
- medicines called anti-epileptic drugs (AEDs)
- surgery to remove a small part of the brain that's causing the seizures.
- a procedure to put a small electrical device inside the body that can help control seizures.
- a special diet (ketogenic diet) that can help control seizures.
What is the best treatment or Medicine for epilepsy?
When patients have been seizure free for two to five years, discontinuation of antiepileptic drugs may be considered. For patients with seizures that are not controlled with these agents, alternative treatments include surgical resection of the seizure focus, ketogenic diets, vagus nerve stimulators, and implantable brain neurostimulators.
What are the most common medications for epilepsy?
Jul 15, 2017 · Risk of recurrent seizures ... Treatment should begin with monotherapy. The appropriate choice of medication ... Epilepsy: Treatment Options GERALD LIU, MD, Atrius Health, Weymouth, Massachusetts
Is there a natural cure for epilepsy?
Seizure Medication. Side Effects. How to Get Off Your Medication. Ketogenic Diet. Nerve Stimulation. Surgery. After you’re diagnosed with epilepsy, you …
What is the best hospital for treatment of epilepsy?
Nov 04, 2021 · Candidates for epilepsy surgery must have failed several epilepsy drugs and have seizures with a known focus. Epilepsy surgeries fall into two general categories: resection and disconnection. Resection Surgery. The most common type of neurosurgery for epilepsy is resection, in which the portion of the brain causing seizures is removed.
What is the latest treatment for epilepsy?
The U.S. Food and Drug Administration today approved XCOPRI (cenobamate tablets) to treat partial-onset seizures in adults.Nov 21, 2019
What is the first line of treatment for epilepsy?
Lamotrigine and levetiracetam are emerging as first-line treatments for epilepsy, which people may be more likely to keep taking than carbamazepine. Reducing the risk of adverse events and treatment withdrawal is important when selecting an anti-epilepsy drug as it usually will need to be taken long-term.Sep 12, 2017
Is there any permanent treatment for epilepsy?
There's currently no cure for epilepsy, but it can be managed with medications and other strategies.
What is the most common medication for epilepsy?
AEDs are the most commonly used treatment for epilepsy. They help control seizures in around 7 out of 10 of people. AEDs work by changing the levels of chemicals in your brain....Common types include:sodium valproate.carbamazepine.lamotrigine.levetiracetam.topiramate.
What triggers epilepsy?
Triggers are situations that can bring on a seizure in some people with epilepsy. Some people's seizures are brought on by certain situations. Triggers can differ from person to person, but common triggers include tiredness and lack of sleep, stress, alcohol, and not taking medication.Mar 15, 2020
What food should epileptics avoid?
If you have a sudden spike or crash in blood sugar, this could cause seizures. This is why it is generally best to avoid high sugar, processed foods such as cookies, cakes, candy and white bread. Ideally you should aim to follow a balanced diet which will release energy into your bloodstream at a slower, steadier rate.Feb 3, 2022
What is the best vitamin for epilepsy?
Nutrients that may reduce seizure frequency include vitamin B6, magnesium, vitamin E, manganese, taurine, dimethylglycine, and omega-3 fatty acids. Administration of thiamine may improve cognitive function in patients with epilepsy.
Can epilepsy be managed without medication?
For most people with epilepsy seizures last for a short time and stop of their own (without needing medical treatment). Although there is a risk of accident and injury, seizures themselves do not usually cause any lasting harm. However, for some people their seizures can cause serious harm.Feb 16, 2020
What are the treatments for seizures?
For patients with seizures that are not controlled with these agents, alternative treatments include surgical resection of the seizure focus, ketogenic diets, vagus nerve stimulators, and implantable brain neurostimulators.
What are the risk factors for epilepsy in children?
In children, key risk factors are abnormal electroencephalography results, an epileptic syndrome associated with seizures, severe head trauma, and cerebral palsy. The risk of adverse effects from antiepileptic drugs is considerable and includes potential cognitive and behavioral effects. In the absence of risk factors, ...
What are the risk factors for recurrence of seizures?
In adults, key risk factors for recurrence are two unprovoked seizures occurring more than 24 hours apart, epileptiform abnormalities on electroencephalography, abnormal brain imaging, nocturnal seizures, or an epileptic syndrome associated with seizures.
Does epilepsy require antiepileptics?
Epilepsy: Treatment Options. The occurrence of a single seizure does not always require initiation of antiepileptic drugs. Risk of recurrent seizures should guide their use. In adults, key risk factors for recurrence are two unprovoked seizures occurring more than 24 hours apart, epileptiform abnormalities on electroencephalogr ….
What is the diagnosis of epilepsy?
