
Common Causes
What causes hematemesis? 1 Tears in the lining of your stomach from retching. 2 Irritation or loss of the lining of your stomach or esophagus. 3 Bleeding from varices in your stomach or intestine. 4 A tumor in your stomach or esophagus. 5 Radiation or a procedure such as endoscopy that damages your upper GI. 6 ... (more items)
Related Conditions
Medicine may be given to reduce the amount of acid your stomach produces. This may help if your hematemesis is caused by an ulcer. You may also need medicine to prevent blood flow to an injury or tear. Endoscopy may be used to treat the cause of your bleeding. Your healthcare provider may use heat to close a tear.
What are the causes of hematemesis?
Hematemesis, or vomiting blood, is a manifestation of upper gastrointestinal bleeding, that is, one that is located in the esophagus, stomach or duodenum.
What are the treatment options for hematemesis?
Hematemesis indicates that the bleeding is from the upper gastrointestinal tract, usually from the esophagus, stomach, or proximal duodenum. Occasionally hemoptysis or vomiting of swallowed blood from epistaxis can be confused with hematemesis.
What is haematemesis or vomiting blood?
What is the pathophysiology of hematemesis in epistaxis?
How can hematemesis be treated?
How is hematemesis treated?Medicine may be given to reduce the amount of acid your stomach produces. ... Endoscopy may be used to treat the cause of your bleeding. ... A blood transfusion may be needed if you lose a large amount of blood.An angiogram is done to look for and stop bleeding from an artery.More items...
How do you treat gastrointestinal bleeding?
How do doctors treat GI bleeding?inject medicines into the bleeding site.treat the bleeding site and surrounding tissue with a heat probe, an electric current, or a laser.close affected blood vessels with a band or clip.
How do doctors stop intestinal bleeding?
If you have an upper GI bleed, you might be given an IV drug known as a proton pump inhibitor (PPI) to suppress stomach acid production. Once the source of the bleeding is identified, your doctor will determine whether you need to continue taking a PPI .
What medication can cause gastrointestinal bleeding?
Drugs that can lead to gastrointestinal bleeding include non-steroidal anti-inflammatory drugs (NSAIDs) like diclofenac and ibuprofen, platelet inhibitors such as acetylsalicylic acid (ASS), clopidogrel and prasugrel, as well as anticoagulants like vitamin-K antagonists, heparin or direct oral anticoagulants (DOAKs).
How do you stop bleeding in the small intestine?
The small intestinal ulcers can be treated with endoscopic techniques or surgery in case of recurrent bleeding. Ulcers due to specific aetiology require treatment according to the aetiology. NSAIDs should be stopped in bleeding due to NSAID-induced ulcers.
Is GI bleeding curable?
Bleeding in the digestive tract is a symptom of a problem rather than a disease itself. It usually happens due to conditions that can be cured or controlled, such as hemorrhoids. The cause of the bleeding may not be serious, but it's important for your doctor to find the source of this symptom.
Can a CT scan show bleeding in the colon?
The use of computed tomography (CT) for evaluation of acute GI bleeding is gaining popularity because it can be used to rapidly diagnose active bleeding and nonbleeding bowel disease. The CT examinations used to evaluate acute GI bleeding include CT angiography and multiphase CT enterography.
What is a natural cure for gastrointestinal bleeding?
There is no home care for heavy gastrointestinal bleeding. Hemorrhoids or anal fissures may be treated with a diet high in fiber, fluids to keep stools soft may be helpful, and stool softeners if necessary. If they do not heal, they may need to have surgery to remove or fix them.
What causes internal bleeding in colon?
There are many possible causes of GI bleeding, including hemorrhoids, peptic ulcers, tears or inflammation in the esophagus, diverticulosis and diverticulitis, ulcerative colitis and Crohn's disease, colonic polyps, or cancer in the colon, stomach or esophagus.
Which drugs cause hematemesis?
Pill-induced esophagitis can cause hematemesis. Particular antibiotics (doxycycline, tetracycline, clindamycin), potassium chloride, bisphosphonates, and NSAIDs are often associated with pill-induced esophagitis.
