
Therapy
- Disruptive behavior disorder;
- Depression;
- Anxiety; and
- PTSD.
Self-care
Medication: Although there is no medication formally approved to treat conduct disorder, various drugs may be used (off label) to treat some of its distressing symptoms (impulsivity, aggression ...
What is the best therapy for conduct disorder?
The most widely used and accepted form of therapy for Co-occurring disorders is behavioral therapy. Cognitive-behavioral therapy (CBT) and Dialectical-behavioral therapy (DBT) are the most renowned. The National Institute on Drug Abuse lists several forms of behavioral therapy helpful to Co-occurring disorders.
Is there a cure for conduct disorder?
Life expectancy is not affected by oppositional defiant disorder. The affected person may have suicidal tendencies. As discussed above, oppositional defiant disorder is a risk factor for the development of conduct disorder (CD). The diagnostic criteria of conduct disorder are more severe than the criteria linked with oppositional defiant disorder.
How to best treat co-occurring disorders?
Is conduct disorder a lifelong disorder?
See more
What are the treatments for conduct disorder?
Treatment for conduct disorder may include:Cognitive-behavioral therapy. A child learns how to better solve problems, communicate, and handle stress. ... Family therapy. This therapy helps make changes in the family. ... Peer group therapy. A child develops better social and interpersonal skills.Medicines.
What is the best form of treatment for a conduct disorder?
Treatment for conduct disorder may include: Multisystemic therapy: Intensive, often home- or community-based interventions to promote positive behavior change in the youth's environment. Treatment relies heavily on family and school involvement. Family therapy.
What medication is used for conduct disorder?
STIMULANTS. Dextroamphetamine (Dexedrine) and methylphenidate (Ritalin) are the most promising agents used in the treatment of conduct disorder.
How is conduct disorder treated in adults?
Family therapy, multi-systemic therapy, and cognitive behavioral treatment (CBT) have been found to be an effective treatment for conduct disorder.
How can you help students with conduct disorder?
Try to monitor your expressions, keep them as neutral as possible, communicate a positive regard for the students, and give them the benefit of the doubt whenever possible. Remember that students with conduct disorder like to argue. Remain respectful, calm, and detached. Avoid power struggles and don't argue.
How does CBT help conduct disorder?
CBT is another well-studied psychosocial treatment for anger and aggression in children and adolescents. During CBT, children learn how to regulate their frustration, improve their social problem-solving skills, and role-play assertive behaviors that can be used during conflicts instead of aggression.
How do you treat behavioral problems in children?
Parent behavior therapy has the strongest evidence as an effective treatment for disruptive behavior problems in children. Other approaches like client-centered therapy or play therapy did not have enough studies or strong enough evidence of effectiveness to receive a high rating.
Is conduct disorder a disability?
“Disability” can include behavioral and other mental health disorders, such as depression, anxiety disorder, obsessive-compulsive disorder, phobias, or conduct disorder, to the extent that it interferes with the child's ability to thrive at school.
