamethasone [62]. In NDMM patients, ixazomib also showed promising results, being effective and apparently well tolerated by these patients [63].
Which is better, thalidomide or lenalidomide?
Lenalidomide is more potent and effective than thalidomide in modulating the immune system [64]. The secretion of cytokines increases MM growth and survival, being associated with drug resistance [64,66]. Lenalidomide inhibits the production of pro-inflammatory cytokines such as IL-6, TNF-α, Interleukin-1 (IL-1) or Interleukin-12 (IL-12), and promotes the production of the anti-inflammatory cytokine IL-10 [64]. Like thalidomide , it inhibits the adhesion of MM to bone marrow stromal cells (BMSCs) and, consequently, decreases the production of IL-6 and downregulates TNF-α production (decreasing its levels up to 50,000 times more than thalidomide [64,65]. As thalidomide , it co-stimulates about 50 to 2000 times more T-cell proliferation triggered by the T cell receptor, increasing by 50 to 100 times the secretion of IFN-γ and IL-2 [64,65]. Besides the clonal production of both cytotoxic CD8+ and helper CD4+ T cells, lenalidomide also enhances natural killer (NK) cell activity against MM cells [64,65,73]. Lenalidomide blocks angiogenesis (being 2 to 3 times more potent than thalidomide as an antiangiogenic drug) by decreasing the angiogenic factors VEGF and IL-6 [64], and consequently inhibiting the development of blood vessels required for the growth of primary and metastatic tumors [65].
Does pomalidomide inhibit MM cells?
Like others IMIDs, pomalidomide acts by inhibiting MM cells proliferation and by inducing apoptosis. Likewise lenalidomide, it also enhances T-cell and NK cells activity, inhibits the production of pro-inflammatory cytokines and demonstrates anti-angiogenic activity, being also more potent than thalidomide. In order to produce its effects, it also requires the presence of cereblon in the MM cells [70,71,72,73,74]. Pomalidomide efficacy is higher when combined with dexamethasone or with PI combinations such as bortezomib. Nowadays, pomalidomide should be considered a beneficial treatment option for relapsed and refractory MM patients who received prior therapies that included bortezomib or lenalidomide [75,76,77].
What is multiple myeloma?
Multiple myeloma is a cancer of plasma cells. This disease can present a variety of challenges,...
Does alcohol help with multiple myeloma?
One explained, “I used to drink heavily. Upon diagnosis, I discovered that heavy alcohol use is NOT the best choice for someone diagnosed with multiple myeloma. It was enhancing all the negative results of multiple myeloma. I had to stop drinking. I did stop, and my life has been so much more satisfying.”
Does smoking cigarettes cause myeloma?
Research has also shown that smoking cigarettes can worsen the side effects of myeloma treatments like chemotherapy.
Can you drink alcohol while on chemotherapy?
For instance, drinking alcohol — even in moderation — can aggravate the mouth sores that result from chemotherapy and radiation therapy. Drinking alcohol may also put you at risk of dehydration or nutrient deficiency during cancer treatment. Because of these risks, your health care team may recommend that you avoid alcohol at certain points during your myeloma treatment.
Can you drink alcohol after a myeloma diagnosis?
Drinking Alcohol After a Myeloma Diagnosis. Despite a potentially decreased risk of developing myeloma with alcohol use, there are several reasons you may want to limit your alcohol intake or eliminate alcohol consumption if you already have myeloma.
Can alcohol cause myeloma?
Myeloma Lifestyle Changes: Drinking and Smoking Habits. There are limited and sometimes confusing findings on the connections between drinking alcohol and various types of cancer. However, alcohol can also interact with some drugs used during cancer treatment, which might increase the risk of harmful side effects.
Does alcohol affect chemotherapy?
Alcohol has been found to interfere with chemotherapy and potentially decrease its efficacy. That’s because alcohol and certain cancer drugs are processed in the liver. Alcohol can cause the organ to become inflamed. Inflammation of the liver can inhibit the breakdown of chemotherapy drugs and even worsen the side effects a person experiences during myeloma treatment.
What is the best treatment for myeloma?
Common combinations that we use are things like Revlimid® plus dexamethasone , or Velcade®, Revlimid, and dex. Many combinations of the most active therapies used for myeloma treatment include that dexamethasone.
How do steroids help myeloma?
The use of steroids improves the effectiveness of myeloma therapies. Consider reducing the steroid dose or stopping the use of steroids once a desirable outcome has been achieved. Discuss the use of steroids carefully with your doctor.
Should steroids be reduced?
Whenever there is a chance, and if it’s feasible, steroid dosage should be reduced. If feasible, even stopped, if an excellent response has been achieved. The BOTTOM LINE, in this case, is that you can see clearly that the use of steroids is something to discuss very carefully with your doctor.
Does dexamethasone cause side effects?
However, we know that dexamethasone has a lot of side effects. In some cases, for older patients or frail patients, the side effects could be so threatening that we decide that it’s not worth adding in the risks of steroid therapy to get some added benefit eventually. These side effects include things like increased risk of infection, ...
What is multiple myeloma?
Multiple myeloma is a cancer of plasma cells. This disease can present a variety of challenges,...
Does red wine help with myeloma?
In particular, red wine might be an optimal choice for this purpose. However, research shows that while light drinking might reduce myeloma risk, heavy alcohol use is linked to impaired immune function and increased susceptibility to infection, particularly bacterial pneumonia.
