What causes SMA syndrome?
· Trusted Sourcethey may use are: X-ray barium swallow endoscopy CT scan Doppler ultrasound magnetic resonance angiography (MRA)
What is the treatment for systemic inflammatory response syndrome?
One way of treating SMA is to increase the amount of survival motor neuron protein in the body. These ways of treating SMA are often called “SMN-based” or “SMN-enhancing” approaches. All individuals with SMA have at least one, and often multiple, copies of a second gene, called survival motor neuron gene 2 ( SMN2 ), or the “SMA back-up gene.”
What causes superior mesenteric artery (SMA) syndrome?
Conclusion: SMA syndrome is a well-described entity which must be considered as a cause of vomiting associated with significant weight loss in young adults. Surgical treatment should be allied with psychological assessment to treat any underlying psychosocial abnormality. Publication types Case Reports Review MeSH terms Adolescent Adult Age Factors
Is there any natural treatment for Antisynthetase syndrome?
The first line of treatment for superior mesenteric artery syndrome is nonsurgical management that includes: Feeding through a catheter (parenteral nutrition) Gastric decompression (using a nasogastric tube) Electrolyte correction Fluid resuscitation Posture therapy

How is SMA stenosis treated?
Acute SMA occlusion is treated by embolectomy, thromboendarterectomy, or bypass grafting along with removal of infarcted bowel. With severe aortic disease, an iliac artery may be used as an inflow vessel for a bypass graft.
Can you fix SMA?
Results: The cause of superior mesenteric artery syndrome is variable but always results in duodenal obstruction. Surgery is one treatment option that is effective and can be performed laparoscopically.
What is an SMA procedure?
Options for surgery include a duodenojejunostomy or gastrojejunostomy to bypass the obstruction or a duodenal derotation procedure (otherwise known as the Strong procedure) to alter the aortomesenteric angle and place the third and fourth portions of the duodenum to the right of the superior mesenteric artery.
How serious is superior mesenteric artery syndrome?
Superior mesenteric artery syndrome can be severely debilitating and may require long term management, medications, costly parenteral nutrition (intravenous feeding) and rigorous follow-up.
How much does SMA treatment cost?
In the USA, nusinersen, the first therapy for spinal muscular atrophy approved in 2016, costs $750 000 in the first year and $375 000 every following year for a patient's lifetime compared with onasemnogene abeparvovec, which costs $2.1 million for a one-off injection in five $425 000 instalments.
Is SMAS life threatening?
CONCLUSION. SMA syndrome is a rare but life-threatening cause of abdominal pain and vomiting. SMA syndrome can occur in patients without chronic emesis.
How do you eat with SMA syndrome?
Some individuals may be able to tolerate small, frequent meals or a liquid or soft diet. In contrast, other individuals may not be able to tolerate oral or gastric enteral feeding at all, in which case, nasojejunal feeding or parenteral nutrition may be needed.
Is SMA syndrome painful?
Superior mesenteric artery (SMA) syndrome is a rare cause of abdominal pain, nausea and vomiting that may be undiagnosed in patients presenting to the emergency department (ED). We report a 54-year-old male presenting to a community ED with abdominal pain and the subsequent radiographic findings.
How long can you live with mesenteric ischemia?
The 2- and 5-year survival rates were 70% and 50% and mainly related to cardiovascular comorbidity and malignant disease. Only one patient died after a recurrent attack of arterial mesenteric thrombosis.
Is SMA syndrome a disability?
Spinal muscular atrophy (SMA) is a debilitating disease that can be classified as a disability if symptoms are severe enough to cause significant impairments. SMA is hereditary and progressive, affecting both the central and peripheral nervous systems as well as voluntary muscle function.
How common is SMA syndrome?
SMA syndrome is a rare pathology with an incidence that ranges between 0.013 and 0.3% [7]. The defining feature of this entity is upper gastrointestinal obstruction caused by compression of the third part of the duodenum between the SMA anteriorly and the aorta posteriorly [9].
How long do mesenteric stents last?
Endovascular mesenteric stenting is a durable option for CMI with 86% overall patency and 60% freedom from reintervention at 3 years.
How to treat SMA?