How does aspirin stop stomach bleeding?
Omeprazole appears to be very effective in reducing both acute gastroduodenal mucosal damage and upper GI bleeding in the high-risk patient taking low-dose aspirin, but data with other anti-ulcer agents are lacking (misoprostol) or inconsistent (ranitidine) at present.
How is hematemesis diagnosed?
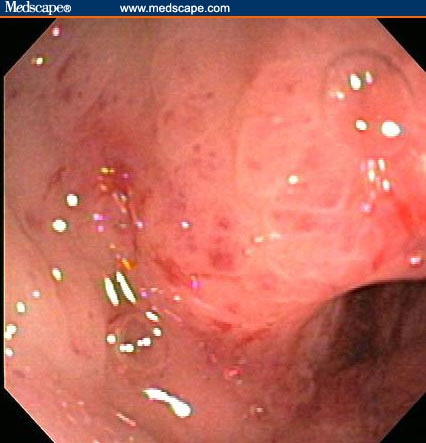
Upper endoscopy: Diagnostic test of choice for acute hematemesis due to the high sensitivity in ability to locate and treat specific locations of active bleeding lesions. Therapeutic endoscopy can be performed with esophageal variceal banding, clips, sclerosing agents, epinephrine injection, and thermocoagulation.
What is a bleed in the stomach called?
A bleeding stomach or duodenal ulcer. Irritation or swelling of the esophagus, called esophagitis. A benign (non-cancerous) or cancerous tumor in the stomach or esophagus. A severe injury to the abdominal area, as caused by a car accident or blow to the abdomen. An inflammation of the stomach, called gastritis.
What is the blood that causes vomiting?
What causes vomiting blood? Blood that is vomited usually comes from what is referred to as the upper GI, or gastrointestinal, tract. This includes the esophagus, stomach and duodenum (upper part of the small intestine).
What to do if you are vomiting blood?
If you are vomiting blood your medical team will first try to stabilize any low blood pressure, breathing problems or other complications of excessive blood loss. You may require a blood transfusion, breathing assistance and medication for your blood pressure or to lower stomach acid levels.
What does it mean when you vomit blood?
Vomiting blood, also called hematemesis, is a serious condition in which blood is expelled from the mouth. The blood can be bright red, black or dark brown. Conditions that cause a person to vomit blood can also cause blood to show up in the stool.
What tests are done to determine if a patient is vomiting blood?
Once a patient is stable, the cause of vomiting blood will be addressed. To determine the cause, several tests may be performed. These include: Blood tests to do complete blood count, check blood chemistry and clotting function. Liver function tests.
Can blood show up in stool?
Conditions that cause a person to vomit blood can also cause blood to show up in the stool. Vomiting blood does not refer to slight amounts of blood that might show up in your spit after brushing your teeth or after a nosebleed or a gum injury. (This is spitting up blood.)
What Causes Hematemesis?
Hematemesis is a sign of bleeding in your upper digestive tract. This includes the first part of your intestine, your stomach, or your esophagus. Your esophagus is the tube that connects your mouth to your stomach.
What Are Hematemesis Symptoms?
The main symptom of hematemesis is blood in your vomit. The blood and vomit can be:
How Is Hematemesis Diagnosed?
If you think you’re vomiting blood, you should go to a hospital right away. If you can, bring a small sample of it with you. Your doctor will need details about what the vomit looks like.
What Is the Treatment for Hematemesis?
True hematemesis is a medical emergency and can’t be treated at home. Your doctor will need to find the cause of your bleeding and stop it, then treat any underlying conditions. If you have only a little blood loss, they might give you medications and some fluids.
Is a Little Blood in Vomit Normal?
It’s common to have blood in your spit after brushing and flossing your teeth. You might also vomit swallowed blood after a nosebleed, but this isn’t hematemesis.
What is it called when you vomit blood?
