Treatment of patients with septic shock has the following major goals:
- Start adequate antibiotics (proper spectrum and dose) as early as possible
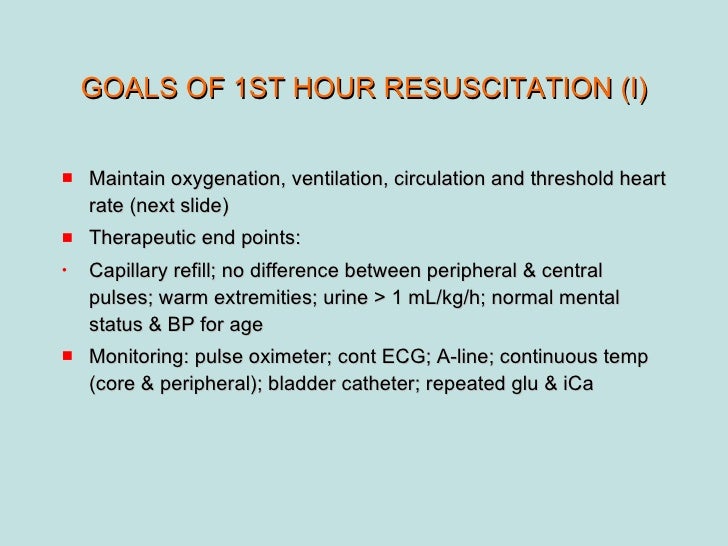
- Resuscitate the patient from septic shock by using supportive measures to correct hypoxia, hypotension, and impaired...
- Identify the source of infection and treat with antimicrobial therapy, surgery, or both (source control)
What is the primary goal of shock management?
Management of Shock. Please purchase the course before starting the lesson. Getting oxygen to the organs and tissues is the primary goal of shock management. To achieve this, the blood must have enough oxygen, it must be able to get to the tissues, and the vasculature must have the blood kept within it.
What are interim goals for treatment of shock?
Interim goals for treatment for shock are to augment perfusion and oxygen delivery and minimize organ damage until the body's natural homeostatic mechanisms return. While simple in theory, the complexity of the body's response to shock and its therapies can make realtime goal-directed management of shock surprisingly challenging.
What are the goals of treatment for septic shock?
Treatment of patients with septic shock has the following major goals: Start adequate antibiotics (proper spectrum and dose) as early as possible Resuscitate the patient from septic shock by using supportive measures to correct hypoxia, hypotension, and impaired tissue oxygenation (hypoperfusion)
What are the nursing goals of care for patients in shock?
When caring for a patient in shock, one of the major nursing goals is to reduce the risk that the patient will develop complications of shock. How can the nurse best achieve this goal?

What are the four basic principles for treatment of shock?
These four phases are the resuscitation phase, the optimization phase, the stabilization phase and the evacuation phase.
What are the 3 steps in the treatment of shock?
Shock TreatmentCall 911.Lay the Person Down, if Possible.Begin CPR, if Necessary.Treat Obvious Injuries.Keep Person Warm and Comfortable.Follow Up.
What is the 1st priority in treating shock?
Shock requires emergency medical treatment. The first priority is to get blood pressure back up to normal. This may be done by giving blood and fluids through a vein. Blood-pressure-raising medicines may be administered.
What is the priority treatment for most types of shock?
Getting oxygen to the organs and tissues is the primary goal of shock management. To achieve this, the blood must have enough oxygen, it must be able to get to the tissues, and the vasculature must have the blood kept within it. Achieving these three important goals is the priority of shock management.
What are the methods of shock treatment?
Shock factsSeptic shock is treated with antibiotics and fluids.Anaphylactic shock is treated with diphenhydramine (Benadryl), epinephrine (an "Epi-pen"), and steroid medications (solumedrol).Cardiogenic shock is treated by identifying and treating the underlying cause.More items...
What are the nursing management of shock?
Nursing care focuses on assisting with treatment targeted at the cause of the shock and restoring intravascular volume. Safe administration of blood. It is important to acquire blood specimens quickly, to obtain baseline complete blood count, and to type and crossmatch the blood in anticipation of blood transfusions.
What are the 4 goals of first aid?
We define first aid as helping behaviors and initial care provided to a person for an acute illness or injury. The goals of a first aid provider include preserving life, alleviating suffering, preventing further illness or injury, and promoting recovery.