One way of treat ing SMA is to increase the amount of survival motor neuron protein in the body. These ways of treating SMA are often called “SMN-based” or “SMN-enhancing” approaches. All individuals with SMA have at least one, and often multiple, copies of a second gene, called survival motor neuron gene 2 ( SMN2 ), or the “SMA back-up gene.”.
How early can you start treatment for SMA?
Beginning therapy as early as possible is the only way to prevent this motor neuron loss. For babies identified through newborn screening, treatment should begin even before the infant shows symptoms of SMA. In clinical trials of SMN-based therapies, individuals who began treatment earlier had better results than those who began treatment later.
When do SMA neurons die?
This is especially important for SMN-enhancing therapies. When SMN levels are low , motor neuron cells shrink and eventually die. In infants with SMA Type 1, 90% of motor neurons have been lost by 6 months of age. And once these neurons are lost, they cannot be regenerated.
Can SMN be used to treat SMA?
Increasing the amount of SMN protein in the body is not the only way to treat SMA. The loss of SMN protein also impacts other systems, pathways, and processes, and other treatments target these systems. These approaches are often called “non-SMN” approaches. Many of these non-SMN approaches target the muscles or nerves.
Can you take two non-SMN drugs together?
Many of these non-SMN approaches target the muscles or nerves. Many researchers believe that it will take a combination of SMN-based and non-SMN treatments to provide the most benefit for those with SMA. This could mean that individuals with SMA will take two drugs together.
Can you be on SMN therapy?
Generally, you cannot be on an approved therapy and participate in a clinical trial, though there are some exceptions. For example, certain muscle drugs may be tested in individuals who are also on an approved SMN-enhancing therapy.
Is there a treatment for SMA?
Currently, there are multiple FDA-approved treatments for SMA. All are SMN-enhancing treatments. In addition to these these approved treatments, several other treatments are being tested in clinical trials. You can see a list of treatments below, including those that are approved by the U.S. Food and Drug Administration (FDA).
What Are the Symptoms of Superior Mesenteric Artery Syndrome?
There are a few symptoms that might indicate you have superior mesenteric artery syndrome. Different individuals may go through different symptoms of the same condition. Some of them include:
How Is Superior Mesenteric Artery Syndrome Diagnosed?
Your doctor may make a diagnosis of superior mesenteric artery syndrome by checking you for symptoms. Sometimes, the symptoms might be non-specific. Your doctor may go on to rule out other conditions that may share symptoms and do some tests to make the diagnosis. They include:
What Is the Treatment for Superior Mesenteric Artery Syndrome?
The first line of treatment for superior mesenteric artery syndrome is nonsurgical management that includes:
What is the best treatment for SMA?
onasemnogene abeparvovec-xioi (Zolgensma), which is approved to treat SMA in children under 2 years old. risdiplam (Evrysdi), which is approved to treat SMA in individuals ages 2 months and older. These treatments are relatively new, so experts don’t yet know what the long-term effects of using these treatments may be.
What is the FDA approved treatment for SMA?
SMA therapies. To treat the underlying causes of SMA, the Food and Drug Administration (FDA) has recently approved three specific therapies: nusinersen (Spinraza), which is approved to treat SMA in children and adults. onasemnogene abeparvovec-xioi (Zolgensma), which is approved to treat SMA in children under 2 years old.
How does SMN2 work?
It’s composed of a small molecule that works by modifying the amount of SMN protein that’s made from the SMN2 gene. Like SMN1, the SMN2 gene produces SMN protein. However, it typically does this at lower levels. In fact, the extent to which SMN2 produces functional SMN protein has an impact on the severity of SMA.
What is Spinraza used for?
Spinraza is a type of medication that’s designed to boost the production of an important protein , known as sensor motor neuron (SMN) protein. People with SMA don’t produce enough of this protein on their own. The protein helps motor nerves survive.
How is Zolgensma administered?
Zolgensma is a one-time treatment that’s administered through intravenous (IV) infusion.
Why is it so hard to breathe with SMA?
Children with SMA tend to have weak respiratory muscles, which makes it harder to breathe and cough. Many also develop rib deformities, which can worsen breathing difficulties.
