...
Insulin and other medications
- Short-acting (regular) insulin.
- Rapid-acting insulin.
- Intermediate-acting (NPH) insulin.
- Long-acting insulin.
Medication
Apr 05, 2018 · In a landmark study, researchers compared immunotherapy based treatment for type 1 diabetes with placebo and showed that the novel immune treatment can stop the progression of type 1 diabetes. The immune therapy was also deemed safe among subjects. The study was published in the journal Science Translational Medicine.
Nutrition
4 rows · For more than 50 years, regular, NPH and Lente insulins derived from the pancreata of animals were ...
See more
When medicines and lifestyle changes are not enough to manage your diabetes, a less common treatment may be an option. Other treatments include bariatric surgery for certain people with type 1 or type 2 diabetes, and an "artificial pancreas" and pancreatic islet transplantation for some people with type 1 diabetes. Bariatric surgery
What is the best medicine for Type 1 diabetes?
Nov 20, 2017 · Insulin therapy itself is the basis in treatment of type 1 diabetes. Recent years have brought multiple solutions in the implementation of the treatment. New types of insulin, modern glycaemia monitoring, and insulin administration techniques revolutionized the capabilities of contemporary insulin therapy.
What you should know about treating Type 1 diabetes?
May 10, 2022 · Treatment for Type 1 Diabetes Since type-1 people with diabetes fail to produce insulin from the beta cells in their pancreas, the patients need to administer a set dosage of insulin into their bodies every day. The dose depends on the extent of the disease and the overall physiological functions of the patient.
Is there a cure for diabetes type 1?
What drugs are used for Type 1 diabetes?
See more

What is the most common treatment for type 1 diabetes?
What is the latest treatment for type 1 diabetes?
What are the treatment options for diabetes?
...
Treatments for type 1 and type 2 diabetes
- Monitoring your blood sugar. ...
- Insulin. ...
- Oral or other medications. ...
- Transplantation. ...
- Bariatric surgery.
Can type 1 diabetes be treated with oral medications?
What is the best type of insulin for type 1 diabetes?
The quick action of insulin lispro makes it the ideal insulin for maintaining blood glucose levels below 180 mg per dL (10 mmol per L) for two hours after a meal, particularly when the meal contains foods that are relatively high in carbohydrates and low in fat.Nov 15, 1999
Can type 1 diabetes be treated without insulin?
Which type diabetes is worse 1 or 2?
Can you manage diabetes without medication?
How does an artificial pancreas work?
An artificial pancreas is a medical device that mimics the work of a real pancreas by monitoring your blood sugar levels and releasing insulin automatically. Instead of checking your glucose levels and injecting yourself throughout the day, you wear a sensor under your skin, a continuous glucose monitor, and an insulin pump. The insulin pump releases a low level of insulin in a steady stream throughout the day. When the sensor perceives that your glucose levels are spiking, such as after a meal, it triggers the pump automatically releasing the right dose of insulin to balance it out. You and your doctor can monitor the whole process on a smartphone app.
How does diabetes affect mood?
Managing type 1 diabetes can be stressful, and fluctuating glucose levels can affect your mood throughout the day. Diabetes can also increase your risk of depression. It’s important to manage your stress by getting enough sleep and finding support.
What is islet cell transplant?
Islet cell transplantation is a procedure that takes healthy insulin-producing cells from a donor pancreas, and transplants them into a person with type 1 diabetes. Clinical trials have shown that islet transplantation therapy can restore a person’s natural ability to produce insulin on their own, reducing or even eliminating the need for insulin injections.
What is an insulin pump?
Insulin pump. An insulin pump is a device you wear on your body at all times. Instead of injecting yourself throughout the day, the pump delivers a steady dose of insulin, as well as supplemental doses at meal times. You’ll need to maintain and refill the pump, and move it to a different site on your body every few days.
How to control blood sugar levels in type 1 diabetes?
Monitoring carbohydrates can help you avoid a blood sugar spike and plan ahead for the amount of insulin you need to take. Eating a healthy diet with plenty of fruits, vegetables, and whole grains, and limiting animal proteins, sugars, and refined carbohydrates like white bread can also help you stabilize your blood sugar and keep your heart and cardiovascular system healthy.
