Procedures
Are esophageal varices fully curable? Initial treatment of bleeding esophageal varices is effective in 80 to 90% of cases but mortality remains approximately 15 to 20%, with the majority of deaths due to liver failure, hepatorenal syndrome, and infections, and occurring predominantly in Child class C cirrhotic patients.
Self-care
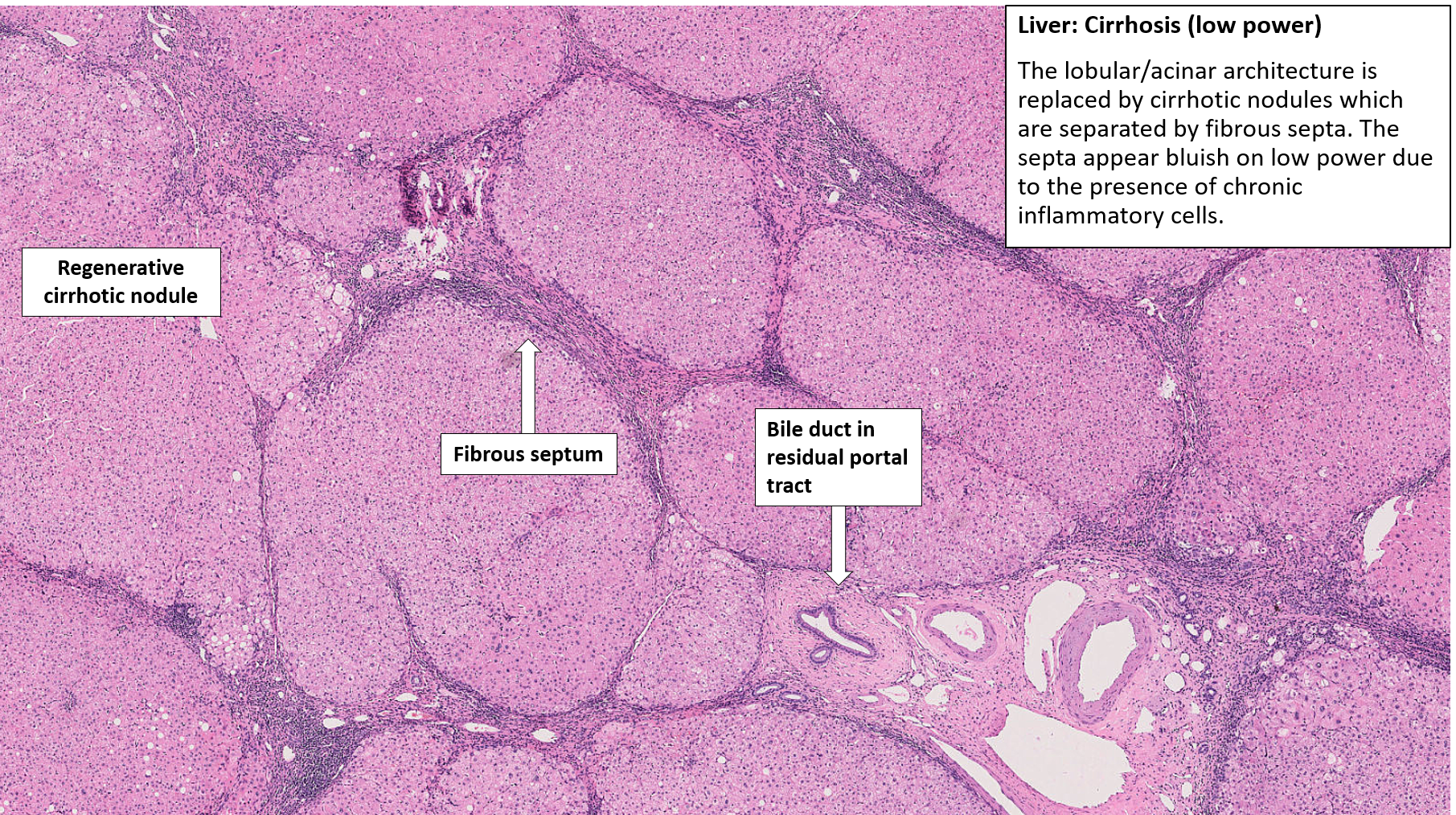
Causes of esophageal varices include: Severe liver scarring (cirrhosis). A number of liver diseases — including hepatitis infection, alcoholic liver disease, fatty liver disease and a bile duct disorder called primary biliary cirrhosis — can result in cirrhosis. Blood clot (thrombosis). A blood clot in the portal vein or in a vein that ...