Can drinking alcohol cause myeloma?
People with myeloma are already producing fewer white blood cells, red blood cells, and platelets. Keep in mind that drinking heavily could put you at risk for several chronic conditions other than blood cancer. Generally, oncology professionals recommend being careful about your alcohol intake and having honest conversations with your doctors ...
Can alcohol affect myeloma?
Alcohol may also interact negatively with medications that you take during and after your myeloma treatments, and your health care team can help you understand whether this is a possibility with any drugs you’re taking.
Does alcohol cause multiple myeloma?
One 2013 study found that consuming alcohol may be associated with a lower risk of multiple myeloma. One possible reason alcohol might have this effect is because small to moderate consumption helps reduce factors that can prompt inflammation, according to the International Myeloma Foundation.
Can multiple myeloma take a toll?
Living with multiple myeloma (MM) and undergoing treatments can take a toll on a person’s outlook...
Does dexamethasone work better with bortezomib?
Dexamethasone allows us to have synergy between those drugs, the bortezomib (Velcade), the lenalidomide (Revlimid), things like that. And we know that all of these regimens work better with steroids on board. That being said, I can't think of anybody who loves taking 40 milligrams of dexamethasone.
Is dexamethasone good for myeloma?
Dexamethasone (Decadron) is a steroid, and it's a very effective drug against many immune cells. And myeloma is a cancer of immune cells, and so that' s why we use dexamethasone to treat myeloma. Now, there was a time where that was one of the most important drugs and one of the most used drugs, and I should say, one of the most effective drugs.
Which steroid is used to treat multiple myeloma?
These studies suggest that the particular combination of a proteasome inhibitor (like bortezomib or carfilzomib), an immunomodulating agent (like lenalidomide) and a steroid (like dexamethasone) may have enhanced activity against multiple myeloma, said Dr. Kazandjian.
What drugs are used for multiple myelom?
For example, in a single-arm phase II trial, Dr. Kazandjian and his colleagues found that treatment with lenalidomide, dexamethasone, and carfilzomib (Kyprolis ®) generated deep responses in patients with newly diagnosed multiple myeloma. And an ongoing phase III trial is comparing outcomes of patients treated with lenalidomide and dexamethasone plus either carfilzomib or bortezomib.
Why delay transplant?
But some transplant-eligible patients may opt to delay the procedure because of its potential toxicity and the risk of developing a second primary cancer, especially when highly efficacious drug regimens are becoming another option, explained Dr. Kazandjian. Previous early-stage clinical trials demonstrated the safety and efficacy ...
Can bortezomib be used for multiple myeloma?
For newly diagnosed patients with multiple myeloma who plan to delay autologous stem cell transplantation, adding the targeted therapy bortezomib (Velcade®) to a two-drug therapy improves how long they live compared with the doublet therapy alone, a new study has shown.
Can multiple myeloma patients have stem cells?
As part of first-line therapy, some patients with multiple myeloma may undergo a stem cell transplant. But because the procedure is time consuming and may cause serious side effects, patients may opt to delay it or to not have one at all. For patients who don’t intend to have a stem cell transplant immediately after diagnosis, ...
Does Bortezomib block proteasomes?
Bortezomib blocks the action of the proteasome (pictured above), a cellular complex that eliminates and recycles proteins that are damaged or no longer needed. For newly diagnosed patients with multiple myeloma who plan to delay autologous stem cell transplantation, adding the targeted therapy bortezomib ...
Does bortezomib cause nerve issues?
These side effects may be due to the intravenous delivery of bortezomib, which was standard at the time of the trial’s inception, the researchers wrote. Subcuta neous delivery of bortezomib, the current standard method, may reduce the incidence of nerve issues, they explained.
How to help people with multiple myeloma?
Tai chi and yoga are both gentle forms of exercise that may benefit people with multiple myeloma. Tai chi combines flowing movements with focused breathing. Yoga moves you through a series of poses. Research shows that both of these could reduce stress and anxiety, ease pain and fatigue, and improve sleep in people who have cancer.
How to help myeloma pain?
Massage therapy can relieve muscle pain and help you relax. Tell your massage therapist you have multiple myeloma and to use light touch to protect your bones, which may be weak.
What is complementary medicine?
The term “complementary and alternative medicine ” refers to treatments that are not part of standard medical care. They can include massage, acupuncture, tai chi, and herbal remedies. There’s some overlap between this term and naturopathy, homeopathy, and holistic medicine.
Does multiple myeloma have vitamin D?
People with multiple myeloma often have low levels of vitamin D. Healthy levels of this vitamin can protect you from bone complications that are common in this type of blood cancer.
Can multiple myeloma cause constipation?
Multiple myeloma and the treatments for it can cause pain, fatigue, constipation, loss of appetite, and other unpleasant symptoms. Complementary and alternative treatments may help you relieve these symptoms or ease the stress of living with cancer.
Can you have complementary treatments for multiple myeloma?
Before you try any complementary treatments for multiple myeloma, talk to your oncologist . They can tell you whether the therapy is safe for you, if it will interact with your cancer treatments, and if it’s likely to be effective.
Does acupuncture help with myeloma?
One study showed that acupuncture may help control nausea, appetite loss, and drowsiness and reduce the need for pain medicine after a stem cell transplant, a common myeloma treatment.