Nutrition
5 rows · The 4-month TB treatment regimen (high-dose daily rifapentine with moxifloxacin, isoniazid, and ...
How long will my tuberculosis take to get cured?
Treatment. impurities in rifampin and rifapentine, two important anti-tuberculosis (TB) medications. People with TB disease or latent TB infection taking rifampin or rifapentine should continue taking their current medication, and should …
What medications are used to treat tuberculosis?
Nov 24, 2020 · TB disease is curable. It is treated by a standardized course of treatment usually including 4 antibacterial medicines. In some cases the TB bacteria does not respond to the standard drugs. In this case, the patient has drug-resistant TB. Treatment for drug-resistant TB is longer and more complex.
How can you cure tuberculosis?
Apr 08, 2020 · The most common treatment for active TB is isoniazid INH in combination with three other drugs—rifampin, pyrazinamide and ethambutol. You may begin to feel better only a few weeks after starting to take the drugs but treating TB …
How to cure TB naturally?
Oct 27, 2016 · Evaluation of shorter treatment regimens to make it easier for people to complete drug therapy Inclusion of antibiotics that are already available for treatment of other infections and have been shown to act on Mycobacterium tuberculosis may make therapy more potent and easier to tolerate
See more
The overall goals for treatment of tuberculosis are 1) to cure the individual patient, and 2) to minimize the transmission of Mycobacterium tuberculosis to other persons. Thus, successful treatment of tuberculosis has benefits both for the individual patient and the community in which the patient resides.

What is first line treatment for TB?
Which is best medicine for TB?
How is TB treated at home?
- Foods rich in vitamins A, C, B complex and E. ...
- Protein-rich food. ...
- Foods that are a storehouse of Zinc. ...
- Calorie dense food. ...
- Garlic. ...
- Mint. ...
- Black pepper.
How many types of TB treatments are there?
Is TB curable today?
What are the 3 types of tuberculosis?
Which food is not good for TB patients?
Limit intake of refined carbs such as maida and sugar-laden foods as they offer only empty calories devoid of nutrients. Deep-fried foods and junk foods packed with saturated fats and trans-fat would worsen symptoms associated with TB such as diarrhoea, abdominal cramps, and fatigue.Aug 11, 2021
How do u know if u have TB?
Can we sleep with TB patient?
Is there a vaccine for tuberculosis?
Bacille Calmette-Guérin (BCG) is a vaccine for tuberculosis (TB) disease. This vaccine is not widely used in the United States. However, it is often given to infants and small children in other countries where TB is common.
What is #3 TB?
What is the name of TB medication?
How long does it take to treat TB?
TB disease can be treated by taking several drugs for 6 to 9 months. There are 10 drugs currently approved by the U.S. Food and Drug Administration (FDA) for treating TB. Of the approved drugs, the first-line anti-TB agents that form the core of treatment regimens are: isoniazid (INH) rifampin (RIF)
What is drug resistant TB?
Drug-resistant TB is caused by TB bacteria that are resistant to at least one first-line anti-TB drug. Multidrug-resistant TB (MDR TB) is resistant to more than one anti-TB drug and at least isoniazid (INH) and rifampin (RIF).
What is XDR TB?
Extensively drug-resistant TB (XDR TB) is a rare type of MDR TB that is resistant to isoniazid and rifampin, plus any fluoroquinolone and at least one of three injectable second-line drugs (i.e., amikacin, kanamycin, or capreomycin). Treating and curing drug-resistant TB is complicated.
How is treatment completion determined?
Treatment completion is determined by the number of doses ingested over a given period of time.
What is it called when TB bacteria multiply?
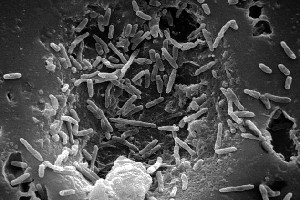
When TB bacteria become active (multiplying in the body) and the immune system can’t stop the bacteria from growing, this is called TB disease. TB disease will make a person sick. People with TB disease may spread the bacteria to people with whom they spend many hours.
Can TB be treated?
It is very important that people who have TB disease are treated, finish the medicine, and take the drugs exactly as prescribed. If they stop taking the drugs too soon, they can become sick again; if they do not take the drugs correctly, the TB bacteria that are still alive may become resistant to those drugs.
Is TB a serious disease?
TB is a serious disease, and can be fatal if not treated properly. It is important to remember that all medications have risks and benefits. Learn more from CDC’s Dear Colleague letter. Not everyone infected with TB bacteria becomes sick. As a result, two TB-related conditions exist: latent TB infection and TB disease.