See more
Technically varicose veins cannot be permanently cured as the condition that causes them – Chronic Venous Insufficiency (CVI) results in permanent damage to the valves which control the flow of blood back to the heart and lungs. Currently, there is no way to repair the vein using a microscopic scalpel. Are esophageal varices reversible?
Are esophageal varices fully curable?
What You Should Know About Bleeding Esophageal Varices
- Diagnosis. To diagnose esophageal varices, a doctor or other healthcare professional (HCP) will perform a physical examination and ask you about your symptoms.
- Treatment options. The main goal of treatment is to prevent esophageal varices from rupturing and bleeding. ...
- Long-term outlook for people with bleeding esophageal varices. ...
What causes esophageal varices treatment?
Will esophageal varices go away?
What is the treatment for bleeding esophageal varices?
What Are Esophageal Varices?
Varices are veins that are enlarged or swollen. The esophagus is the tube that connects the throat to the stomach. When enlarged veins occur on the...
Who Is at Risk For Esophageal Varices That Break Open and Bleed?
Not everyone who develops esophageal varices will have bleeding. Factors that increase the risk for bleeding include: 1. High portal blood pressure...
What Causes Esophageal Varices?
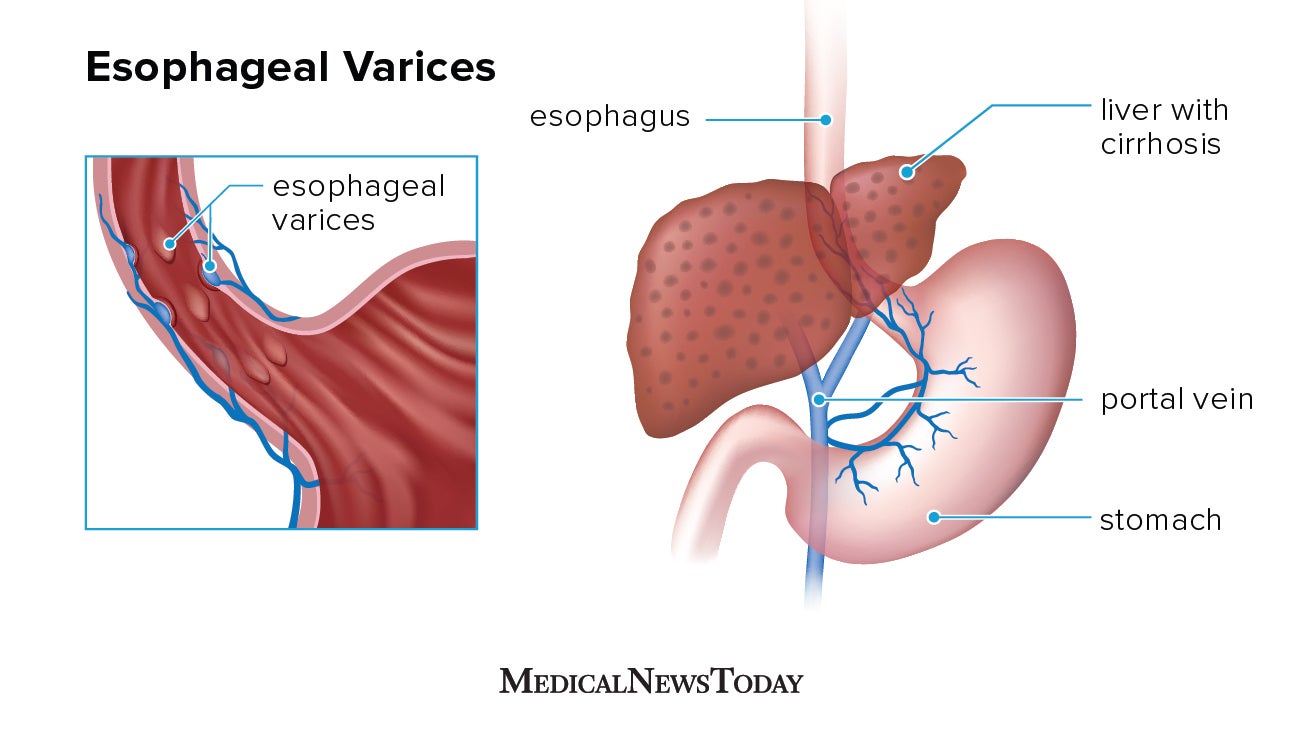
The liver is the organ that cleanses toxins from the blood. The portal vein delivers blood to the liver. Esophageal varices usually occur in people...