What is spinal muscular atrophy?
Takeaway. Spinal muscular atrophy (SMA) is a rare genetic condition that causes muscles to become atrophied and weak. Most types of SMA begin during infancy or early childhood. SMA can lead to joint deformities, feeding difficulties, and potentially life threatening breathing problems. Children and adults with SMA may have difficulty sitting, ...
What is the diagnosis of SMA syndrome?
SMA syndrome presents with vague symptoms of bowel obstruction. However, diagnosis is based on interpreting clinical symptoms alongside radiological testing which can confirm its presence. Various imaging modalities that can be used include plain film x-ray, barium x-ray, endoscopy, computed tomography (CT), Doppler ultrasound, and magnetic resonance angiography (MRA). Plain radiographs may reveal a dilated stomach and diminished distal bowel gas. Endoscopy and barium studies can be used but are often nonspecific and not available in an emergency setting. Endoscopy, rather, can be used to investigate complications of the disease including gastric stasis, biliary reflux, gastritis and duodenal ulcers and to rule out other cause of the duodenal compression. CT scan is helpful in diagnostics in that it allows for measurement of aortomesenteric (AO) angle which aids in confirmation of SMA syndrome and has thus replaced MRA as the standard for diagnosis. The normal AO angle is between 38 to 65 degrees and has a distance of 10 to 28 mm. In a study which reviewed 8 cases of SMA syndrome, a reported AO angle cutoff of 22 degrees revealed a 42.8% sensitivity and 100% specificity, and a distance of 8 mm was both 100% sensitive and specific for the condition. Laboratory tests are usually nondiagnostic and it is noted that electrolyte disturbances as well as protein and albumin levels can still be normal despite associated weight loss. While it is rare, SMA syndrome is important to consider because the delay in diagnosis can result in significant morbidity and mortality from malnutrition, dehydration, electrolyte abnormalities, gastric pneumatosis and portal venous gas, gastrointestinal hemorrhage and gastric perforation. [8][9][10]
What is the management of superior mesenteric artery syndrome?
The diagnosis and management of superior mesenteric artery syndrome is with an interprofessional team that consists of a general surgeon, radiologist, emergency department physician, and a gastroenterologist. However, the majority of patients with this syndrome initially present to the nurse practitioner and primary care provider. Because the symptoms are non-specific and there is no sensitive test, the diagnosis in most cases is delayed. Management in the acute setting includes fluid resuscitation, electrolyte correction, total parenteral nutrition and nasogastric tube insertion for gastric decompression. The patient should be educated on lifestyle changes such as eating small meals and adopt the left lateral decubitus position to improve symptoms. Most patients need a dietary consult as significant weight loss is common. Unfortunately, conservative measures help very few patients and most patients eventually require surgery. Various types of surgical procedures are done but none produces satisfactory results. Because there are very few cases, there are no large trials. Anecdotal reports indicate mild improvement in the short term but the long term prognosis remains unknown. The quality of life of these patients is poor. [11][12](Level V)
What is the treatment for AO angle?
The patient is encouraged to eat small meals and engage in posture therapy which involves patients lying in the left lateral decubitus position, rather than recombinant, to improve symptoms. Nutritional support through hyperalimentation is of great importance with conservative therapy in an attempt to increase the mesenteric fat pad, thus increasing the AO angle and improving symptoms. Many patients will fail conservative therapy and ultimately require surgical intervention. Various surgical procedures have been considered for surgical management including gastrojejunostomy, Strong procedure (a division of the ligament of Treitz), transabdominal duodenojejunostomy and laparoscopic duodenojejunostomy. Traditional open bypass surgery was the standard of care until 1998 when the first successful laparoscopic duodenojejunostomy was performed. This technique has since surpassed open bypass as the most common surgical treatment. Laparoscopic duodenojejunostomy has recently replaced open bypass at the standard operative treatment. A study involving laparoscopic duodenojejunostomy as a treatment for failed conservative management was done on 12 patients. This retrospective study revealed improved or eliminated symptoms in 11 of the 12 patients without any postoperative bowel obstruction, wound infection, anastomotic complications or deaths. Most surgeons prefer duodenojejunostomy due to reported success rates of 80% to 100% with reduced postoperative pain shortened hospital stay and reduced risk of incisional herniation.