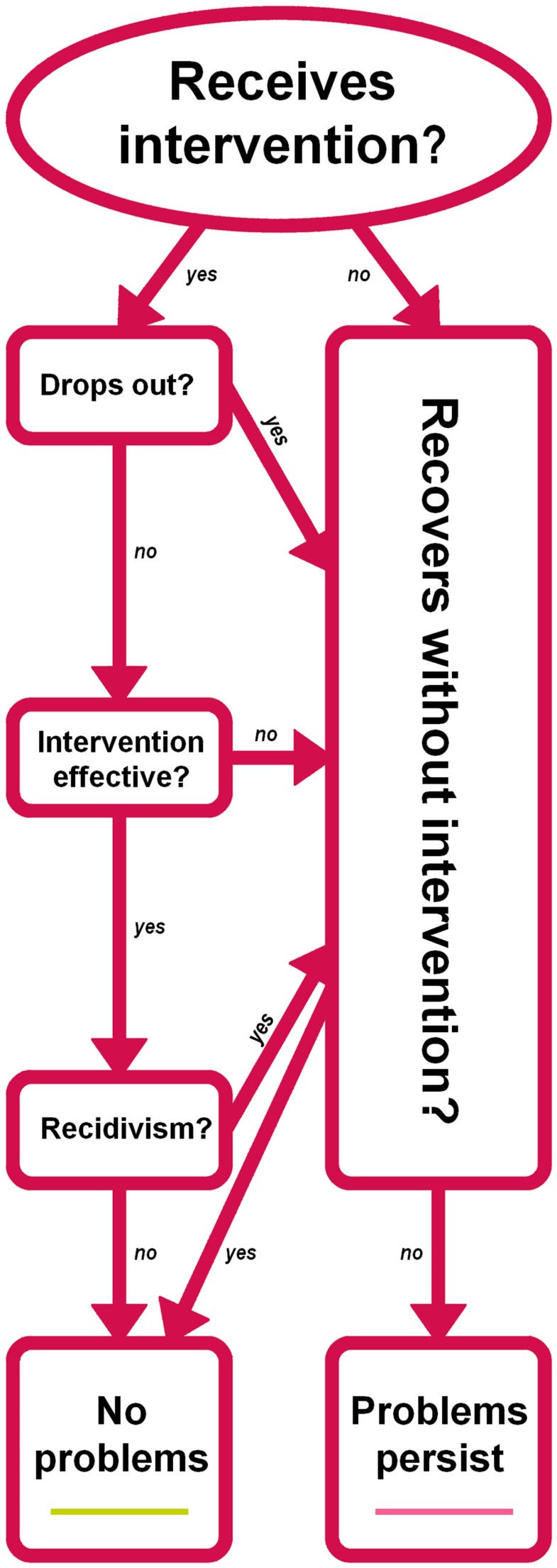
Can you grow out of conduct disorder?
The majority of children, about 70%, who do display symptoms of conduct disorder will grow out of it by adolescence. The children that do not grow out of it and progress on to adolescence have a poorer prognosis than those with the adolescent-onset type.
What are the best interventions for conduct disorder?
The most common interventions for this disorder include cognitive behavioral therapy, behavior therapy, and pharmacotherapy.
What are the interventions used to treat conduct disorder?
Psychosocial Interventions. Psychosocial interventions that are commonly used to treat conduct disorder include medication. These medications help a child or adult suffering from this disorder to control their symptoms, and reduce the number of instances in which they engage in unruly or violent behavior.
How to treat ADHD in children?
While early and mild cases of ADHD can be effectively managed through regular checkups by family practitioners, most patients with ADHD will need specialized psychotherapy or medication for conduct disorder. If your child’s symptoms are severe enough to interfere with normal family life, you may need to seek out medications that can help reduce hyperactivity and other disruptive behaviors in order to improve the quality of your daily routine. Medication for conduct disorder, while effective at controlling symptoms, does not work miracles and can often produce unwanted side effects, so it is important to understand how to treat ADHD with medication.
How to treat ADHD with medication?
Once the cause of the disorder has been identified, you can use psychotherapy as the first step in treating the disorder with medication for ADHD. A thorough assessment of the child’s behavior is required in order to determine whether therapy is appropriate.
What is a behavior replacement intervention?
Behavior replacement is an intervention for conduct disorder that has proven to be highly effective.
What are the best treatments for a syphilis disorder?
The most common interventions for this disorder include cognitive behavioral therapy, behavior therapy, and pharmacotherapy. In addition, there are also psychosocial interventions that can be used.
What is the intervention for aggressive behavior in children?
One intervention for this disorder, behavior therapy, aims at modifying the patterns of inappropriate and aggressive behavior in children with this condition . These behaviors should be modified so that they do not become normal and acceptable behavior for children. This kind of intervention may involve teaching children coping skills that help them to recognize the appropriate behaviors when they are acting out.
How to treat conduct disorder?
Treatment for conduct disorder may include: Cognitive-behavioral therapy. A child learns how to better solve problems, communicate, and handle stress. He or she also learns how to control impulses and anger. Family therapy.
How can I help prevent conduct disorder in my child?
Things such as a traumatic experience, social problems, and biological factors may be involved. To reduce the risk for this disorder, parents can learn positive parenting strategies. This can help to create a closer parent-child relationship. It can also create a safe and stable home life for the child.
What is conduct disorder in children?
Conduct disorder is a type of behavior disorder. It’s when a child has antisocial behavior. He or she may disregard basic social standards and rules. He or she may also:
What are the symptoms of conduct disorder in a child?
But in children with the disorder, these symptoms occur more often. They also interfere with learning, school adjustment, and sometimes with the child’s relationships.
How is conduct disorder diagnosed in a child?
He or she will talk with parents and teachers about the child’s behavior and may observe the child. In some cases, your child may need mental health testing.
How can I help my child live with conduct disorder?
Early treatment for your child can often prevent future problems . Here are things you can do to help your child:
What are the symptoms of antisocial behavior in children?
Children with other mental health problems are more likely to have this disorder. Symptoms are divided into 4 main groups. They are aggression, destruction, deceitfulness, and violation of rules.
Why is it so hard to treat conduct disorder?
Treatment can prove difficult because children are often uncooperative and distrustful of adults.
What is conduct disorder?
Conduct disorder is a behavioral disorder that occurs when children engage in antisocial behaviors, have trouble following rules, and struggle to show empathy to others. They may also threaten the safety of others or themselves. Conduct disorder typically emerges in children under the age of 16, but can be diagnosed in adults as well.
What is the difference between autism and conduct disorder?
One is that people with conduct disorder have trouble with social interaction because of deficits in social learning, whereas people with autism have trouble socializing due to developmental challenges.
What are the causes of conduct disorder in children?
Children diagnosed with conduct disorder may have a history of the following: abuse. poverty. parental substance abuse. other mental health problems. family conflict or violence. brain damage. other trauma. Researchers also believe that genetics may play a role in the development of conduct disorder.
How long does it take to get diagnosed with conduct disorder?
Signs must have been present for at least a year in order to receive a diagnosis.
How can positive parenting help with conduct disorder?
Researchers believe that positive parenting as well as providing a safe and supportive environment for a child can reduce the risk of conduct disorder. Reducing the risk factors that can increase the possibility of conduct disorder, such as poverty and abuse, is likely to ensure the best outcome for the child.
Which is more likely to be diagnosed with conduct disorder: boys or girls?
Boys are more likely to receive a diagnosis than girls. Neuropsychologists and other researchers believe that the development of conduct disorder is somehow related to impairment in the frontal lobe of the brain, which can keep children and teens from learning from negative experiences and adjusting their behaviors.
How to treat conduct disorder?
Treatment options for conduct disorder are family therapy, behavioral modification and pharmacotherapy, often in combination. The clinician must assess the severity of the individual child’s disorder and should refer the child and family to a subspecialist if any of the following conditions apply: there are concerns about safety, diagnostic behaviors escalate rapidly, psychoeducational interventions are ineffective, there is conflicting information from multiple sources or many comorbid symptoms exist [4]. Substance abuse problems should be treated first with appropriate interventions and rehabilitation.
What are the characteristics of conduct disorder?
The primary features of conduct disorder are: Aggression. Vandalism. Theft. Frequent lying. Violation of rules, running away. About 40 percent of children with the diagnosis of conduct disorder will grow into adults with antisocial personality disorder.
Why should comorbid disorders be identified in making the diagnosis?
Comorbid disorders such as the following should be identified in making the diagnosis because their existence can influence presentation and treatment options: Attention deficit hyperactivity disorder (ADHD), which has features of disinhibition, inattention and distractability.
What percentage of boys have conduct disorder?
As many as 5 percent of preadolescent boys, 8 percent of adolescent boys and a quarter to a half that percentage of girls of those same ages fulfill criteria for a diagnosis of conduct disorder [1]. In contrast to isolated behavior problems, this diagnosis requires a repeated, persistent pattern of violating the rights of others and age-appropriate societal rules for six months or more. Multiple factors are probably responsible for this developmental pathway [2]. The primary features of conduct disorder are:
What is the best medication for depressive behavior?