How do you help someone in shock after an accident?
use a coat or blanket to keep them warm. do not give them anything to eat or drink. give them lots of comfort and reassurance. monitor the person – if they stop breathing, start CPR and call 999 to update them.
How do Emts treat shock?
Treat the effects of shock with oxygen, IV fluid administration and medications to maintain critical body systems.
What is the primary therapy for hypovolemic shock?
The main treatment for the critically-ill child with hypovolemic shock is fluid resuscitation. Fluid resuscitation consists of rapid boluses of isotonic crystalloid IV fluids (NS-normal saline or LR-lactated Ringer's). This treatment is primarily focused on correcting the intravascular fluid volume loss.
What is the primary goal of fluid resuscitation in hemorrhagic shock?
Fluid resuscitation in CHS is aimed toward normalization of hemodynamic parameters, in contrast to UCHS, where hemostasis cannot be safely achieved, and early rapid evacuation to a surgical facility is considered the most important step of management after the airway and breathing have been secured.
What is the most important step in the specific emergency treatment for hypovolemic shock?
Three goals exist in the emergency department treatment of the patient with hypovolemic shock as follows: (1) maximize oxygen delivery - completed by ensuring adequacy of ventilation, increasing oxygen saturation of the blood, and restoring blood flow, (2) control further blood loss, and (3) fluid resuscitation.
What is the primary goal of shock management?
Getting oxygen to the organs and tissues is the primary goal of shock management. To achieve this, the blood must have enough oxygen, it must be able to get to the tissues, and the vasculature must have the blood kept within it. Achieving these three important goals is the priority of shock management.
What is the procedure for obstructive shock?
Rapid and definitive care must be administered to causes of obstructive shock, as they are acutely life-threatening. Pericardial drainage is a requirement of cardiac tamponade. Needle decompression and subsequent placement of a chest tube (tube thoracotomy) is required by tension pneumothorax. Vascular abnormalities can be addressed by pediatric heart surgeons, and administering prostaglandin E1 analogs can result in ductus arteriosus into being induced to remain open. Trained personnel can administer anticoagulant agents and fibrinolytic, though pulmonary embolism care is mostly supportive. The scope of this handbook does not cover the management of these complex etiologies.
What is the first line of treatment for cardiogenic shock?
A primary intervention in cardiogenic shock is not fluid resuscitation, unlike with most other types of shock. First-line treatments often include medications that reduce afterload and support contractility. This means diuretics and vasodilators in normotensive persons, as both decrease intravascular volume.
How to manage distributive shock?
Increasing intravascular volume is the initial management of distributive shock. The intent is to overcome the inappropriate redistribution of existing volume by providing enough volume. Administer 20 mL/kg of fluids as a bolus over 5 to 10 minutes, just like hypovolemic shock, and repeat when necessary. Therapy is tailored to the cause of the distributive shock beyond initial management.
How to know if you have neurogenic shock?
A clinical sign of neurogenic shock is bradycardia or an inappropriately low pulse. Reassess the person for a response after an initial treatment focusing on fluids first: 20 mL/kg bolus over 5 to 10 minutes. Vasopressors are required if fluid resuscitation does not cause a response in hypotension. A broader neurological evaluation and treatment plan should be done together with this resuscitation.
What is the first treatment for anaphylactic shock?
The first and most important treatment for anaphylactic shock is intramuscular epinephrine. Intravenous administration or a second dose of epinephrine may be required in severe cases. Administer crystalloid fluid judiciously. Capillary permeability may increase significantly while in anaphylactic shock.
How to treat septic shock?
A key intervention that should be administered immediately is the use of broad-spectrum intravenous antibiotics. Additionally, to support blood pressure, you may need to also employ vasopressors and a stress dose of hydrocortisone (especially with adrenal insufficiency). Depending on the type of septic shock, vasopressors may be given if necessary after fluid resuscitation. Epinephrine treats cold shock, norepinephrine treats warm shock, and dopamine is usually given to normotensive persons. Decreased oxygen-carrying capacity is treated by transfusing packed red blood cells to bring hemoglobin above 10 g/dL. Focus antibiotic therapy to the particular microbe and its resistance patterns as blood cultures return.
How to treat septic shock?