How to help someone with diabetes?
Your physician might have a counselor or social worker on their diabetes care team, or you can find a therapist to speak with on your own. There are also many diabetes support groups where you can talk with people who understand the challenges you are facing and can share their experiences and suggestions. Finally, talking to a supportive friend or family member can help reduce your stress.
How long does it take for insulin to work?
Rapid-acting insulin, which starts working in 15 minutes after injection and lasts three to four hours.
Why is blood sugar high?
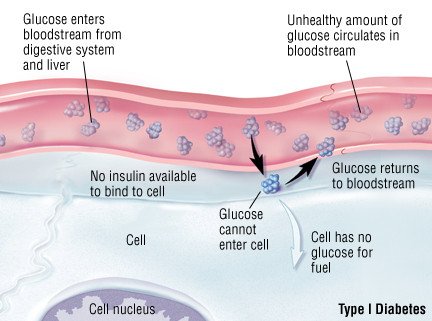
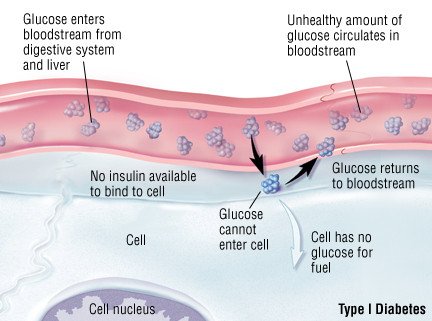
When you don’t have insulin, blood sugar can’t get into your cells and builds up in the bloodstream. That causes high blood sugar, which is bad for your body. High blood sugar causes many of the symptoms and complications of diabetes, like peeing a lot, feeling very thirsty, losing weight without trying, feeling very hungry, having blurry vision, having numbness or tingling, and feeling very tired, the CDC says.
What happens when blood sugar is too high?
Have strategies in place for when blood sugar levels are off. High blood sugar (aka hyperglycemia) happens when your blood sugar level is higher than your target or 180. This can cause symptoms like feeling really tired, having blurry vision, or needing to pee more often than usual, the NIDDK says.
How to know if your blood sugar is low?
If you have these symptoms and your blood sugar is low, the NIDDK recommends chewing four glucose tablets, drinking four ounces of fruit juice, drinking four ounces of regular (not diet) soda, or chewing four pieces of hard candy right away.
Why do doctors use insulin pumps?
“We usually like to have patients on insulin pumps if they can safely manage them because they’re easier and more flexible for people with diabetes ,” Dr. Dungan says. Some newer pumps can “provide more of an automated insulin delivery, so a patient is not constantly having to make adjustments,” she says.
What is the target blood sugar level?
Everyone’s target blood sugar levels are slightly different, but the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) says that targets usually are between 80 and 130 before you have a meal and below 180 two hours after the start of the meal.
What happens if you don't have insulin?
When you don’t have insulin, blood sugar can’t get into your cells and builds up in the bloodstream. That causes high blood sugar, which is bad for your body. High blood sugar causes many of the symptoms and complications of diabetes, like peeing a lot, feeling very thirsty, losing weight without trying, feeling very hungry, having blurry vision, ...
How to detect type 1 diabetes?
Type 1 diabetes is detected through a simple blood test. If you have the disease, your doctor will likely give you some options when it comes to treatment—and a lot of it is managed by you. 1. Take regular insulin shots or a use an insulin pump. People with type 1 diabetes will need to take regular insulin shots or wear an insulin pump ...
What is the T1D ratio?
This ratio is the amount of insulin needed to balance the intake of a certain amount of carbohydrates (typ ically measured in grams). Measuring the amount of carbohydrates and factoring the insulin to carb (I:C) ratio helps maintain stable blood-sugar levels after eating.
How is Type 1 diabetes managed?
Type 1 diabetes is managed through use of a variety of insulins. People with T1D must work closely with their medical team to find the right insulin treatment for their condition. Further information about the types of insulin and their effects are available on our insulin page.