What is Hematemesis ? Hematemesis or Vomiting blood is the regurgitation of stomach contents mixed with blood or the regurgitation of blood only. Vomiting blood can be caused for concern, but sometimes minor causes can trigger it. This includes ingestion of blood following an injury to the mouth or a nosebleed.
What is the test for vomiting blood?
A test called an esophagogastroduodenoscopy (EGD) to look for sources of bleeding in the upper digestive tract. Once the cause of the vomiting blood is determined, your doctor will determine the best treatment plan that will address both your symptoms and the underlying condition causing the vomiting.
What is the procedure to check for blood in the stomach?
Your doctor may order an upper endoscopy to look for blood in the stomach. This procedure is performed while you are sedated. Your doctor will place a small flexible tube called an endoscope in your mouth and your stomach and your small intestine.
What causes a swollen vein in the lower part of the esophagus?
This often occurs in people with severe liver damage, including people with long-term alcoholism. A serious injury to the abdominal area, caused by a car accident or a blow to the abdomen.
What is the name of the condition that affects an artery in the wall of the stomach?
Inflammation of the stomach called gastritis. Taking too much aspirin or nonsteroidal anti-inflammatory drugs. A condition called Dieulafoy's lesion, which affects an artery in the wall of the stomach. Inflammation of the small intestine called duodenitis.
What causes hematemesis in the stomach?
What causes hematemesis? Tears in the lining of your stomach from retching. Irritation or loss of the lining of your stomach or esophagus. Bleeding from varices in your stomach or intestine. A tumor in your stomach or esophagus. Radiation or a procedure such as endoscopy that damages your upper GI.
How to treat hematemesis?
You may also need medicine to prevent blood flow to an injury or tear. Endoscopy may be used to treat the cause of your bleeding. Your healthcare provider may use heat to close a tear.
What does it mean when you have a red bloody rash?
Hematemesis is the vomiting of blood. This is caused by bleeding in your upper gastrointestinal (GI) system. The blood may be bright red, or it may look like coffee grounds. Hematemesis is a medical emergency that needs immediate treatment.
What is the term for a procedure that damages the upper GI?
Radiation or a procedure such as endoscopy that damages your upper GI. A viral infection, hepatitis, or an H pylori infection. A condition such as gastroenteritis, gastritis, or a stomach ulcer. Use of medicines such as NSAIDs, aspirin, or blood thinners.
How to heal from vomiting?
Healthy foods can help you heal and improve your energy. Drink extra liquids as directed. You may need to drink extra liquids to prevent dehydration from vomiting. Ask your healthcare provider how much liquid to drink each day and which liquids are best for you.
Why do you need a blood transfusion?
A blood transfusion may be needed if you lose a large amount of blood. An angiogram is done to look for and stop bleeding from an artery. Contrast liquid is injected into an artery and x-rays of your blood flow are taken. Tell a healthcare provider if you have ever had an allergic reaction to contrast liquid.
What causes gastrointestinal hemorrhage?
Peptic ulcer, the most common cause of gastrointestinal hemorrhage, should be pursued through questions about epigastric distress, the relationship of symptoms to food intake, and a past history of peptic ulcer disease. Patients with liver disease may have varices, a source of bleeding.
What is hematochezia in a bowel?
Hematocheziais the passage of fresh blood per anus, usually in or with stools. Technique. Hematemesis, melena, and hematochezia are symptoms of acute gastrointestinal bleeding. Bleeding that brings the patient to the physician is a potential emergency and must be considered as such until its seriousness can be evaluated.
Why is my stool black?
If slow intestinal transit occurs, melenic stools may be due to bleeding from sites as distal as the cecum.
What is the difference between hematocezia and melena?
Melena is the passage of black, tarry stools. Hematochezia is the passage of fresh blood per anus, usually in or with stools. Hematemesis is the vomiting of blood, which may be obviously red or have an appearance similar to coffee grounds. Melena is the passage of black, tarry stools.
What causes melena in the stomach?
This makes the hypothesis untenable that melena is caused by the effect of gastric acid and pepsin on blood. Although melena usually means upper gastrointestinal hemorrhage, the small intestine and cecum should be studied if no cause for bleeding is found in the esophagus, stomach, or duodenum.