Diagnosis of epilepsy is dependent on history, physical and neurologic examination, labo-ratory testing as indicated, and electroen-cephalography and neuroimaging findings. The history should include events directly preceding the seizure, number of seizures in the past 24 hours, length and description of the seizure, focal aspects, and length of the postictal period. The need for laboratory testing is based on clinical context and may include blood glucose, blood counts, elec-trolyte panels (particularly sodium), lum-bar puncture in febrile patients, and urine toxicology (Figure 1). Electroencephalogra-phy should be used to confirm, but not to exclude, a diagnosis of epilepsy.12,13 Evalu-ation of a patient who has experienced a first seizure has previously been reviewed, including in American Family Physician.12-14
How many people with epilepsy have refractory seizures?
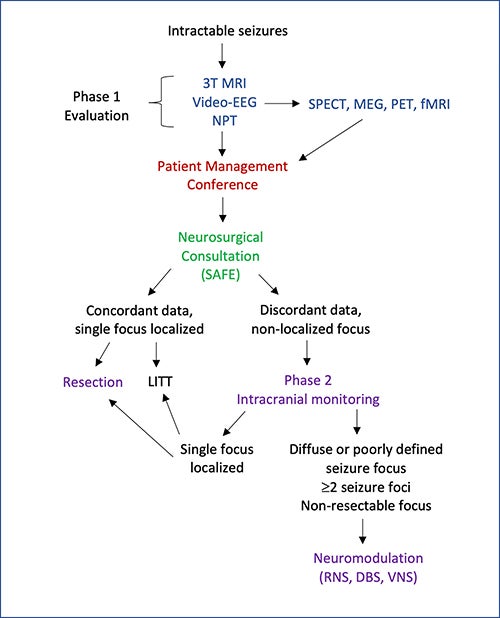
Up to 30% of patients with epilepsy can have medically refractory epilepsy. These patients have continued sei-zures despite appropriate AED therapy.30 Surgical resec-tion of the seizure focus in appropriately selected patients often results in decreased frequency or elimination of seizures with improvement in quality of life. Seizure free-dom is achieved in up to 76% of patients after resection.31Factors associated with seizure freedom after surgery include seizures without loss of consciousness, complete or extensive resection of the lesion, and prolonged febrile sei-zures. The possibility of recurrence decreases with increas-ing postoperative seizure-free intervals. Factors associated with postoperative recurrence include nonlesional (non-structural) epilepsy, normal magnetic resonance imaging, preoperative generalized tonic-clonic seizures, and infan-tile spasms or tonic seizures. Also, the need for invasive intracranial electroencephalography monitoring to deter-mine seizure focus predicts a worse outcome.31Cognitive deficits are common following surgery and depend on the site of the resection. Left temporal lobe resection is associated with verbal memory deficits (44%) and naming deficits (34%). After a right tempo-ral lobe resection, verbal memory deficits are also com-mon (20%). Operative mortality in most centers is below 0.5%. Lower mortality is associated with procedures lim-ited to the temporal lobe. Other adverse effects include neurologic deficits (5%), medical complications (e.g., intracerebral infection, hydrocephalus; 1.5%), cerebro-spinal fluid leak (8.5%), aseptic meningitis (3.6%), and noncerebral bacterial infections (3%). Other medical problems such as hemorrhage, pneumonia, and deep venous thrombosis are uncommon (2.5%).13,21,32
What is the procedure to remove a part of the brain that causes seizures?
There are two main kinds: Resective surgery. The surgeon will remove the part of your brain that causes the seizures. This surgery is most often done when the part of the brain causing the seizures is very small, has very good boundaries, and doesn’t control things like your speech, movement, sight, or hearing.
What is the medication called that changes the way the brain works?
Epilepsy medications, sometimes called anti-seizure or anticonvulsant medications, change the way your brain cells work and send messages to each other. The kind of medication your doctor suggests depends on a few things: The type of seizures you have. How likely it is you’ll have more seizures. Your age. Your sex.
How to get off medication?
How to Get Off Your Medication. Ketogenic Diet. Nerve Stimulation. Surgery. After you’re diagnosed with epilepsy, you have several ways to get treatment. Medication, a special diet, an implant that works on your nerves or brain, and surgery could all help you feel better.
Can a teenager have seizures?
Some types of seizures only happen in children and younger teenagers. If you’re an older teenager or young adult, your doctor might think it’s safe for you to stop your medication. This diet is high in fats and low in carbohydrates. Your doctor may suggest it, depending on the type of seizures you have.
Do you need a blood test for epilepsy?