Treatment of patients with septic shock has the following major goals: 1 Start adequate antibiotics (proper spectrum and dose) as early as possible 2 Resuscitate the patient from septic shock by using supportive measures to correct hypoxia, hypotension, and impaired tissue oxygenation (hypoperfusion) 3 Identify the source of infection and treat with antimicrobial therapy, surgery, or both (source control) 4 Maintain adequate organ system function, guided by cardiovascular monitoring, and interrupt the progression of MODS
How to resuscitate a patient from septic shock?
Resuscitate the patient from septic shock by using supportive measures to correct hypoxia, hypotension, and impaired tissue oxygenation (hypoperfusion)
What is ARDS in septic shock?
Acute respiratory distress syndrome (ARDS), commonly observed in septic shock as a part of multiorgan failure syndrome, results in pathologically diffuse alveolar damage (DAD). This is a high-powered photomicrograph of early stage (exudative stage) DAD.
What is the goal of shock management?
The goal of shock management is to get oxygen to the tissues and to the organs. This requires having enough oxygen in the blood, getting the blood to the tissues, and keeping the blood within the vasculature. Thus, shock management is dedicated to achieving these three critical goals. In objective terms, this means returning the person to ...
How to manage distributive shock?
The intent is to provide enough volume to overcome the inappropriate redistribution of existing volume. As with hypovolemic shock, administer 20 mL/kg of fluid as a bolus over 5 to 10 minutes and repeat as needed. Beyond initial management, therapy is tailored to the cause of the distributive shock.
How to treat cardiac shock in children?
Since children in cardiogenic shock have a problem with cardiac contractility, the primary goal of therapy is to restore contractility. Unlike most other types of shock, fluid resuscitation is not a primary intervention in cardiogenic shock. Often medications to support contractility and reduce afterload are first-line treatments. In normotensive persons, this means vasodilators and diuretics (both decrease intravascular volume). Contractility is supported with inotropes. Milrinone is often used to decrease peripheral vascular resistance. When additional volume is needed, fluid can be administered slowly and cautiously: 5 to 10 mL/kg over 10 to 20 minutes. A pediatric cardiologist or critical care specialist should manage persons with cardiogenic shock.
How to respond to hypovolemic shock?
The primary means of responding to hypovolemic shock is to provide additional volume. For children, an isotonic crystalloid such as normal saline or Lactated Ringer’s is the preferred fluid for volume resuscitation. While volume repletion is somewhat straightforward in adults, great care must be taken when administering intravenous fluids to children and infants. Careful estimates should be made concerning the amount of volume lost (e.g. blood loss), the size of the person, and the degree of deficit. Current recommendations are to administer 20 mL/kg of fluid as a bolus over 5 to 10 minutes and repeat as needed. In hypovolemic (or hemorrhagic) shock, administer 3 mL of fluid for every 1 mL of estimated blood lost—a 3:1 ratio. If fluid boluses do not improve the signs of hypovolemic, hemorrhagic shock, consider the administration of packed red blood cells without delay. Albumin can also be considered for additional intravenous volume for shock, trauma, and burns as a plasma expander. If fluid boluses do not improve the signs of hypovolemic, hemorrhagic shock, re-evaluation of proper diagnosis and occult blood loss (e.g. into the GI tract) should be considered. The remaining interventions are aimed at restoring electrolyte imbalances (e.g. acid/base, glucose, etc.).
What is the treatment for septic shock?
In septic shock, aggressive fluid management is generally necessary. Broad-spectrum intravenous antibiotics are a key intervention and should be administered as soon as possible. In addition, a stress dose of hydrocortisone (especially with adrenal insufficiency) and vasopressors may be needed to support blood pressure. After fluid resuscitation, vasopressors are given if needed and according to the type of septic shock. Normotensive persons are usually given dopamine, warm shock is treated with norepinephrine, and cold shock is treated with epinephrine. Transfusing packed red blood cells to bring hemoglobin above 10 g/dL treats decreased oxygen-carrying capacity. As blood cultures return, focus antibiotic therapy to the particular microbe and its resistance patterns.
What is the best treatment for anaphylactic shock?
Intramuscular epinephrine is the first and most important treatment for anaphylactic shock. In severe cases, a second dose of epinephrine may be needed or intravenous administration may be required. Crystalloid fluid can be administered judiciously. Remember that in anaphylactic shock, capillary permeability may increase considerably. Thus, while it is important to support blood pressure overall, there is significant likelihood that third spacing and pulmonary edema will occur. Antihistamines and corticosteroids can also blunt the anaphylactic response. If breathing challenges arise, consider albuterol use to achieve bronchodilation. In very severe cases of anaphylactic shock, a continuous epinephrine infusion in the Neonatal Intensive Care Unit (NICU) or Pediatric Intensive Care Unit (PICU) may be required.