What are the side effects of T1D?
The most common side effects of insulin are injection site reactions, which includes redness, soreness or irritation around the area. People can also experience lowered potassium levels and a risk of hypoglycemia.
What is the drug used to treat diabetes?
Metformin. Combined with insulin, diet and exercise, type 2 diabetes (T2D) drug metformin is sometimes prescribed to people with T1D to help treat their diabetes. Metformin helps control the body’s blood-sugar levels and how the liver processes sugar.
How many units of insulin should I take for an apple?
For example, if your I:C is 1:12 and you have an apple that contains 24g carbs, you would take two units of insulin. Taking those two units of insulin prior to having the apple helps to avoid a high or low blood-sugar fluctuation post-snack.
What kind of doctor do you see for T1D?
People with T1D regularly meet with a team of medical professionals (endocrinologist, ophthalmologist and dietitian) to help manage diabetes and to avoid the effects it has on the body.
How to treat T1D?
Monitoring blood sugar can be done using traditional blood-sugar meters or continuous glucose monitors (CGMs).
What is the role of GLP-1 RAs in promoting beta cell replication?
Recent evidence from rodent models indicates a role for GLP-1 RAs in protecting beta cells from apoptosis and in promoting beta cell replication and mass [113–117]. As such, although this remains to be confirmed, it is conceivable that GLP-1 RAs may offer a way to prevent the ‘unmasking’ of the beta cell to immune effector cells, for example, by downregulating expression of MHC class I proteins. Intriguingly, unpublished non-clinical evidence shows that liraglutide also limits immune cell infiltration into pseudo-islets (M. von Herrath, unpublished results). In addition, studies in NOD mice have shown that GLP-1 RAs administered in combination with various immunomodulatory agents, including anti-CD3 compounds [118], were more efficient in inducing diabetes remission than when given as monotherapy [119]. Furthermore, the anti-inflammatory effects of GLP-1 RAs are well-documented, with liraglutide being associated with reduced systemic levels of C-reactive protein and of proinflammatory cytokines, such as TNF-α, IL-1β and IL-6 [120–123]. Whilst these findings have mainly been observed in animal models or in type 2 diabetes, their relevance to (clinical) type 1 diabetes is conceivable but, so far, largely unexplored.
What is anti-inflammatory cytokine?
Anti-inflammatory cytokine-specific compounds, which are successfully used, for example, in rheumatic diseases, have been tested as alternatives to directly targeting the T or B cell in type 1 diabetes , as briefly summarised below.
What is the goal of immune-focused therapies in type 1 diabetes?
The overarching goal of immune-focused therapies in type 1 diabetes is to prevent or delay the loss of functional beta cell mass. The traditional understanding of autoimmunity in type 1 diabetes has focused on systemic immune dysregulation and on autoreactive T cells that have evaded thymic selection and migrated to the periphery, where they destroy islets. This view on the pathogenesis of type 1 diabetes has been referred to as T cell-mediated ‘homicide’ [6]. Thus, recent efforts have concentrated on cell- or cytokine-directed interventions, which have been successful in other autoimmune diseases. Targeting T cells or proinflammatory cytokines remain valid efforts and many agents are in active development; so far, however, these approaches have been only partly successful. This arguably indicates a need to refocus hypotheses, as discussed later in this review (see ‘Future perspectives’ section), where we outline how the beta cell itself contributes to its own demise (the ‘assisted suicide’ hypothesis).
What is the role of HLA in diabetes?
Type 1 diabetes is a polygenic disorder, in which susceptibility loci or genetic variation contributes to disease risk. The HLA region on chromosome 6 is the main susceptibility locus and, in recent years, many other loci across the genome have been associated with an increasing risk of the disease [8]. However, from studies in monozygotic twins, for whom the onset of type 1 diabetes can vary considerably [9], it has become evident that non-genetic factors play a major role in triggering or perpetuating overt type 1 diabetes. A multitude of efforts have failed at robustly identifying such factors, strongly indicating that no single pathogen is responsible. Viral infections have been suggested, including enteroviruses and human herpesvirus-6 [10–13]. Of note, however, studies (mainly in animals) have also suggested that several viral infections may prevent the development of type 1 diabetes [14, 15], in line with the ‘hygiene hypothesis’ [16, 17].