Can latent TB be fatal?
Without treatment latent TB infection can progress to TB disease. If not treated properly, TB disease can be fatal.
Can rifampin be used for TB?
Treatment. impurities in rifampin and rifapentine, two important anti-tuberculosis (TB) medications. People with TB disease or latent TB infection taking rifampin or rifapentine should continue taking their current medication, and should talk with their healthcare provider about any concerns.
What is the best treatment for TB?
The most common treatment for active TB is isoniazid INH in combination with three other drugs—rifampin, pyrazinamide and ethambutol. You may begin to feel better only a few weeks after starting to take the drugs but treating TB takes much longer than other bacterial infections.
How long does it take to treat TB?
The treatment for this type of TB takes much longer, 20 to 30 months to complete, and you may experience more side effects.
What is DOT therapy?
This means a healthcare worker will come to you to administer your medication and eliminate the concern of forgetting to take the treatment.
What are the side effects of TB?
While you are in treatment for active TB disease, you will need regular checkups to make sure your treatment is working. Everyone is different, but there are side effects associated with taking the medications, including: 1 Upset stomach, nausea and vomiting or loss of appetite 2 Tingling or numbness in the hands or feet 3 Itchy skin, rashes or bruising 4 Changes in your eyesight or blurred visions 5 Yellowish skin or eyes 6 Dark-colored urine 7 Weakness, fatigue or fever that for three or more days
What are the symptoms of TB?
Yellowish skin or eyes. Dark-colored urine. Weakness, fatigue or fever that for three or more days. It is important to tell your doctor or TB nurse immediately if you begin having any unusual symptoms while taking medicine for either preventive therapy or for active TB disease.
What to take for TB tingling?
If you are having trouble with tingling and numbness, your doctor may prescribe a vitamin B6 supplement while you are in treatment. It may also be possible to change TB medications if your side effects are serious.
Can you get TB from taking too much medicine?
You must finish your medicine and take the drugs exactly as prescribed. If you stop taking the drugs too soon you can become sick again and potentially spread the disease to others. Additionally, by taking the drugs incorrectly, TB germs that are still alive may become drug-resistant, making it harder for you to get better next time.
What is the most successful treatment for tuberculosis?
Treatment of patients with tuberculosis is most successful within a comprehensive framework that addresses both clinical and social issues of relevance to the patient. It is essential that treatment be tailored and supervision be based on each patient's clinical and social circumstances (patient-centered care). Patients may be managed in the private sector, by public health departments, or jointly, but in all cases the health department is ultimately responsible for ensuring that adequate, appropriate diagnostic and treatment services are available, and for monitoring the results of therapy.
What are the goals of tuberculosis treatment?
The overall goals for treatment of tuberculosis are 1) to cure the individual patient, and 2) to minimize the transmission of Mycobacterium tuberculosis to other persons. Thus, successful treatment of tuberculosis has benefits both for the individual patient and the community in which the patient resides.
Why are antituberculosis drugs needed?
New antituberculosis drugs are needed for three main reasons: 1) to shorten or otherwise simplify treatment of tuberculosis caused by drug-susceptible organisms, 2) to improve treatment of drug-resistant tuberculosis, and 3) to provide more efficient and effective treatment of latent tuberculosis infection.
How many subpopulations of tuberculosis are there?
It is theorized that there are three separate subpopulations of M. tuberculosis within the host. These populations are defined by their growth characteristics and the milieu in which they are located ( 1 ). The largest of the subpopulations consists of rapidly growing extracellular bacilli that reside mainly in cavities. This subpopulation, because of its size, is most likely to harbor organisms with random mutations that confer drug resistance. The frequency of these mutations that confer resistance is about 10 -6 for INH and SM, 10 -8 for RIF, and 10 -5 for EMB; thus, the frequency of concurrent mutations to both INH and RIF, for example, would be 10 -14, making simultaneous resistance to both drugs in an untreated patient a highly unlikely event ( 2 ).
What is the purpose of chemo for tuberculosis?
As noted previously, antituberculosis chemotherapy is both a personal health measure intended to cure the sick patient and a basic public health strategy intended to reduce the transmission of Mycobacterium tuberculosis. Typically, tuberculosis treatment is provided by public health departments, often working in collaboration with other providers and organizations including private physicians, community health centers, migrant health centers, correctional facilities, hospitals, hospices, long-term care facilities, and homeless shelters. Private providers and public health departments may cosupervise patients, assuring that the patient completes therapy in a setting that is not only mutually agreeable but also enables access to tuberculosis expertise and resources that might otherwise not be available. In managed care settings delivery of tuberculosis treatment may require a more structured public/private partnership, often defined by a contract, to assure completion of therapy. Regardless of the means by which treatment is provided, the ultimate legal authority for assuring that patients complete therapy rests with the public health system.