While you’re taking it, the doctor will want you to get blood tests to see how your body handles the treatment. How often you need them depends on your type of epilepsy medication, other drugs you take, and any health conditions you might have.
Can you take more than one medication for epilepsy?
Drugs that work for one person might not work for another. You might have to try more than one. Most people who take medication for epilepsy find a good fit on the first or second try. You might have to start with a low dose and slowly add more. It depends which medication you take.
What are the different types of epilepsy treatments?
There are a wide range of epilepsy treatments, with most falling into one of four categories: medication, diet, implanted devices, and surgeries. Before recommending a course of treatment, a physician will take into account age, overall health, medical history, severity of condition, and type or types of seizure.
What are some ways to help someone with epilepsy?
Other Treatments. Some people with epilepsy try natural or alternative treatments. Some report improvements when they use medical cannabis, melatonin, or complementary therapies such as acupuncture, herbal or nutritional supplements, chiropractic treatments, and mind-body practices such as meditation.
What is the most common type of neurosurgery for epilepsy?
Epilepsy surgeries fall into two general categories: resection and disconnection. The most common type of neurosurgery for epilepsy is resection , in which the portion of the brain causing seizures is removed. If successful, the surgery can provide long-term remission from seizures.
What is an implanted device for epilepsy?
Implanted Devices. Some people with intractable epilepsy may be candidates for an implanted device such as a vagus nerve stimulator (VNS) or a responsive neurostimulation system (RNS). To be eligible, people must generally be 12 years or older and have tried several AEDs.
Why are seizures so difficult to treat?
Some epilepsies and seizure types are more difficult to treat because they are less responsive to most treatments. In most cases, a medication will be the first treatment prescribed. On average, anti-epileptic drugs (AEDs) will work for 70 percent of people with epilepsy.
What is the keto diet for epilepsy?
The ketogenic diet, used to treat children with refractory epilepsy, is an extreme diet involving fasting and monitoring by a physician and a nutritionist. The purpose of the diet is to force the body to burn fat for energy instead of carbohydrates, increasing the level of molecules called ketones in the blood.
What is the broad spectrum of anticonvulsants?
Broad-spectrum anticonvulsants include Depakote (Valproic acid), Keppra (Levetiracetum), Lamictal (Lamotrigine), Topamax (Topiramate), and Zonegran (Zonisamide). Apart from AEDs, other classes of drugs may be prescribed to control seizures. For instance, Klonopin (Clonazepam) is a sedative of the benzodiazepine class used to treat Lennox-Gastaut ...
What is the treatment for a seizure?
Treatment should begin with monotherapy. The appropriate choice of medication varies depending on seizure type. Routine monitoring of drug levels is not correlated with reduction in adverse effects or improvement in effectiveness and is not recommended.
What activities should an epilepsy patient participate in?
Patients with epilepsy should be encouraged to participate in physical activity and sports. Regular physical activity, in addition to providing cardiovascular and psychological benefits, may decrease seizure frequency. 57 Patients may participate in most sports, including bicycling, contact sports, and swimming, assuming seizures are well controlled and supervision is available. High-risk sports where a seizure may result in severe injury or death, such as hang-gliding, scuba diving, and free climbing, are not recommended. 58 Information about sports activities for children with epilepsy is available at http://www.epilepsy.com/learn/seizures-youth/about-kids/playing-sports-and-other-activities.
What is the risk of recurrent seizures?
Adults at high risk of recurrent seizures should receive AED therapy. High-risk characteristics include two unprovoked seizures occurring more than 24 hours apart; one unprovoked seizure and an assessment that predicts an increased probability of further seizures based on underlying cause and seizure characteristics; or a diagnosis of an epilepsy syndrome in which recurrent seizures are a prominent feature ( http://www.epilepsy.com/learn/types-epilepsy-syndromes ). Epileptiform abnormalities on electroencephalography also predict a high risk of recurrence (60% over 10 years), as does abnormal brain imaging or a nocturnal seizure. 8 – 10, 15 – 18 Adults should be counseled that the cumulative risk of a recurrent seizure after a first unprovoked seizure is approximately 50% over five years, with one-third of the risk accruing in the first year. In persons 65 years and older, the risk of recurrence following a first unprovoked seizure is 53% within one year (lifetime risk is 80%). 16 Initiating AED therapy after the first seizure decreases the absolute risk of recurrence by 35% over the next two years. AED therapy is almost always indicated after two unprovoked seizures occurring more than 24 hours apart because of the high recurrence rate (32% at three months, 57% at one year, 73% at four years). AEDs may not improve quality of life and prognosis for sustained seizure remission. The risk of an adverse effect from an AED ranges from 7% to 31%. 16 – 18
How many people with epilepsy have refractory seizures?