Is superior mesenteric artery syndrome a morbidity?
Superior mesenteric artery syndrome is a rare cause of proximal small bowel obstruction and is linked to notable morbidity and mortality when the diagnosis is delayed. While superior mesenteric artery syndrome is rare, the morbidity and mortality associated with its complications make it a crucial differential to consider when concerned for bowel obstruction, especially in the setting of recent weight loss. Conservative management for SMA syndrome often fails, and laparoscopic duodenojejunostomy proves to be safe and effective as optimal definitive treatment.[1][2][3][4]
Is proximal small bowel obstruction a morbidity?
Superior mesenteric artery syndrome is a rare cause of proximal small bowel obstruct ion and is linked to significant morbidity and mortality when the diagnosis is delayed. Despite the rarity of this condition, the morbidity and mortality associated with its complications make it a crucial differential to consider when there is a concern for bowel obstruction, especially in the setting of recent weight loss. Conservative management for SMA syndrome often fails, and laparoscopic duodenojejunostomy proves to be safe and effective as optimal definitive treatment.
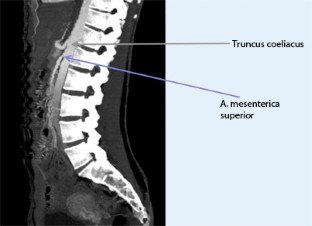
How to diagnose SMA syndrome?
SMA syndrome Radiology Diagnosis 1 The diagnosis of SMA syndrome is based on clinical symptoms and radiologic evidence of obstruction. 2 Plain radiograph dilated fluid and gas-filled stomach and proximal duodenum.#N#Upper GI fluoroscopy can demonstrate dilatation of the first and second part of the duodenum, extrinsic compression of the third part, and a collapsed small bowel distal to the crossing of the SMA. 3 CT and magnetic resonance angiography (CTA/MRA) enable visualization of vascular compression of the duodenum and measurement of aortomesenteric distance normally, the aortomesenteric angle and aortomesenteric distance are 25-60° and 10-28 mm, respectively in SMA syndrome, both parameters are reduced, with values of 6° to 15° and 2 to 8 mm.
When was SMA first diagnosed?
SMA syndrome was first described in 1861 by Carl Freiherr von Rokitansky in victims at autopsy, but remained pathologically undefined until 1927 when Wilkie published the first comprehensive series of 75 patients. According to a 1956 study, only 0.3% of patients referred for an upper-gastrointestinal-tract barium studies fit this diagnosis, making it one of the rarest gastrointestinal disorders known to medical science.
What is the SMA angle?
Superior mesenteric artery syndrome (SMAS) is a digestive condition that occurs when the duodenum (the first part of the small intestine) is compressed between two arteries (the aorta and the superior mesenteric artery). This compression causes partial or complete blockage of the duodenum. This rare, potentially life-threatening syndrome is typically caused by an angle of 6°–25° between the abdominal aorta and the SMA, in comparison to the normal range of 38°–56°, due to a lack of retroperitoneal and visceral fat (mesenteric fat). In addition, the aortomesenteric distance is 2–8 millimeters, as opposed to the typical 10–20. However, a narrow SMA angle alone is not enough to make a diagnosis, because patients with a low BMI, most notably children, have been known to have a narrow SMA angle with no symptoms of SMA syndrome
What are the complications of superior mesenteric artery syndrome?
Delay in the diagnosis of superior mesenteric artery syndrome can result in malnutrition, dehydration, electrolyte abnormalities, gastric pneumatosis and portal venous gas, formation of an obstructing duodenal bezoar, hypovolemia secondary to massive GI hemorrhage, and even death secondary to gastric perforation.
What is the first step in medical therapy?
Medical therapy usually begins with the initiation of intravenous fluids and, once no significant emesis, with the frequent administration of small amounts of liquids. In some cases, nasojejunal or nasogastric tube feedings with a standard liquid diet may be indicated. If the patient is completely obstructed or unable to tolerate liquids, total parenteral nutrition is indicated.