What is given after fluid resuscitation?
After fluid resuscitation, vasopressors are given if needed and according to the type of septic shock. Normotensive persons are usually given dopamine, warm shock is treated with norepinephrine, and cold shock is treated with epinephrine.
Full text
Full text is available as a scanned copy of the original print version. Get a printable copy (PDF file) of the complete article (759K), or click on a page image below to browse page by page. Links to PubMed are also available for Selected References.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
What is shock in medical terms?
Shock is acute circulatory failure threatening multiple organ systems and producing a grave threat to survival. Most patients will be hypotensive (mean arterial blood pressure [MAP] < 60 mm Hg) and are often tachycardic, tachypneic, and exhibit overt end-organ dysfunction, such as oliguria, encephalopathy, or lactic acidosis ( Table 21–1 ). The basis for shock may be readily evident from the presentation, such as following trauma, or when symptoms or signs of hemorrhage, fluid loss, or sepsis are evident. A subset of shock patients will have normal blood pressure (even hypertension is possible); many will also lack tachycardia. In such patients, the diagnosis may be challenging, especially since there is such interindividual variance in normal values for blood pressure. Subtle or atypical presentations of shock may require a high index of clinical suspicion. Initially, shock is reversible, but rapidly progresses to cellular injury, cell death, failure of critical organ systems, and an irreversible state that terminates in death. Timely resuscitation blunts inflammation and mitochondrial damage, potentially reducing the burden of early and late morbidity. Because delays in resuscitation may be lethal, shock demands prompt diagnosis and urgent resuscitation.
What are the different types of shock?
Shock is divided into three types: hypovolemic, cardiogenic, or distributive. In a patient with new-onset shock, it is usually possible to categorize the type of shock within minutes based on a concise history and targeted examination.
What is NIRS in septic shock?
The continuous measurement of oxyhemoglobin saturation in thenar capillaries by near-infrared spectroscopy (NIRS) has the promise of directly monitoring the microvasculature. This technique has provided an early warning of shock progression during acute hemorrhage following trauma. 16 Moreover, the microvascular dysfunction of septic shock is related to organ failures, 6 while increased microcirculatory flow during resuscitation is associated with reduced subsequent organ dysfunction. 17 Static NIRS measures generally normalize, however, presumably due to shunting and cellular dysoxia, and so may be less useful during prolonged shock states.
How does shock affect lactic acid levels?
Shock often produces significantly elevated blood levels of lactic acid; sometimes this precedes hypotension and serves as an early indicator. 2 In a similar vein, successful resuscitation typically produces rapidly falling values. In a trial of early goal-directed therapy, targeting a lactate clearance of 10% was as good as aiming for normal central venous oxyhemoglobin saturation. 3 Moreover, normalization of lactate values is strongly associated with survival. 4 For patients with low CO shock (hypovolemic or cardiogenic), the genesis of hyperlactatemia is easy to understand: limited oxygen delivery to tissues cripples oxidative metabolism, causing tissues to shift to anaerobic production of ATP, and increases the generation and release of lactic acid. The lactic acidosis of sepsis (and perhaps some other forms of distributive shock) is more complex. In some patients, tissues may be deprived of oxygen, especially before resuscitation or perhaps in the mesenteric circulation, and produce lactic acid anaerobically. Yet many resuscitated septic patients have high CO, total body oxygen delivery, venous saturations, and tissue oxygen saturations, 5 along with oxidation-reduction ratios that do not support a theory of anaerobic metabolism. These findings cannot exclude oxygen lack, since microvascular dysfunction 6 and maldistribution of blood flow 7 may create hidden zones of hypoxia. Nevertheless, other mechanisms are likely, including enhanced aerobic glycolysis through activation of Na+/K ATPase, perhaps mediated by catecholamines. 8 This may be one reason that treatments for shock directed at augmenting oxygen delivery fail to lower lactic acid values or improve outcomes. 9, 10
Why is rapid recovery of intravascular volume important?
