Symptoms
Rectal prolapse is usually caused by a weakening of the muscles that support the rectum. Symptoms of rectal prolapse include: Feeling a bulge after coughing, sneezing, or lifting Anyone can develop rectal prolapse, but women are more likely to have the condition than men.
Causes
If your rectal prolapse is very minor and it is caught early, your doctor might have you treat it by taking stool softeners to make it easier to go to the bathroom and by pushing the rectum’s tissue back up the anus by hand. But, typically, you will eventually need to have surgery to fix rectal prolapse.
Prevention
These are the two main types of complications: A rectal prolapse that can’t be pushed back into the rectum. This can cause the blood supply to the prolapse to be cut off. This complication is called strangulation. It’s painful and needs emergency treatment.
Complications
Throughout your life, this support structure can start to weaken. This can happen for a variety of reasons, but the result is a sagging of your organs. When your organs sag or droop out of their normal position, this is called a prolapse. Prolapses can be small—with just a little movement—or large. A small prolapse is called an incomplete prolapse.
What causes rectal prolapse in women?
How is rectal prolapse treated?
What are the complications of rectal prolapse?
What is an incomplete prolapse?
How to treat prolapsed anus?
However, surgery is usually necessary to repair the prolapse. There are several surgical approaches.
What causes rectum prolapse?
Other diseases, conditions and infections: Rectal prolapse can be a consequence of diabetes, cystic fibrosis, chronic obstructive pulmonary disease, hysterectomy, and infections in the intestines caused by parasites – such as pinworms and whipworms – and diseases resulting from poor nutrition or from difficulty digesting foods.
What is rectal prolapse?
Rectal prolapse occurs when the rectum (the last section of the large intestine) falls from its normal position within the pelvic area and sticks out through the anus. (The word "prolapse" means a falling down or slipping of a body part from its usual position.)
What is the term for a fall from the pelvic area?
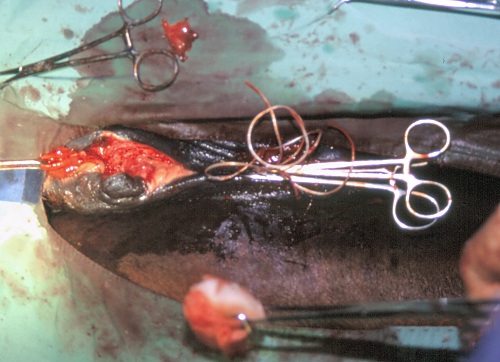
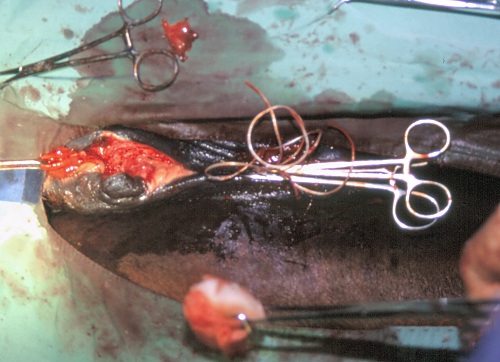
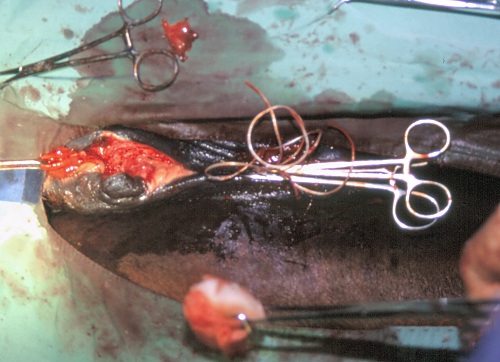
Rectal Prolapse. Rectal prolapse occurs when the rectum (the lower end of the large intestine) falls from its normal position within the pelvic area. In some cases of very minor, early prolapse, treatment can begin at home with the use of stool softeners. However, surgery will be necessary to repair the prolapse.
What are the risks of rectal prolapse surgery?
Other risks and complications from surgeries to repair rectal prolapse include: Lack of healing where the two ends of bowel reconnect. This can happen in a surgery in which a segment of the bowel is removed and the two ends of the remaining bowel are reconnected. Intra-abdominal or rectal bleeding.
What are the conditions that can be present with rectal prolapse?
Other conditions, such as urinary incontinence, bladder prolapse and vaginal/uterine prolapse , could be present along with rectal prolapse. Because of the variety of potential problems, urologists, urogynecologists and other specialists often team together to share evaluations and make joint treatment decisions.
How long does it take to recover from a prolapse?
Complete recovery can usually be expected in a month; however, patients should avoid straining and heavy lifting for at least 6 months. In fact, the best chance for preventing prolapse from returning is to make a lifetime effort to avoid straining and any activities that increase abdominal pressure.
How does rectum prolapse happen?