What Liver Conditions Can Lead to Esophageal Varices?
Any type of serious liver disease can cause esophageal varices. Cirrhosis is the most common type of liver disease, and more than 90% of these pati...
What Are The Symptoms of Esophageal Varices?
Most people do not know they have esophageal varices until the varices start to bleed. When bleeding is sudden and severe, the person vomits large...
How to reduce veins in legs?
These treatments can reduce their appearance and relieve discomfort: Elevation: To increase blood flow and decrease pressure in the veins, you should elevate your legs above your waist several times throughout the day. Elastic stockings: Supportive stock ings or socks compress the veins and reduce discomfort.
Where do varicose veins develop?
Most often, varicose veins develop on the lower half of the body, usually on the calves, ankles and feet. They can also develop in the pelvic area (pelvic congestion syndrome), especially in women who have had children. Varicose veins in the testicles ( varicocele) can lead to infertility in men.
What is the difference between spider veins and varicose veins?
What is the difference between varicose veins and spider veins? Varicose veins and spider veins are both types of venous disease, but they look different. Spider veins are smaller and thinner than varicose veins. They look like a red or blue spider webs or branches of a tree, and they are close to the skin’s surface.
How to tell if you have varicose veins?
The most recognizable sign of varicose veins is a gnarled, blue or purple vein just under the skin’s surface. Symptoms include: Bulging veins: Twisted, swollen, rope-like veins are often blue or purple. They appear just below the surface of the skin on the legs, ankles and feet. They can develop in clusters.
Why do veins get bigger?
Varicose veins occur when the walls of veins become weakened. As blood pressure in the vein increases, the weakened walls allow the vein to get bigger. As the vein stretches, the valves in the vein can’t work like they should. Sluggish blood backs up or pools in the vein, causing the vein to swell, bulge and twist.
What are purple veins?
Varicose Veins. Varicose veins are twisted, blue or purple veins that bulge under the skin’s surface. They don’t usually cause serious health problems. If veins are painful or bleeding, or if the area is swollen, see your healthcare provider.
What is the procedure called when you strip a vein?
Vein surgery: During these procedures, also called ligation and stripping, the surgeon ties off the affected vein (ligation) to stop blood from pooling. The surgeon may remove (strip) the vein to prevent varicose veins from reappearing.
How to stop bleeding from esophageal varices?
Doctors are exploring an experimental emergency therapy to stop bleeding from esophageal varices that involves spraying an adhesive powder. The hemostatic powder is administered through a catheter during an endoscopy. When sprayed on the esophagus, hemostatic powder sticks to the varices and may stop bleeding.
What is the procedure called to check for varices in the esophagus?
A procedure called upper gastrointestinal endoscopy is the preferred method of screening for esophageal varices. Your doctor inserts a thin, flexible, lighted tube (endoscope) through your mouth and into your esophagus, stomach and the beginning of your small intestine (duodenum).
What to do if you have internal bleeding?
If you're having signs and symptoms of internal bleeding, call 911 or your local emergency number to be taken to the hospital for urgent care.
What is the best treatment for portal vein bleed?
These medications include propranolol (Inderal, Innopran XL) and nadolol (Corgard).
Can you get an antibiotic for a bleed?
There is an increased risk of infection with bleeding, so you'll likely be given an antibiotic to prevent infection . Replacing the diseased liver with a healthy one. Liver transplant is an option for people with severe liver disease or those who experience recurrent bleeding of esophageal varices.
Can esophageal varices bleed?
There is a high risk that bleeding will recur in people who've had bleeding from esophageal varices. Beta blockers and endoscopic band ligation are the recommended treatments to help prevent re-bleeding.
Why do varices bleed?
Varices also can develop in the small blood vessels in the upper part of the stomach. If the pressure caused by the extra blood gets too high, varices can break open and bleed. Bleeding is an emergency that requires urgent treatment.
What is a varices in the esophagus?
Esophageal varices are enlarged or swollen veins on the lining of the esophagus. Varices can be life-threatening if they break open and bleed. Treatment is aimed at preventing liver damage, preventing varices from bleeding, and controlling bleeding if it occurs.
What is esophageal varices?
What are esophageal varices? Varices are veins that are enlarged or swollen. The esophagus is the tube that connects the throat to the stomach. When enlarged veins occur on the lining of the esophagus, they are called esophageal varices. Cleveland Clinic is a non-profit academic medical center.
Which organ is responsible for removing toxins from the blood?