Why is it important to obtain sputum cultures at the time of completion of the initial phase of treatment?
Emphasis is placed on the importance of obtaining sputum cultures at the time of completion of the initial phase of treatment in order to identify patients at increased risk of relapse.
Is tuberculosis treated with HIV?
Treatment of tuberculosis in patients with HIV infection follows the same principles as treatment of HIV-uninfected patients. However, there are several important differences between patients with and without HIV infection. These differences include the potential for drug interactions, especially between the rifamycins and antiretroviral agents, paradoxical reactions that may be interpreted as clinical worsening, and the potential for the development of acquired resistance to rifamycins when treated with highly intermittent therapy.
What are the drugs that treat TB?
Food and Drug Administration (FDA) for the treatment of TB disease (Table 6.2). In addition, the fluoroquinolones (levofloxacin, moxifloxacin, and gatifloxacin), although not approved by the FDA for TB disease, are commonly used to treat TB disease caused by drug-resistant organisms or for patients who are intolerant of some first-line drugs. Rifabutin, approved for use in preventing Mycobacterium avium complex disease in patients with HIV infection but not approved for TB disease, is useful for treating TB disease in patients concurrently taking drugs that interact with rifampin (e.g., certain antiretroviral drugs). Amikacin and kanamycin, nearly identical aminoglycoside drugs used in treating patients with TB disease caused by drug-resistant organisms, are not approved by the FDA for treatment of TB.
How long does it take to treat TB?
As a general rule, the principles used for the treatment of pulmonary TB disease also apply to extrapulmonary forms of the disease. A 6-month treatment regimen is recommended for patients with extrapulmonary TB disease, unless the organisms are known or strongly suspected to be resistant to the first-line drugs. If PZA cannot be used in the initial phase, the continuation phase must be increased to 7 months. The exception to these recommendations is central nervous system TB, for which the optimal length of therapy has not been established but some experts recommend 9 to 12 months. Most experts do recommend corticosteroids to be used as additional therapy for patients with TB meningitis and pericarditis. Consultation with a TB expert is recommended.
What are the four drugs that are included in the initial treatment regimen?
Four drugs— INH, RIF, PZA, and EMB — should be included in the initial treatment regimen until the results of drug-susceptibility tests are available. Each of the drugs in the initial regimen plays an important role. INH and RIF allow for short-course regimens with high cure rates. PZA has potent sterilizing activity, which allows further shortening of the regimen from 9 to 6 months. EMB helps to prevent the emergence of RIF resistance when primary INH resistance is present. If drug-susceptibility test results are known and the organisms are fully susceptible, EMB need not be included. For children whose clarity or sharpness of vision cannot be monitored, EMB is usually not recommended except when the risk of drug resistance is high or for children who have “adult-type” (upper lobe infiltration, cavity formation) TB disease.
How long is the TB continuation phase?
The continuation phase of treatment is given for either 4 or 7 months. The 4-month continuation phase should be used in patients with uncomplicated, noncavitary, drug-susceptible TB, if there is documented sputum conversion within the first 2 months. The 7-month continuation phase is recommended only for
What is the recommended treatment regimen based on?
The recommended treatment regimens are based, in large part, on evidence from clinical trials and are rated on the basis of a system developed by the U.S. Public Health Service (USPHS) and the Infectious Diseases Society of America (IDSA) (Table 6.3).
How to educate patients about TB?
Educating patients about TB disease helps ensure their successful completion of therapy. Health-care providers must take the time to explain clearly to patients what medication should be taken, how much, how often, and when. Patients should be clearly informed about possible adverse reactions to the medications they are taking and when to seek necessary medical attention. Providing patients with the knowledge they need regarding the consequences of not taking their medicine correctly is very important. In addition, patients should be educated about infection control measures and potential need for isolation (Table 6.1). HIV testing and counseling is recommended for all patients with TB disease in all health-care settings. The patient must first be notified that testing will be performed. The patient has the right to decline HIV testing and counseling (opt-out screening).
How long does it take to develop a TB control plan?
For each patient with newly diagnosed TB disease, a specific treatment and monitoring plan should be developed in collaboration with the local TB control program within 1 week of the presumptive diagnosis. This plan should include: