
Medication
Jan 07, 2020 · Another treatment option is kyphoplasty, a minimally invasive procedure used to treat spinal compression fractures. It reduces pain by using bone cement to repair fractures caused by osteoporosis or cancer. For chronic disk pain, the doctor can perform an ablation, which burns the specific nerves that carry pain signals from the bony endplates.
Procedures
Chronic pain can significantly inhibit one’s ability to do the activities you love – however, there is hope. Traditional chronic pain treatments include physical therapy, prescription medications, steroid injections, and surgery. HFX, the most advanced spinal cord stimulator, offers the widest range of benefits.
Self-care
The following actions can help you cope with your chronic pain and improve your overall health: Avoid smoking. Don’t try to do too much. Create a daily schedule that includes a few priorities and time for rest and self-care. Eat a healthy diet. Exercise regularly. Get enough sleep. Manage your ...
Nutrition
For more information on complementary health approaches that have been studied for pain, see: Acupuncture Massage therapy Meditation Qigong Relaxation …
See more
Patients who have chronic pain likely will not obtain adequate pain control through the single daily dose of methadone that can be provided through an OTP. Such programs may, however, be willing to collaborate in the management of patients, providing addiction treatment and allowing the prescription of additional opioids for pain management through a medical provider.
What is the best thing for chronic pain?
Effective approaches to chronic pain should: Use nonopioid therapies to the extent possible Identify and address co-existing mental health conditions (e.g., depression, anxiety, PTSD) Focus on functional goals and improvement, engaging patients actively in their pain management Use disease-specific treatments when available (e.g., triptans for migraines, …
Are there better ways to treat chronic pain?
How can you effectively treat chronic pain?
What is the best medicine for chronic pain?
See more

What is the most common treatment for chronic pain?
What is the preferred treatment plan for chronic pain?
What are 3 different types of pain management?
- pain medicines.
- physical therapies (such as heat or cold packs, massage, hydrotherapy and exercise)
- psychological therapies (such as cognitive behavioural therapy, relaxation techniques and meditation)
- mind and body techniques (such as acupuncture)
- community support groups.
What are pain management options?
- Acetaminophen (Tylenol®) or ibuprofen (Advil®)
- Topical Ointments (for example lidocaine)
- Exercise therapy, including physical therapy.
- Interventional therapies (injections)
- Exercise and weight loss.
Why is treating chronic pain so difficult?
How do you live with severe chronic pain?
- Avoid smoking.
- Don't try to do too much. ...
- Eat a healthy diet.
- Exercise regularly.
- Get enough sleep.
- Manage your stress.
- Join a support group for chronic pain to learn from other people with similar conditions.
- Limit alcohol, which can cause more problems with sleep and pain.
What is the strongest pain medication?
- Opioid analgesics, in general, are the strongest pain-relieving medications. ...
- Codeine is only about 1/10th as powerful as morphine.
- Opioids more powerful than morphine include hydromorphone (Dilaudid) and oxymorphone (Opana).
What is a drug that removes pain known as?
Is tramadol stronger than codeine?
What is a new treatment to pain that is being developed?
What can be prescribed instead of opioids?
Can chronic pain be managed?
How to treat chronic pain?
The treatments for chronic painare as diverse as the causes. From over-the-counter and prescription drugsto mind/body techniques to acupuncture, there are a lot of approaches. But when it comes to treating chronic pain, no single technique is guaranteed to produce complete pain relief. Relief may be found by using a combination of treatment options.
What is WebMD for chronic pain?
WebMD provides an overview of treatments for chronic pain, from surgery to herbal remedies.
What is the best medication for pain?
Drug Therapy: Nonprescription and Prescription. Milder forms of pain may be relieved by over-the-counter medications such as Tylenol ( acetaminophen) or nonsteroidal anti-inflammatory drugs ( NSAIDs) such as aspirin, ibuprofen, and naproxen.
What are some exercises that help with chronic pain?
Some exercises are easier for certain chronic pain sufferers to perform than others; try swimming, biking, walking, rowing, and yoga. Psychological Treatment. When you are in pain, you may have feelings of anger, sadness, hopelessness, and/or despair.