Up to 30% of patients with epilepsy can have medically refractory epilepsy. These patients have continued seizures despite appropriate AED therapy. 30 Surgical resection of the seizure focus in appropriately selected patients often results in decreased frequency or elimination of seizures with improvement in quality of life. Seizure freedom is achieved in up to 76% of patients after resection. 31
What is the risk of sudden death in epilepsy?
A significant risk factor for SUDEP is nocturnal seizures. Although rare in children, SUDEP is the leading cause of epilepsy-related death among young adults with uncontrolled epilepsy, occurring in nine per 1,000 persons with epilepsy overall, but as many as one in 150 persons with poor seizure control. 20, 21 The risk of SUDEP can be decreased by optimizing seizure control. 22, 23
What is the diagnosis of epilepsy?
Diagnosis of epilepsy is dependent on history, physical and neurologic examination, laboratory testing as indicated, and electroencephalography and neuroimaging findings. The history should include events directly preceding the seizure, number of seizures in the past 24 hours, length and description of the seizure, focal aspects, and length of the postictal period. The need for laboratory testing is based on clinical context and may include blood glucose, blood counts, electrolyte panels (particularly sodium), lumbar puncture in febrile patients, and urine toxicology ( Figure 1). Electroencephalography should be used to confirm, but not to exclude, a diagnosis of epilepsy. 12, 13 Evaluation of a patient who has experienced a first seizure has previously been reviewed, including in American Family Physician. 12 – 14
What are the risk factors for epilepsy in children?
In children, key risk factors are abnormal electroencephalography results, an epileptic syndrome associated with seizures, severe head trauma, and cerebral palsy. The risk of adverse effects from antiepileptic drugs is considerable and includes potential cognitive and behavioral effects. In the absence of risk factors, ...
What is the diagnosis of epilepsy?
A doctor makes his or her epilepsy diagnosis based on symptoms, physical signs and the results of such tests as an electroencephalogram (EEG), computed tomography (CT or CAT scan) or magnetic resonance imaging (MRI). It is essential that the type of epilepsy and the type of seizures both are diagnosed properly.
What is epilepsy disorder?
Check out the new videos at the bottom of the page. Epilepsy is a disorder of the brain characterized by repeated seizures. A seizure is usually defined as a sudden alteration of behavior due to a temporary change in the electrical functioning of the brain.
What are the two types of seizures?
Typically, seizures belong in one of two basic categories: primary generalized seizures and partial seizures. The difference between these types is in how they begin.
What percentage of epilepsy patients have intractable seizures?
According to the National Institute of Neurological Disorders and Stroke, 20 percent of epilepsy patients have intractable seizures — seizures that do not respond to treatment. The reasons why epilepsy begins are different for people of different ages.
How does epilepsy affect the brain?
In epilepsy the brain's electrical rhythms have a tendency to become imbalanced, resulting in recurrent seizures.
How many people have epilepsy?
According to the Epilepsy Foundation, epilepsy affects three million people in the U.S. and 50 million worldwide. Epileptic seizures may be tied to a brain injury or genetics, but for 70 percent of epilepsy patients, the cause is unknown.
What causes epilepsy in children?
Children may be born with a defect in the structure of their brain or they may suffer a head injury or infection that causes their epilepsy. Severe head injury is the most common known cause in young adults. For middle-age individuals, strokes, tumors and injuries are more frequent catalysts.
Treatment
- Doctors generally begin by treating epilepsy with medication. If medications don't treat the condition, doctors may propose surgery or another type of treatment.
Clinical Trials
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and Home Remedies
- Understanding your condition can help you take better control of it: 1. Take your medication correctly.Don't adjust your dosage before talking to your doctor. If you feel your medication should be changed, discuss it with your doctor. 2. Get enough sleep.Lack of sleep can trigger seizures. Be sure to get adequate rest every night. 3. Wear a medical alert bracelet.This will help emergency …
Coping and Support
- Uncontrolled seizures and their effects on your life may at times feel overwhelming or lead to depression. It's important not to let epilepsy hold you back. You can still live an active, full life. To help cope: 1. Educate yourself and your friends and familyabout epilepsy so that they understand the condition. 2. Try to ignore negative reactions from people.It helps to learn about epilepsy so …
Preparing For Your Appointment
- You're likely to start by seeing your family doctor or a general practitioner. However, in some cases when you call to set up an appointment, you may be referred immediately to a specialist, such as a doctor trained in brain and nervous system conditions (neurologist) or a neurologist trained in epilepsy (epileptologist). Because appointments can be brief, and because there's ofte…