The liver is the organ that cleanses toxins (poisons) from the blood. The portal vein delivers blood to the liver. Esophageal varices usually occur in people who have liver disease. Blood flow through the liver slows in people who have liver disease. When this happens, the pressure in the portal vein goes up.
Can esophageal varices cause bleeding?
Not everyone who develops esophageal varices will have bleeding. Factors that increase the risk for bleeding include: High portal blood pressure: The higher the portal pressure, the greater the risk of bleeding. Large varices: Risk of bleeding increases with size of varices. Severe liver disease: Advanced cirrhosis or liver failure increases ...
Does TIPS help with bleeding?
This reduces the pressure in the portal vein, which reduces the pressure in the varices, which reduces their risk of bleeding. TIPS can be very effective in preventing bleeding , but it also can cause serious complications, particularly in patients with advanced liver disease, including confusion and liver failure.
Is esophageal varices life threatening?
Bleeding esophageal varices is life-threatening condition and can be fatal in up to 50% of patients. People who have had an episode of bleeding esophageal varices are at risk for bleeding again. Treatment with variceal ligation is effective in controlling first-time bleeding episodes in about 90% of patients.
What is the treatment for spider veins?
Laser treatment. Laser energy is used to scar and destroy varicose veins. This is called ablation. Simple laser therapy is done on small veins close to the skin, such as spider veins. The laser is used outside of your skin. Endovenous laser therapy uses a laser fiber inserted into the vein.
Why do you inject a chemical into a vein?
A chemical is injected into a varicose vein to damage and scar the inside lining of the vein, causing the vein to close. This usually works best for small veins.
What causes varices in the stomach?
Varices are dilated veins in the distal esophagus or proximal stomach caused by elevated pressure in the portal venous system, typically from cirrhosis. They may bleed massively but cause no other symptoms. Diagnosis is by upper endoscopy. Treatment is primarily with endoscopic banding and IV octreotide.
How long does it take for variceal bleeding to recur?
Endoscopy is done for diagnosis and treatment; banding or sclerotherapy can be used. Recurrence rate of variceal bleeding is 50 to 75% within 1 to 2 years.
What antibiotics are used for cirrhosis?
Patients with known cirrhosis with GI bleeding are at risk of bacterial infection and should receive antibiotic prophylaxis with norfloxacin or ceftriaxone. Because varices are invariably diagnosed during endoscopy, primary treatment is endoscopic. Endoscopic banding of varices is preferred over injection sclerotherapy.
How to treat gastric varices?
Blood transfusions are often needed to replace the blood being lost from the bleeding varices. Endoscopic variceal ligation is the most common technique used when treating gastric varices.
What is the procedure to diagnose gastric varices?
Diagnosing gastric varices often requires an endoscopy for confirmation. An endoscopy is an imaging procedure, similar to an ultrasound, that allows a doctor to view the inside of your digestive tract.
What happens if your varices burst?
If the varices burst, the internal bleeding they cause can become life-threatening. The internal bleeding from gastric varices causes patients to cough up blood, vomit blood, have bloody or black and tarry stools, and eventually dizziness and shock.
What causes gastric varices?
Gastric varices are a pathological condition caused by liver dysfunction, most often cirrhosis of the liver, resulting in portal hypertension. Portal hypertension occurs when there is increased pressure in the portal veins of the liver. These veins are how blood reaches the liver and the spleen.
Why do portal veins swell?
Portal hypertension forces blood from the portal veins into smaller blood vessels in the stomach area that are unable to handle the additional amounts of blood, causing them to swell and sometimes burst. Before they rupture, gastric varices are asymptomatic.
What is the treatment for a vein clot?
Sclerotherapy is also a treatment option, where certain medicines are injected directly into the veins, causing them to shrink. Alternatively, endoscopic injections can be used to place tissue adhesives at the site of bleeding, forcing the tissues to clot and control the bleeding.
Can gastric varices bleed?
As the veins are swollen, the vein walls are much thinner and more susceptible to rupturing than normal. If they remain unbroken, gastric varices show no symptoms. Once they start to bleed, varices can result in any number of the following symptoms.
What is the best treatment for bleeding varices?
Aside from the urgent need to stop the bleeding, treatment is also aimed at preventing more bleeding. Procedures that help treat bleeding varices include: Banding.
What is the procedure to remove varices?
A surgical procedure that removes the bleeding varices. This procedure is done when a TIPS or a surgical shunt isn't possible or unsuccessful in controlling the bleeding. Esophageal transection. A surgical procedure in which the esophagus is cut through and then stapled back together after the varicies have been tied off.