What kind of doctor treats SMA?
Neurologists are often the first doctors to meet with individuals suspected of having SMA, and should coordinate the multidisciplinary care team as needed. They specialize in the diagnosis and treatment of disorders of the nervous system (brain, spinal cord, muscles, nerves) and are a vital part of the care team. Some neurologists may conduct electromyography or nerve conduction studies to rule out other forms of muscle disease if a child has a negative gene test for spinal muscular atrophy.
What is noninvasive SMA?
Noninvasive SMA respiratory care involves techniques that avoid or delay the use of invasive intervention. Special equipment such as a ventilator or bilevel positive airway pressure (BiPAP) machine can deliver a continuous flow of air to the lungs through a mask that covers the mouth and/or nose. A cough assist device may also be used at home to help individuals cough and clear secretions.
Why is nutrition important for spinal muscular atrophy?
Nutrition is important for individuals with spinal muscular atrophy in order to promote growth and motor function. Individuals may experience over- or undernourishment, which can affect bone strength, growth, and overall mobility. Experts suggest working with a registered dietitian who is familiar with the nutritional needs of individuals with spinal muscular atrophy.
What is the role of anesthesiology in spinal muscular atrophy?
Anesthesiology is another important aspect in the care of individuals with spinal muscular atrophy who may have to undergo surgery such as tracheostomy or spinal stabilization. They handle planning of care before, during, and after surgery, as well as delivering anesthesia.
What is the best way to care for a child with spinal muscular atrophy?
The current guidelines of care for individuals with spinal muscular atrophy suggest that care is best accomplished with the help of many specialists and primary care providers. Because every individual with spinal muscular atrophy is different, the members, as well as their level of involvement, may change over time according to individual needs and circumstances. For children with SMA, caregivers are key members of this team, and are encouraged to work closely with their child’s healthcare provider in determining a care team that works best for them.
How to help with spinal muscular atrophy?
A proactive approach, including regular sessions of physical therapy, may help influence the progression of SMA. This may consist of exercises to help improve flexibility and overall function.
Can SMA cause weakness?
Muscle weakness may cause some individuals with SMA to lose their ability to chew and swallow effectively. This puts them at risk of inhaling food and liquid into the lungs and developing respiratory infections. A healthcare provider may recommend a temporary or long-term feeding tube put into place to provide the necessary nutrition and hydration.
What is the FDA approved medication for SMA?
Treatments for Adult-Onset SMA. As of May 2021, Spinraza (nusinersen) and Evrysdi (rysdiplam) are the only medications approved by the U.S. Food and Drug Administration (FDA) for the treatment of spinal muscular atrophy in adults as well as children. Researchers are beginning to focus on finding effective treatments for adults living ...
How does SMA help adults?
Treatment can benefit adults with SMA by improving quality of life and addressing complications associated with aging. More than one-third of people with spinal muscular atrophy (SMA) — 35 percent — are adults.
How many people have spinal muscular atrophy?
Article written by. Kelly Crumrin. About one-third of people with spinal muscular atrophy ( SMA) are adults. Adults with SMA may have a hard time accessing effective health care, and many disengage from the health care system. There is one medication approved to treat children over age 2 and adults with SMA. More treatments are being tested in ...
What percentage of people with SMA are adults?
More than one-third of people with spinal muscular atrophy (SMA) — 35 percent — are adults. Among adults with SMA, most have SMA type 3 (Kugelberg-Welander syndrome). Type 4, also known as adult-onset SMA, is the mildest type of SMA. Since SMA type 4 is extremely rare, there is little research and information about the condition available.
What is spinal muscular atrophy?
Facts and Statistics About Spinal Muscular Atrophy. Spinal muscular atrophy (SMA) is a rare disease involving nerve cells called motor neurons, which... If you or a loved one is living with spinal muscular atrophy (SMA), you’re already aware of the...
What is SMA-LED?
Spinal muscular atrop hy with lower extremity predominance (SMA-LED) is a rare type of spinal...
Which animal is the ultimate study model animal for spinal muscular atrophy?
Zebra fish are the ultimate study model animal for spinal muscular atrophy (SMA) because their...