Prolapse occurs when the rectum becomes unattached inside the body and comes out through the anus, effectively turning itself inside out. Rectal prolapse is a relatively rare condition, with the American Society of Colon and Rectal Surgeons estimating that it affects less than 3 in every 100,000 people.
What happens if you have a rectal prolapse?
Complications include: Strangulated prolapse: This occurs when part of rectum becomes trapped and cuts off the blood supply, causing tissue to die. This can develop gangrene, and the area will turn black and drop off.
What is the difference between a rectal prolapse and a hemorrhoids?
While rectal prolapse affects the rectal wall, hemorrhoids affect the blood vessels in the anal canal.
How many types of rectal prolapse are there?
There are three types of rectal prolapse:
What to do if you have a bowel problem?
In the first instance, it is important to relieve the symptoms and allow easier bowel movements. Doctors may recommend a high fiber diet, stool softeners, and bowel training, as well as drinking plenty of water.
How long does it take to recover from a rectal prolapse?
Typically, people who have had surgery spend 3 to 5 days in the hospital after the operation, and most make a complete recovery within 3 months. After undergoing surgery for a rectal prolapse, people should avoid straining and heavy lifting for at least 6 months afterward. Last medically reviewed on November 11, 2017.
Can you push a prolapsed anus back?
Over time, however, the prolapse is likely to protrude permanently, and a person will be unable to push the prolapse back.
What are the risks of rectal prolapse?
These are some conditions that may increase your risk for developing a rectal prolapse: A long history of constipation. Straining to have bowel movements. Chronic diarrhea.
How to diagnose rectal prolapse?
Your healthcare provider will be able to diagnose rectal prolapse with a medical history and a physical exam. You may be asked to squat and strain as if you are having a bowel movement. Your healthcare providers may also do other tests to confirm the diagnosis. Tests may include:
How to tell if you have a prolapsed rectum?
Having mucous discharge in your stool. Pain and rectal bleeding. Fecal incontinence. Having to push the prolapse back into the anus by hand. Feeling pressure in your rectum. Being constipated.
What to do after rectal prolapse surgery?
If you are recovering from rectal prolapse surgery, make sure to take your pain medicine as directed by your healthcare provider. Finish all antibiotics and don’t take any over-the-counter medicine without talking with your surgeon.
Why does my anus leak?
Fluid, mucus, and blood can leak from the anus, too. Causes of anal leakage include: Diarrhea: Often caused by bacteria or an infection such as norovirus, gastroenteritis, food poisoning, and other infections in the digestive system.
What percentage of women have anal leakage?
One study found that 19 percent of surveyed women reported an episode of anal leakage. This number is much higher than what has been previously reported. Anal leakage can affect men and women, particularly women after childbirth.
Why does my rectum stiffen?
Rectal stiffening can be caused by rectal surgery, inflammatory bowel disease, and radiation damage. Rectal prolapse: If the rectum can no longer be well supported by surrounding muscles it can protrude through the anus. In rectal prolapse, fluid can leak out through the protruding rectum.
What causes nerve damage in the rectum?
Types of nerve damage include diabetic neuropathy, spinal cord injury, stroke, and multiple sclerosis. Nerve damage can also be a result of straining when pushing out bowels and during childbirth. Rectal stiffening: If the rectum becomes diseased, then its ability to stretch and hold stool becomes impaired.
Why does my sphincter leak out?
If these muscles are sick or unable to contract fully, stool can leak out. Muscle weakness can be caused by hemorrhoids, childbirth , certain muscular disease, and some surgeries.
Can fluid leak out of the rectum?
In rectal prolapse, fluid can leak out through the protruding rectum. Anal cancer: Anal cancer damages the nerves and muscles of the anus, impairing the function of the anal sphincter. Blood may be present in the leakage. Anal cancer is a life-threatening condition.
Can anal leakage be left untreated?
Your doctor will be able to recommend the most suitable option for your particular case. The longer anal leakage is left untreated, the higher the risk of complications. Speak to your doctor about this problem to obtain treatment.
How to tell if you have rectal prolapse?
If you have rectal prolapse, you may notice a reddish mass that comes out of the anus, often while straining during a bowel movement. The mass may slip back inside the anus, or it may remain visible. Other symptoms may include: The inability to control bowel movements (fecal incontinence) Constipation or diarrhea.
What age is rectal prolapse more common?
Age. Rectal prolapse is more common in people over age 50.
What is the term for a rectum that protrudes from the anus?
Rectal prolapse. Rectal prolapse. Rectal prolapse occurs when the rectum becomes stretched and protrudes from the anus. Rectal prolapse occurs when part of the large intestine's lowest section (rectum) slips outside the muscular opening at the end of the digestive tract (anus).
Can rectal prolapse be treated with stool softeners?
While rectal prolapse may cause discomfort, it's rarely a medical emergency. Rectal prolapse can sometimes be treated with stool softeners, suppositories and other medications . But surgery is usually needed to treat rectal prolapse.
Why does my rectum prolapse?
Chronic constipation. The strain of chronic bowel movement problems can make your rectum more likely to move down from its location. Strain while having bowel movements, if done often over a period of years, can also cause rectal prolapse.
How to prevent rectal prolapse?
Preventing rectal prolapse isn’t always possible. You can reduce your risk if you maintain good intestinal health. To help avoid constipation, in particular: 1 make high-fiber foods part of your regular diet, including fruits, vegetables, bran, and beans 2 reduce the amount of processed food in your diet 3 drink plenty of water and fluids every day 4 exercise most, if not all, days of the week 5 manage your stress with meditation or other relaxation techniques
What percentage of people with rectal prolapse have diarrhea?
Chronic constipation occurs in 30 to 67 percent of people with rectal prolapse, and about 15 percent experience diarrhea.
How long does it take for rectum prolapse to get better?
Rectal prolapse won’t get better on its own. The degree of prolapse will increase over time. This process can take months or years , so there isn’t always a rush to make a decision.
How long does it take to recover from rectum prolapse?
A full recovery can be expected in about six weeks. Rectal prolapse can be uncomfortable and painful, but it’s treatable. The sooner you see a doctor about your symptoms, the easier the surgery and recovery.
How many people have rectum prolapse?
Rectal prolapse affects about 2.5 people out of 100,000. Women over 50 are six times more likely than men to have this condition. It’s often suspected when the problem is actually a serious case of hemorrhoids. Rectal prolapse can range from mild to severe. Mild cases can often be treated without surgery.
What age is the most likely to develop rectal prolapse?
Women over age 50 are also at an increased risk of rectal prolapse.
How to prevent prolapse?
Don’t lift alone: When you have something that’s oddly shaped or very large, get help lifting it. Also, avoid lifting something above waist level. Check your footing: Make sure you have a good footing before lifting something.
What is a prolapse in the vagina?
Vaginal Prolapse. Vaginal prolapse is a condition where the vagina slips out of position. This is more common in women who have had multiple vaginal deliveries during childbirth, have gone through menopause, are smokers or are overweight. The chances of developing a prolapse also increases as you age.
How to diagnose vaginal prolapse?
A vaginal prolapse is often diagnosed in your healthcare provider’s office during an appointment. Your provider will do a physical exam, talk to you about any symptoms of fullness in your pelvic area or urinary incontinence (leakage). You may also be asked about your family history and about any previous pregnancies.
Why does my vagina slip out of place?
When that happens, the vagina might slip down out of place, causing a prolapse. Several common causes of a vaginal prolapse can include: Childbirth: Vaginal delivery raises the risk of prolapse more than a cesarean section (when the baby is delivered through a surgical opening in the wall of the abdomen).
What is the name of the organ that droops down into the vagina?
The different types of pelvic organ prolapse can include: Vaginal vault prolapse: The top of the vagina (known as the “vaginal vault ”) droops down into the vaginal canal.
Is there a surgical treatment for vaginal prolapse?
There are non-surgical and surgical treatment options for vaginal prolapses. These treatments are very similar to treatment options for uterine prolapses. There are a few things your healthcare provider will take into account when forming a treatment plan.
Can you feel a prolapse?
In many cases, you may not feel any symptoms from a prolapse. You may find out about a vaginal prolapse during an exam in your healthcare provider’s office. If you do experience symptoms, they can include:
Diagnosis
Sometimes it can be difficult to distinguish rectal prolapse from hemorrhoids. To help diagnose rectal prolapse and rule out other associated conditions, your doctor may recommend:
Treatment
Treatment for rectal prolapse usually involves surgery. Other treatments include various therapies for constipation, including stool softeners, suppositories and other medications. There are a few different surgical methods for treating rectal prolapse.
What causes rectal prolapse?
Anything that increases the pressure inside your tummy (abdomen) can make you more likely to develop a rectal prolapse. This can include:
When to use surgery for prolapse?
Surgery may also be used where the prolapse keeps coming back, becomes painful or where ulcers or bleeding develop .
What are the treatment options for rectal prolapse?
If doing this is painful, a doctor may be required to do this after giving you a sedative and a local anaesthetic injection to numb the area.
What is the outlook for rectal surgery?
The outlook (prognosis) will depend on your age, on whether you have any untreatable causes for the prolapse and on the state of your general health.
What causes poo to get stuck in the bowel?
Hirschsprung's disease (a rare condition that can cause poo to become stuck in the bowel).
How to get a child to stop prolapse?
In children, the prolapse can usually be gently pushed back using a lubricant gel. You need to make sure your child has a high-fibre diet and doesn't strain when they go to the loo. Sometimes a laxative is required. Very occasionally an injection that shrinks tissue (a sclerosant) has to be given.
What causes nerve damage in the pelvic region?
Damage to the nerves from back surgery, a slipped disc, or an accident injuring the pelvic nerves.
Symptoms
Risk Factors
Diagnosis
Treatment
Complications
When to Call The Healthcare Provider
Managing Rectal Prolapse