What is the procedure to stop bleeding from varices?
A gastroenterologist places small rubber bands directly over the varices. This will stop the bleeding and get rid of the varices. Sclerotherapy. A gastroenterologist directly injects the varices with a blood-clotting solution instead of banding them. Transjugular Intrahepatic Portosystemic Shunt (TIPS).
What is varices in 2021?
Medically Reviewed by Carol DerSarkissian, MD on March 08, 2021. Varices are dilated blood vessels in the esophagus or stomach caused by portal hypertension. They cause no symptoms unless they rupture and bleed, which can be life-threatening. Someone with symptoms of bleeding varices should seek treatment immediately.
What are the symptoms of varices?
Symptoms include: Vomiting of blood. Black, tarry, or bloody stool. Low blood pressure. Rapid heart rate. Lightheadedness. Shock (in severe cases) Bleeding from varices is a medical emergency. If the bleeding is not controlled quickly, a person may go into shock or die.
What is the best treatment for liver disease?
Earlier treatment of liver disease may prevent them from developing. Certain medications, including the class of heart drugs called "beta-blockers," may reduce elevated portal pressure and lower the likelihood of bleeding. Long-acting nitroglycerines are also used for this purpose.
Where are varices located?
This leads to the development of large, swollen veins (varices) within the esophagus, stomach, rectum, and umbilical area (around the belly button). The varices are fragile and can rupture easily, resulting in a large amount of blood loss.
Is gastric varices more common than esophageal varices?
Gastric varices are less common than esophageal varices, and their treatment is quite challenging. Gastric varix bleedings (GVB) occur less frequently than esophageal varix (EV) bleedings and represent 10% to 30% of all variceal bleedings. They are; however, more severe and are associated with high …. Current Approaches to the Treatment of Gastric ...
Is GV bleeding more severe than esophageal varices?
Re-bleeding may occur in 35% to 90% of cases after spontaneous hemostasis. GV bleedings represent a serious clinical problem compared with esophageal varices due to their location. Sclerotherapy and band ligation, in particular, are less effective.
What are gastrointestinal varices?
Gastrointestinal varices are abnormally dilated submucosal veins in the digestive tract due to portal hypertension and can potentially cause life-threatening bleeding. Prevalence of varices increases with the severity of liver disease (Child-Pugh class A 42.7%, class B 70.7% and class C 75.5%) [ 2, 10 ]. The Child-Pugh score is described in Table#N# Table1.#N#1. The incidence of esophageal varices in cirrhotic patients is around 5% at the end of one year and 28% at the end of three years. Small varices progress to large varices at a rate of 10% to 12% annually [ 11 ]. Approximately 50% of all patients with a new diagnosis of cirrhosis have gastrointestinal varices [ 2 ]. Annual risk of variceal bleeding among small and large varices is 5% and 15% respectively [ 12 ]. The six-week mortality rate among patients with index variceal bleeding is approximately 20% [ 13 ]. Risk of rebleeding without endoscopic intervention is almost 60% with an increased mortality rate (33%) [ 14 ].
What is the gold standard procedure for gastroesophageal varices?
Esophago-gastro duodenoscopy (EGD) is the gold standard procedure used in the diagnosis of gastroesophageal varices (GOVs). Based on the endoscopic assessment, GOVs are classified into small (< 5 mm), and large varices (> 5 mm) [ 38] for clinical management. Disadvantages of endoscopy include the risk of sedation, higher cost, bleeding and risk of aspiration.
What percentage of patients with cirrhosis have duodenal varices?
According to one estimate, among patients with cirrhosis and portal hypertension who underwent angiography, 40% of patients had duodenal varices. Ectopic varices are responsible for up to 1%-5% of all variceal bleeding.
Where do stoma varices occur?
Stomal varices. Stomal varices usually occur at the mucocutaneous junction of the stoma, due to portosystemic shunt between the portal circulation of the bowel and systemic circulation of the abdominal wall. Diagnosis of stomal varices is difficult, on physical exam, they appear as bluish discoloration of the skin.
Is EVL a sclerotherapy?
Currently, EVL is considered to be the first line of endoscopic treatment for the management of bleeding esophageal varices. EVL has better hemostasis, a lower rate of side effects (ulcer, stricture), a reduced rate of early rebleeding, and a lower rate of early mortality compared to sclerotherapy.
Diagnosis
Lifestyle and Home Remedies
Alternative Medicine
Preparing For Your Appointment