Medical monitoring of cardiac history, height and weight, sleep, and symptom reports from parents and teachers are recommended. Antidepressants such as fluoxetine (a selective seratonin reuptake inhibitor, or SSRI) may benefit patients with depressive, rigid or inflexible aggressive behaviors.
What is intermittent explosive disorder?
Intermittent explosive disorder, which is characterized by sudden aggressive outbursts in isolation from all other persistent symptoms. It is unprovoked and without intent to harm anyone.
Is pharmacotherapy an adjuvant treatment?
Pharmacotherapy can be an adjuvant treatment for children who are highly aggressive, impulsive or have mood-disorder symptoms. No medications have been formally approved for conduct disorders in general, so medications are directed at specific symptoms.
Is there a drug for CD?
Although conduct disorder (CD) is the most common psychiatric disorder in youth from the community and encompasses one third to one half of all referrals to child and adolescent clinics, there is no licensed drug, to date, for treatment of CD, neither in Europe nor in the US.
Is there a drug for conduct disorder?
Although conduct disorder (CD) is the most common psychiatric disorder in youth from the community and encompasses one third to one half of all referrals to child and adolescent clinics, there is no licensed drug, to date, for treatment of CD, neither in Europe nor in the US. The aims of this paper are to review research data available on the use of medication for CD in young people and to identify future directions for research. We review 17 controlled studies and six open trials. Investigated compounds mainly belong to three classes of psychotropic drugs: mood stabilizers, neuroleptics and stimulants (six, five and six controlled studies, respectively). Lithium is the most documented treatment (3/4 positive studies). Conventional neuroleptics have been most commonly prescribed (3/3 positive studies), atypical neuroleptics appear promising (2/2 positive studies). Methylphenidate improves some CD symptoms, even in the absence of ADHD (6/6 positive studies). Sparse research has been conducted on response to antidepressants. The evidence for an effective role of pharmacotherapy in CD is still limited. Treatment should be multimodal and individualized to each patient's specific condition.
How to manage CDs?
Nonpharmacological management has been the mainstay of treatment in managing the CDs. The preventive programs as discussed in the later section should form the most important of the intervention strategies while talking about this issue. In preschool children such programs, for example, Head Start has been tried. They provide parent education about normal development; provide children with stimulation and crisis management to the parents. In the clinical setting, the interventions are targeted toward the temperament of the child, the interpersonal relations in the family, and increasing the parental efficiency in addressing the child's behavioral issues. In the school-aged children, the primary target of intervention is the child, family, and the school. Both parenting skills training and training for the child to improve peer relationships, social competence, academic performance, and compliance with demands from parents/teachers are effective for CD. As in adolescent period the relative importance of peers is increased than that of the family, the interventions should also be targeted toward the peer group. The multi-systemic therapy is imparted in the family environment to the adolescents with conduct problems. It combines intensive case management in the home setting with family interventions, and this has been found to be cost effective. Psychoeducational intervention to inculcate social skills, address conflict resolution and anger control skills to target adolescents and parents are found to be helpful.
What is the Achenbach's child behavior checklist?
The Achenbach's child behavior checklist had an Indian adapted version and known as childhood psychopathology measurement schedule (CPMS). It is a semi-structured interview schedule having 75 symptoms and has a designated section on CD symptoms, and it gives a dimensional score. It is standardized on Indian children with good reliability (0.88–0.98) and validity. With a cut-off score of >10, CPMS has 82% sensitivity and 87% specificity.
What is antisocial behavior?