Rapid restoration of intravascular volume is an essential principle of shock resuscitation since fluids may promptly restore perfusion and prevent organ failures. Fluids should be infused at a rapid pace (usually much faster than typical ICU infusion pumps will allow), and in sufficient volume (which can be many liters). This practice allows for periodic reevaluation for clinical response: slower infusions of small volumes may confound the perception of response. Although colloid-containing fluids have some theoretical advantages over crystalloids, clinical trials generally show equivalence. Some colloids, especially synthetic starches, are clearly detrimental and should not be used. 25 Because crystalloids are more widely available, cheaper, and at least as effective, they are preferred for shock resuscitation. Although vasomotor function and vasopressors are both less active in acidemic environments, attempts to correct a metabolic acidosis with bicarbonate infusions do not speed resuscitation nor reduce vasopressor requirements, and may lead to worsening intracellular acidosis. Accordingly, bicarbonate infusions should be avoided.
How long after septic shock should antibiotics be given?
Appropriate antibiotics must be given within the first hour following the recognition of septic shock. Antibiotic therapy is frequently delayed and often ineffective for the final microbiologic diagnosis. Orders may be delayed due to diagnostic confusion and caregiver attention toward invasive procedures and hemodynamic resuscitation. Systems issues between ordering and administering antibiotics also contribute to these delays. Regardless of cause, delays in appropriate antibiotic administration worsen mortality by approximately 8% per hour of delay. 24 For these reasons, broad-spectrum antibiotics should be ordered and administered promptly after a diagnosis of shock when sepsis is in the differential, preferably guided by preplanned order sets. Antibiotics should then be tailored to microbial susceptibilities, as these data are available, or discontinued promptly if an alternative etiology of shock is identified.
When is mechanical adjunct used?
When ventricular dysfunction is so extensive that it is refractory to vasoactive infusions (or when valvular incompetence contributes to cardiogenic shock), mechanical adjuncts to aid circulation may be employed. Ideally, these devices are employed as a bridge to definitive correction of the cardiac dysfunction.
What are the four types of shock?
Synoptic view of the four types of shock (inner, white field) with the organ systems primarily associated with them (outer corners), sites and mechanisms of manifestation (outside the circle), and pathogenetic and pathophysiologic features (outer and middle sectors of the circle). To maintain clarity, mixed types of shock are not depicted.
What is the common feature of all types of shock?
A severe mismatch between the supply and demand of oxygen is the common feature of all types of shock. We present a newly developed, clinically oriented classification of the various types of shock and their therapeutic implications.
What is a traumatized hypovolemic shock?
Traumatic hypovolemic shock, resulting from a critical reduction in circulating plasma volume without acute hemorrhage, due to soft tissue injury and the release of immune system mediators.
What is hypovolemic shock?
Hypovolemic shock is a condition of inadequate organ perfusion caused by loss of intravascular volume, usually acute. The result is a drop in cardiac preload to a critical level and reduced macro- and microcirculation, with negative consequences for tissue metabolism and the triggering of an inflammatory reaction.
How many subcategories are there in hypovolemic shock?
Of these, hypovolemic shock is divided into four subcategories and distributive shock into three. Obstructive shock has been given a category of its own. Although this nomenclature and classification is schematic and there is some overlapping between the main groups, these four main groups can be basically assigned to four organ systems (figure 1) that, owing to differences in their pathogenesis and pathophysiology, require group-specific—or, in other words, organ-specific—treatment (figure 2):
How many types of shock are there?
There are only four major categories of shock, each of which is mainly related to one of four organ systems. Hypovolemic shock relates to the blood and fluids compartment while distributive shock relates to the vascular system; cardiogenic shock arises from primary cardiac dysfunction; and obstructive shock arises from a blockage of the circulation.
What are the characteristics of hemorrhagic shock?
The characteristic feature of both, hemorrhagic and traumatic hemorrhagic shock is bleeding . However, differences exist between the two subcategories in terms of the extent of soft tissue damage. Clinically the most significant cause of hemorrhagic shock is acute bleeding from an isolated injury to a large blood vessel, gastrointestinal bleeding , nontraumatic vascular rupture (e.g., aortic aneurysm), obstetric hemorrhage (e.g., uterine atony), and hemorrhage in the region of the ear, nose, and throat (vascular erosion). The shock is triggered by the critical drop in circulating blood volume; massive loss of red blood cells intensifies the tissue hypoxia.