Can chronic pain be controlled?
Many people suffering from chronic pain are able to gain some measure of control over it by trying many of the above treatments on their own. But for some, no matter what treatment approach they try, they still suffer from debilitating pain.
Can you have a surgical implant for pain?
When standard medicines and physical therapy fail to offer adequate pain relief, you may be a candidate for a surgical implant to help you control pain. When they are used, which is rare, there are two main types of implants to control pain: Intrathecal Drug Delivery.
Can acupuncture help with chronic pain?
From over-the-counter and prescription drugs to mind/body techniques to acupuncture, there are a lot of approaches. But when it comes to treating chronic pain, no single technique is guaranteed to produce complete pain relief. Relief may be found by using a combination of treatment options.
What is pain management specialist?
Your pain management specialist is a physician specialist like your surgeon or internist. You probably will receive a bill for your pain management specialist's professional service as you would from other physicians. If you have any financial concerns, your pain management specialist or an office staff member will answer your questions.
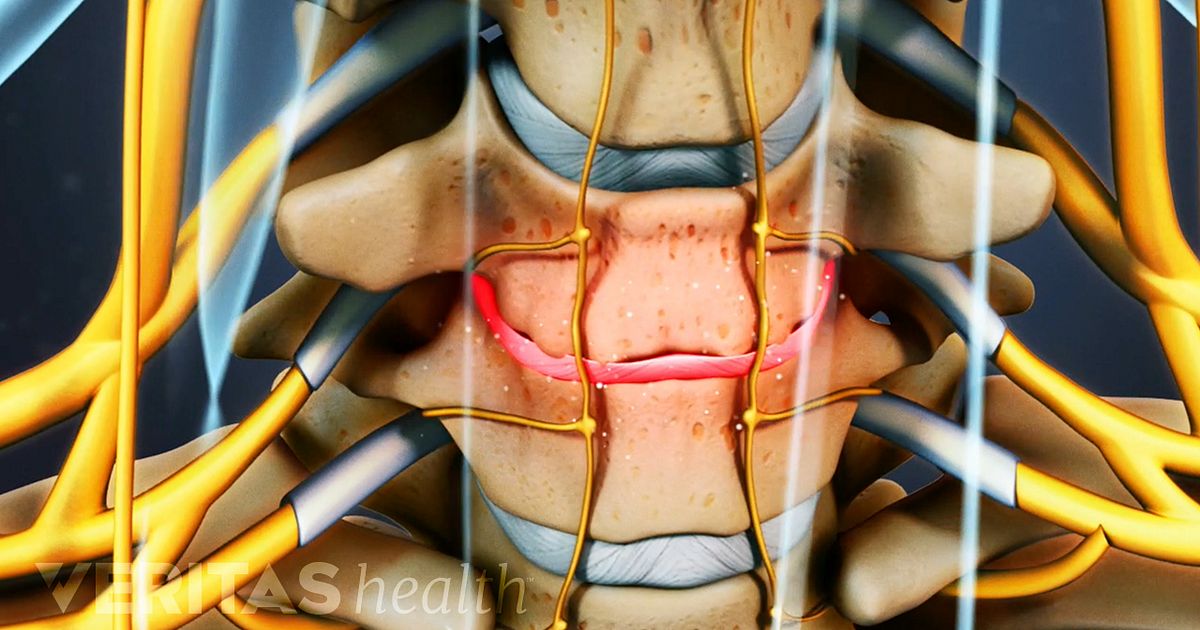
How to treat lumbar nerve pain?
These injections are often performed under fluoroscopic (X-ray) guidance or ultrasound guidance. Local anesthetic is placed near the lumbar sympathetic chain to relieve the pain. Your leg will likely become warm immediately following the injection: this is an expected effect and not a complication. Back soreness is one of the more common side effects. If you feel any sharp pains down your leg or to your groin during the injection, you should let the physician know immediately. There may be some temporary numbness following the injection, but contact your doctor if you experience persistent numbness or weakness lasting more than 8 hours. You will be positioned on your stomach for this injection. The injection is performed at the level of lumbar vertebrae two and three, in the lower back. A needle is placed under X-ray guidance, just anterior to the vertebral body to the side of the affected area where the ganglion is located. When the needles are positioned, a small amount of dye is injected to make sure the needle is in the right spot. After the doctor is satisfied that the contrast dye is in the right place, they will inject numbing medicine then remove the needle.
What is the best way to treat pain in the neck?
Techniques involving injections are commonly offered to help alleviate pain. Known as interventional therapy, these injections often deposit local anesthetics or cortisone into the area surrounding nerves or joints. Depending on the type of pain, these injections can target painful muscles, a technique known as trigger point injections, or may involve other structures of the body such as the epidural space, which are called epidural steroid injections. Based on the area of pain, epidural injections can target the neck, if there is pain radiating down the arms, or low back, if the legs are involved. Sympathetic nerve blocks can help with nerve-related pain, including complex regional pain syndrome (CRPS).
How to treat celiac plexus pain?
Celiac plexus block: A celiac plexus block is performed under fluoroscopic (X-ray) guidance to relieve pain in patients with chronic abdominal pain or cancer in areas of the abdomen causing significant pain. You will be positioned on your stomach for this injection, and a needle is placed in the area of the back to target the sympathetic nerves of the abdomen. A small amount of dye is deposited through the needles and, if appropriately placed, numbing medicine is delivered to the area of a group of nerves called the celiac plexus. For chronic pain, this injection is performed in a series of three. For cancer pain, a single diagnostic injection is used to see whether a more permanent injection may help with the pain. If the diagnostic nerve block provides significant pain relief, the longer lasting injection may be done using either phenol or alcohol solution.
How to treat neck pain with facet injection?
Facet joint injection: The facet joints assist with movement and stabilization of the spine both in the neck and back. Injection into these joints can provide relief of neck or back pain; these injections are always performed under X-ray guidance. Patients may feel soreness in the neck or back when the needle is inserted. You will be positioned to lay on your stomach for this injection. A needle is placed in your neck or back and advanced to the level of the joint under x-ray visualization. This injection or nerve block is often used to learn more about what is causing the pain. A longer-lasting injection may be needed if you have significant pain relief from this injection. An example of a longer-lasting injection is radiofrequency ablation, which uses electric current to heat up an area of nerve tissue to stop it from sending pain signals.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs are most effective for mild to moderate pain that's accompanied by swelling and inflammation. These drugs are commonly used for arthritis and pain resulting from muscle sprains, strains, back and neck injuries, or menstrual cramps.
Acetaminophen
Acetaminophen is usually recommended as a first line treatment for mild to moderate pain, such as from a skin injury, headache or musculoskeletal condition. Acetaminophen is often prescribed to help manage osteoarthritis and back pain. It may also be combined with opioids to reduce the amount of opioid needed.
COX-2 inhibitors
These medications were developed with the aim of reducing common side effects associated with traditional NSAIDs. COX -2 inhibitors are commonly used for arthritis and pain resulting from muscle sprains, strains, back and neck injuries, or menstrual cramps.
Antidepressants and anti-seizure medications
Some medications commonly prescribed to manage depression and prevent epileptic seizures have also been found to help relieve chronic pain, including back pain, fibromyalgia and diabetes-related nerve pain (diabetic neuropathy). Because chronic pain often worsens depression, antidepressants may doubly benefit pain and mood symptoms.
Opioids
Opioid medications are synthetic cousins of opium and the drugs derived from opium, such as heroin and morphine. These drugs are often prescribed for acute pain that stems from traumatic injury, such as surgery or a broken bone.
What is the treatment for spinal compression fractures?
Another treatment option is kyphoplasty, a minimally invasive procedure used to treat spinal compression fractures. It reduces pain by using bone cement to repair fractures caused by osteoporosis or cancer.
What is the procedure for disc pain?
For chronic disk pain, the doctor can perform an ablation, which burns the specific nerves that carry pain signals from the bony endplates.
What is nerve block therapy?
Nerve block techniques, for example, deliver numbing medication directly to the nerve causing the problem. The process can be used to treat pain as well as diagnose specific problems. Neuromodulation therapy delivers electrical current or pharmaceutical agents directly to a targeted nerve area. There are two versions.
Can you prescribe opioids for herniated disks?
“For chronic, non-cancer-related pain, we don’t prescribe opioids. People are looking for non-opioid treatment,” explained Dr. Verrill. “The current opioid crisis confirms that this is the best way to manage pain, with a few exceptions like severe pain caused by cancer.”
How long does chronic pain last?
So, what is chronic pain and how can I get relief? Chronic pain, which lasts three months or longer, is persistent and is often debilitating.
What does a physical therapist do?
Physical therapists can identify areas of weakness that may be contributing to pain. When muscles and joints are strengthened through exercises, you may experience pain relief. Physical therapists can help you learn new ways of doing daily activities that won’t cause pain. Physical therapists can also provide education to help you avoid further injuries.
Can you take opioids for pain?
When you first start experiencing pain, you may treat it with over-the-counter pain medications. If that isn’t effective, your doctor may recommend prescription medications like opioids. While these prescription medications are often helpful for acute pain, they are less useful for chronic pain. It’s crucial to really understand the side effects of prescription medications. There is a significant risk for serious side effects, including addiction. You may also experience drowsiness and constipation.
Can you get epidurals for pain?
Your doctor may also suggest epidural steroid injections. With these injections, steroids are directly inserted into the spine. While these injections don’t offer long-term pain relief, you may find injections useful for short-term pain relief.
What is the best treatment for chronic pain?
Counseling: Talk therapy can help you manage chronic pain, especially psychogenic pain. Occupational therapy: Activities teach you how to do everyday tasks differently to lessen pain or avoid injury. Physical therapy: Exercises stretch and strengthen your body.
How do healthcare providers treat chronic pain?
The approach depends on the type of pain, its cause (if known) and other factors that vary from person to person. The best treatment plans use a variety of strategies — medications, lifestyle changes and therapies.
How common is chronic pain?
Chronic pain is a very common condition, and one of the most common reasons why someone seeks medical care. Approximately 25% of adults in the United States experience chronic pain.
How long does chronic pain last?
Chronic pain is pain that lasts for a long time — months or years. It can happen anywhere in the body. The pain can be there all the time, or it may come and go. Chronic pain can interfere with your daily activities, such as working, having a social life and taking care of yourself or others. It can lead to depression, anxiety ...
Why is it important to seek treatment for mental health issues?
If you have chronic pain and depression and/or anxiety, it’s important to seek treatment for your mental health. Untreated depression and anxiety can make your pain worse and further lower your quality of life.
What is chronic pain?
Chronic pain differs from another type of pain called acute pain. Acute pain happens when something hurts you. It doesn’t last long, and it goes away after your body heals from whatever caused the pain. In contrast, chronic pain continues long after you recover from an injury or illness.
What are some ways to relieve pain?
Certain lifestyle changes and types of alternative medicine have also been shown to relieve chronic pain over time: Acupuncture, which uses small needs placed in the body. Aromatherapy, which uses crushed plants.
What are some complementary therapies that can help with pain?
A growing body of evidence suggests that some complementary approaches, such as acupuncture, hypnosis, massage, mindfulness meditation, spinal manipulation, tai chi, and yoga, may help to manage some painful conditions.
What are the most common chronic pain conditions?
Not all people with chronic pain have a health problem diagnosed by a health care provider, but among those who do, the most frequent conditions by far are low-back pain or osteoarthritis, according to a national survey. Other common diagnoses include rheumatoid arthritis, migraine, carpal tunnel syndrome, and fibromyalgia.
What are some ways to reduce opioid pain?
There was evidence that acupuncture, yoga, relaxation techniques, tai chi, massage, and osteopathic or spinal manipulation may have some benefit for chronic pain, but only for acupuncture was there evidence that the technique could reduce a patient’s need for opioids.
What is the best treatment for low back pain?
The options they suggest include several complementary approaches—acupuncture, mindfulness-based stress reduction, tai chi, yoga, progressive relaxation, biofeedback, and spinal manipulation—as well as conventional methods such as exercise and cognitive behavioral therapy.
How long does yoga help with back pain?
A 2018 evaluation of the research on yoga for low-back pain by the Agency for Healthcare Research and Quality (AHRQ) found that it improved pain and function in both the short term (1 to 6 months) and intermediate term (6 to 12 months). The effects of yoga were similar to those of exercise.
How long does chronic pain last?
Chronic pain is pain that lasts more than several months (variously defined as 3 to 6 months, but longer than “normal healing”). It’s a very common problem. Results from the 2012 National Health Interview Survey show that: About 25.3 million U.S. adults (11.2 percent) had pain every day for the previous 3 months.
How does pain affect your life?
Pain can affect quality of life and productivity, and it may be accompanied by difficulty in moving around, disturbed sleep, anxiety, depression, and other problems . 1. For more information about chronic pain, visit the National Institute of Neurological Disorders and Stroke.
What is multidisciplinary pain management?
The effectiveness of multiple interventions is augmented when all medical and behavioral healthcare professionals involved collaborate as a team (Sanders, Harden, & Vicente, 2005). A multidisciplinary team approach provides a breadth of perspectives and skills that can enhance outcomes and reduce stress on individual providers. Although it is ideal when all relevant providers work within the same system and under the same roof, often a collaborative team must be coordinated across a community. This combined effort requires identification of a designated lead care coordinator and a good system of communication among team members and the patient. A treatment team can include the following professionals:
What is the treatment for CNCP?
Treat CNCP with non-opioid analgesics as determined by pathophysiology.
What is CNCP treatment?
Chronic noncancer pain (CNCP) is a major challenge for clinicians as well as for the patients who suffer from it. The complete elimination of pain is rarely obtainable for any substantial period. Therefore, patients and clinicians should discuss treatment goals that include reducing pain, maximizing function, and improving quality of life. The best outcomes can be achieved when chronic pain management addresses co-occurring mental disorders (e.g., depression, anxiety) and when it incorporates suitable nonpharmacologic and complementary therapies for symptom management. Exhibit 3-1 presents the consensus panel’s recommended strategy for treating CNCP in adults who have or are in recovery from a substance use disorder (SUD).
What is a PT in medical?
PT facilitates recovery from a large variety of medical conditions, including cardiopulmonary, geriatric, pediatric, integumentary, neurologic, and orthopedic. Neurologic PT and orthopedic PT are most likely to be used to treat chronic pain. Physical therapists use various hands-on approaches to help patients increase their range of motion, strength, and functioning. They also offer training in movement and exercises that help patients feel and function better.
Can benzodiazepines help with anxiety?
Excellent options to benzodiazepines for treating anxiety exist (see Treating Psychiatric Comorbidities, below).
Is there evidence for PT interventions?
Many widely used interventions by physical therapists lack definitive evidence. For example, several Cochrane Collaboration reviews of a commonly used PT modality—transcutaneous electrical nerve stimulation—found inconsistent evidence of effectiveness in a variety of chronic and acute pain conditions. Despite this lack of an evidence base, PT interventions have the advantages of being nonsurgical, bringing low risk of injury or dependence, and encouraging patients’ involvement in their own recovery.
Do benzodiazepines cause pain?
Researchers disagree on the beneficial and harmful effects of benzodiazepines and benzodiazepine receptor agonists on chronic pain. Several studies demonstrate increased pain with benzodiazepines or reduced pain following benzodiazepine antagonist use (Ciccone et al., 2000; Gear et al., 1997; Nemmani & Mogil, 2003; Pakulska & Czarnecka, 2001). All benzodiazepines have side effects, including impaired coordination, reduced memory, and addiction liability. For the following reasons, the consensus panel concludes that benzodiazepines have no role in the treatment of CNCP in patients who have comorbid SUD, beyond very short-term, closely supervised treatment of acute anxiety states:
Nonsteroidal Anti-Inflammatory Drugs
Acetaminophen
COX-2 Inhibitors
Antidepressants and Anti-Seizure Medications
Specialist to consult
Opioids
- The treatments for chronic pain are as diverse as the causes. From over-the-counter and prescription drugs to mind/body techniques to acupuncture, there are a lot of approaches. But when it comes to treating chronic pain, no single technique is guaranteed to produce complete pain relief. Relief may be found by using a combination of treatment optio...