Is hematemesis a gastrointestinal bleeding?
Melena strongly suggests, and hematemesis confirms, that bleeding is of upper gastrointestinal origin. In this situation, seek historical evidence for common causes such as peptic ulcer, cirrhosis with esophageal or gastric varices, gastritis, esophagitis, Mallory–Weiss tears, and malignancy.
Is hematemesis a major hemorrhage?
The combination of hematemesis with melena, or red hematemesis alone, also suggests a major hemorrhage. Hematochezia, although it may be massive, usually presents as minor bleeding that is important because it may have come from a rectal or colonic neoplasm.
What to do if bleeding is not severe?
If your bleeding is not severe, you might start by seeing your primary care provider. Or you might be referred immediately to a specialist in gastrointestinal disorders (gastroenterologist). Here's some information to help you get ready for your appointment.
What is balloon assisted enteroscopy?
Balloon-assisted enteroscopy. A specialized scope inspects parts of your small intestine that other tests using an endoscope can't reach. Sometimes, the source of bleeding can be controlled or treated during this test. Angiography.
What tests are needed for occult bleeding?
Tests might include: Blood tests. You may need a complete blood count, a test to see how fast your blood clots, a platelet count and liver function tests. Stool tests. Analyzing your stool can help determine the cause of occult bleeding. Nasogastric lavage.
Can you take PPI if you have a bleed?
Once the source of the bleeding is identified, your doctor will determine whether you need to continue taking a PPI. Depending on the amount of blood loss and whether you continue to bleed, you might require fluids through a needle (IV) and, possibly, blood transfusions. If you take blood-thinning medications, including aspirin or nonsteroidal ...
Can a CT scan show a GI bleed?
A variety of other imaging tests, such as an abdominal CT scan, might be used to find the source of the bleed. If your GI bleeding is severe, and noninvasive tests can't find the source, you might need surgery so that doctors can view the entire small intestine. Fortunately, this is rare.
Does GI bleeding stop on its own?
Often, GI bleeding stops on its own. If it doesn't, treatment depends on where the bleed is from. In many cases, medication or a procedure to control the bleeding can be given during some tests.
How to treat inflamed colon?
If it’s caused by an allergy to a certain food or side effect from a drug, your doctor will recommend removing the food from your diet or changing medication. Most types of colitis are treated using medication and changes to diet.
What causes colitis in the body?
Infection. Viruses, bacteria, and parasites can cause infectious colitis. A person who has infectious colitis will have diarrhea and fever, and a stool sample that tests positive for enteropathogens such as: salmonella. campylobacter.
What is the term for the inflammation of the colon?
Colitis is a general term for the inflammation of the colon’s inner lining, which is your large intestine. There are different types of colitis categorized by cause. Infections, poor blood supply, and parasites can all cause an inflamed colon. If you have an inflamed colon, you’ll likely have abdominal pain, cramping, and diarrhea.
What side of the colon does ischemia affect?
Ischemic colitis can affect any part of your colon, but you usually feel pain on the left side of the abdomen. It can occur gradually or suddenly. Symptoms on your right side may indicate blocked arteries to your small intestine that can quickly cause necrosis of intestinal tissue.
What is the treatment for a bowel infection?
fever. unexplained weight loss. Treatment usually includes anti-inflammatory drugs, immunomodulators (drugs that affect the immune system), antibiotics, or biologics (engineered medicines that target certain proteins or genotypes that cause inflammation).
How to treat colitis?
Most types of colitis are treated using medication and changes to diet. The goal of treatment for colon inflammation is to reduce the inflammation-causing symptoms. Medications used to treat colitis may include: anti-inflammatory drugs, such as corticosteroids and aminosalicylates. immunosuppressants.
How to stop a swollen bowel?
keep track of and avoid foods that trigger or worsen your symptoms. consider eating smaller, more frequent meals throughout the day. avoid foods that increase stool output, such as caffeine and raw fruits and vegetables. consider limiting alcohol consumption.