Conduct disorder (CD) and associated antisocial behavior is one of the most common mental and behavioral problems in children and young people. In the United States, CDs associated behaviors are primary presenting complains in children and adolescent. CD are characterized by a repetitive and persistent pattern of dissocial, aggressive, or defiant conduct (ICD-10). Associated behaviors are outside the socially accepted norms that results into persistent and significant violations of age appropriate social expectations. CD is classified along with the diagnosis of oppositional defiant disorder (ODD) in the spectrum of disruptive behavior disorders. ODD can be seen as precursor to the development of CD. Behaviors include stealing and lying, excessive physical and verbal aggression, rule breaking and violence. Persistence of these behaviors into adulthood leads to antisocial personality disorder (ASPD). As these behaviors are present in some children during the course of development, it is essential for the clinician to differentiate between normalcy and pathological behavior. Remote antisocial or illicit acts are not enough to support a diagnosis of CD. CD must be differentiated from other term like delinquency. CD is a mental and behavioral disorder while delinquency is a legal term. It is comorbid with many other psychiatric conditions, including attention deficit hyperactive disorder (ADHD), depression, substance use disorders, etc. CD in early life has been found to be strongly associated with significant decline in educational performance. They are more likely to remain socially isolated with increase in substance misuse during adolescence. There is increase involvement in criminal acts resulting in frequent contact with the criminal justice system. This adverse effect continues even in adult life with resulting poorer educational and occupational outcomes. There are limited data available about the prevalence of CD across the world. Using the diagnostic and statistical manual of mental disorders-III (DSM-III) and DSM-III-R diagnostic guidelines, the prevalence of CD in the United States was found to be 6%–16% in males and from 2% to 9% in females. With a clinical interview as a method of detection, the prevalence of CD in the general population is found to be between 1.5% and 4%. Boys are likely to have these conditions two times more than girls. Those with early-onset exhibit lower IQ compared to children with later age of onset. They have more attention deficits and impulsivity problems. It is comorbid with many other psychiatric conditions including ADHD, depression, substance use disorders, etc., Children with CD also find difficulty in interacting and integrating with peer group and are more likely to had adverse family circumstances. Increased risk factors include poor prenatal care and poor infant nutrition, poverty, physical abuse, and more crime in the neighborhood society. Families of children and adolescent with CD are more likely to exhibit parents with low income, substance abuse, depression, somatization, and ASPD. CD in early life has been found to be strongly associated with significant decline in educational performance. They are more likely to remain socially isolated with increase in substance misuse during adolescence. There is increase involvement into criminal acts resulting into frequent contact with the criminal justice system. This adverse effect continues even in adult life with resulting poorer educational and occupational outcomes.
Is CD a syndromal diagnosis?
The syndromal diagnosis of CD, which should be differentiated from ODD as described in previous section
What Are the Causes of Conduct Disorder?
While the exact cause of conduct disorder is unknown, it is thought to be the result of a combination of factors including, but not limited to:
What are the co-morbid conditions of conduct disorder?
Many children and teens with conduct disorder have co-morbid conditions like ADHD, mood disorders, anxiety, depression, and substance abuse. These conditions can make the symptoms of conduct disorder worse, making it more important than ever to get these challenges under control.
Why do children have behaviour problems?
While most children go through a period where they act out and try to push their limits, a child’s behaviour-related problems are thought to be the result of conduct disorder if they are long-lasting, infringe on the rights of others, and/or disrupt a child’s life and the lives of his or her family members.
What is cognitive behavior therapy?
Cognitive Behavior Therapy helps a child learn how to reframe the way they think, allowing them to improve their impulse control, anger management, and problem-solving skills.
How does psychotherapy help children?
Psychotherapy helps a child learn how to better express and control his or her feelings, exercise self-control, see other people’s points of view, etc. Psychotherapy can be conducted in a group setting for younger kids or on an individual basis for older kids.
Can medication help with conduct disorder?
While there is no known medication for conduct disorder, some medications can be used to treat specific symptoms (impulsivity, mood, etc.). Additionally, if your child has another condition like ADHD or depression, using medication to get those symptoms under control can be beneficial. 8.
Is it hard to deal with conduct disorder in kids?
There’s no doubt that dealing with conduct disorder in kids can be extremely challenging, and while it can be very difficult to stand your ground in the face of your child’s explosive anger, consistency really is key.
Prevalence and Causes
Signs of Conduct Disorder
Diagnosis
Conduct Disorder Treatment
Specialist to consult
Prevention of Conduct Disorder