What is the pathophysiological feature of type 1 diabetes?
The overall pathophysiological feature is loss of functional beta cell mass in the pancreatic islets of Langerhans (Fig. (Fig.1)1) [5]. Hypotheses suggest that the loss of functional beta cell mass occurs in a chain of events analogous to an ‘assisted suicide’ [6, 7], where the demise of the beta cell is likely due to a combination of a dysfunctional beta cell that becomes more visible to the immune system, which, in turn, overreacts and destroys the beta cell.
How to prevent and manage diabetes?
First, there is an obvious need to act early to prevent or delay the destruction of functional beta cell mass by immunomodulatory intervention or other disease-modifying means. Second, stimulating or reprogramming the remaining beta cell mass to secrete insulin in a balanced way is required to avoid major blood glucose excursions with the lowest possible exogenous insulin dose. Third, reducing the risk of long-term complications, such as cardiovascular and renal outcomes, seems increasingly important (Fig. (Fig.1).1). Below we review selected current and in-development interventions meeting these three criteria (Table (Table11).
What are some strategies to help beta cells?
Correspondingly, beta cell rescue strategies are being pursued, which include antigen vaccination using, for example, oral insulin or peptides, as well as agents with suggested benefits on beta cell stress, such as verapamil and glucagon-like peptide-1 receptor agonists.
What is the treatment for poorly controlled type 1 diabetes?
Pancreatic islet transplantation is an experimental treatment for poorly controlled type 1 diabetes. Pancreatic islets are clusters of cells in the pancreas that make the hormone insulin. In type 1 diabetes, the body’s immune system attacks these cells. A pancreatic islet transplant replaces destroyed islets with new ones that make and release insulin. This procedure takes islets from the pancreas of an organ donor and transfers them to a person with type 1 diabetes. Because researchers are still studying pancreatic islet transplantation, the procedure is only available to people enrolled in research studies. Learn more about islet transplantation studies#N#External link#N#.
What is the treatment for diabetes?
Other treatments include bariatric surgery for certain people with type 1 or type 2 diabetes, and an "artificial pancreas" and pancreatic islet transplantation for some people with type 1 diabetes.
What is the best way to treat diabetes?
Taking insulin or other diabetes medicines is often part of treating diabetes. Along with healthy food choices and physical activity, medicine can help you manage the disease. Some other treatment options are also available.
How to control glucose levels during pregnancy?
If you have gestational diabetes, you should first try to control your blood glucose level by making healthy food choices and getting regular physical activity. If you can’t reach your blood glucose target, your health care team will talk with you about diabetes medicines, such as insulin or the diabetes pill metformin, that may be safe for you to take during pregnancy. Your health care team may start you on diabetes medicines right away if your blood glucose is very high.
What is the National Institute of Diabetes and Digestive and Kidney Diseases?
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. The NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by the NIDDK is carefully reviewed by NIDDK scientists and other experts.
How to take insulin?
Inhaler. Another way to take insulin is by breathing powdered insulin from an inhaler device into your mouth. The insulin goes into your lungs and moves quickly into your blood. Inhaled insulin is only for adults with type 1 or type 2 diabetes.
What is premixed insulin?
Your doctor might also recommend premixed insulin, which is a mix of two types of insulin. Some types of insulin cost more than others, so talk with your doctor about your options if you're concerned about cost. Read about financial help for diabetes care .
Prognosis
Administration
Medical uses
Treatment
Side effects
Diagnosis
Example
- Used in conjunction with insulin, pramlintide is often prescribed after other medications prove not as effective as needed. It acts as a hormone to help the body better control blood sugar.
Diet
- Medications for high blood pressure and high cholesterol as well as aspirin can be prescribed with insulin to help the overall health and treatment of diabetes. Since people with diabetes have an increased chance of cardiovascular disease, these drugs are used in combination with other diabetes medications. Treatment for T1D includes monitoring and lifestyle choices in addition t…