The principle of patient autonomy requires that physicians respect the decision to forgo life-sustaining treatment of a patient who possesses decision-making capacity. Life-sustaining treatment is any treatment that serves to prolong life without reversing the underlying medical condition.
When is it morally safer to forgo life-sustaining treatments?
In contrast to this common practice, the authors argue that in most instances, the morally safer route is actually to forgo life-sustaining treatments, particularly when their likelihood to effectuate a truly beneficial outcome has become small relative to the odds of harming the patient. The ethical analysis proceeds in three stages.
What are the two necessary conditions for life-sustaining interventions?
Next, the two necessary conditions for any medical treatment, i.e., that it is medically indicated and that consent is obtained, are applied to life-sustaining interventions. Finally, the difference between withholding and withdrawing a life-sustaining treatment is discussed.
Is forgoing life-sustaining medical treatment (LSMT) ethically supportable?
However, in some circumstances, the balance of benefits and burdens to the child leads to an assessment that forgoing life-sustaining medical treatment (LSMT) is ethically supportable or advisable. Parents are given wide latitude in decision-making concerning end-of-life care for their children in most situations.
What is the best approach to end-of-life care?
When a patient’s life seems to be nearing its end, it is generally felt that the morally best approach is to try a new intervention, continue all treatments, attempt an experimental course of action, in short, do something.
Do patients have the right to refuse life sustaining treatment?
Under federal law, the Patient Self-Determination Act (PSDA) guarantees the right to refuse life sustaining treatment at the end of life.
When is it justifiable to discontinue life sustaining treatment?
When is it justifiable to discontinue life-sustaining treatments? If the patient has the ability to make decisions, fully understands the consequences of their decision, and states they no longer want a treatment, it is justifiable to withdraw the treatment.
What is withholding or withdrawing life sustaining treatment?
Withholding and withdrawal of life support is a process through which various medical interventions are either not given to patients or removed from them with the expectation that the patients will die from their underlying illnesses.
What happen if life sustaining treatments are continued?
What happens if life-sustaining treatments are continued? These treatments can help extend your life. But they will not cure your illness. If you are near the end of your life, you may find it hard to handle the side effects and problems that can occur with these treatments.
What are the risks of life sustaining measures?
CPR can be life saving; however, there is a risk of broken or cracked ribs, punctured lungs and death. Mechanical ventilation supports a person's breathing when they can no longer breathe on their own. In this situation, a machine called a ventilator forces air into the lungs via tubing in the mouth or nose.
Who makes the decision to withdraw treatment?
Ideally, there should be consensus among the entire clinical team who have been heavily involved in the patients care, that it is appropriate to withhold or withdraw aggressive treatment. Usually two or more senior doctors, one of whom must be an ICU consultant, will agree on the decision.
Is withdrawal of treatment ethical?
The withdrawal of treatment is one of the most emotionally challenging and ethically complex aspects of end-of-life care. As our ability to prolong life progresses, the necessity to address issues such as the withdrawal of treatment increases in parallel.
What does life sustaining treatment mean?
Life-sustaining treatment is any treatment that serves to prolong life without reversing the underlying medical condition. Life-sustaining treatment may include, but is not limited to, mechanical ventilation, renal dialysis, chemotherapy, antibiotics, and artificial nutrition and hydration.
When can you withdraw from care?
In general, treatment is withdrawn when death is felt to be inevitable despite continued treatment. This would typically be when dysfunction in three or more organ systems persists or worsens despite active treatment or in cases such as multiple organ failure in patients with failed bone marrow transplantation.
Would you ever recommend or give life sustaining therapy when you judge it futile?
In surveying physicians, Medscape researchers asked, "Would you ever recommend or give life-sustaining therapy when you judged that it was futile?" Nearly 5300 physicians answered the question: 23.6% said yes, they would recommend or continue to give care they knew to be futile, while 37.0% said they would not.
Is there an ethically significant difference between withdrawing treatment so that a patient dies and withholding treatment so that a person dies?
Code of Medical Ethics Opinion 5.3 While there may be an emotional difference between not initiating an intervention at all and discontinuing it later in the course of care, there is no ethical difference between withholding and withdrawing treatment.
In what circumstances are medical treatments not indicated?
This last situation occurs when a patient is so seriously ill or injured that sound clinical judgment would suggest that the goals of restoration of health and function are unattainable and, thus, certain medical interventions that usually perform these functions are not indicated or should be limited.
Principles
As endorsed by professional organizations in North America and Europe, ethical decision-making concerning providing or forgoing LSMT for children is guided by the patient’s best interests.
Process Guidance
The ethical duties of veracity and fidelity call physicians to share “complete, honest and unbiased information with patients and their families on an ongoing basis and in ways they find useful and affirming.” 17 Beneficent actions also include efforts to identify individuals, groups, and other resources that can provide support to the patient and family.
Special Situations
Medically administered nutrition and hydration constitute interventions that may be withheld or withdrawn for the same types of reasons as other medical treatments.
Recommendations
When decisions to forgo LSMT are being contemplated, compassionate care for children who are severely ill and their families is enhanced by attention to the following considerations:
Competing Interests
POTENTIAL CONFLICT OF INTEREST: Dr Christian provides medical-legal expert work in child abuse cases; and Drs Weise, Okun, and Carter have indicated they have no potential conflicts of interest to disclose.
Liaisons
Mary Lynn Dell, MD, DMin – American Academy of Child and Adolescent Psychiatry
Liaisons
Harriet MacMillan, MD, MSc, FRCPC – American Academy of Child and Adolescent Psychiatry
Objectives
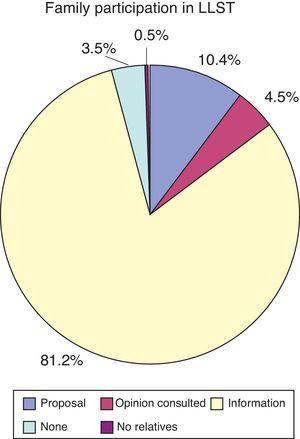
The decision to forgo life support is frequently made in pediatric intensive care units (PICUs). A group of experts is currently preparing recommendations for guidelines concerning this decision-making process in France. We have performed a prospective study to help the experts.
Patients
All consecutive deaths were recorded over a 4-month period. Children who died after a medical decision to forgo life-sustaining treatment were included in group 1 and children who died from other causes were included in group 1.
Main Results
A total of 264 consecutive children died, 40.1% from group 1 and 59.8% from group 2. Patients of both groups were primarily admitted for acute respiratory failure (group 1, 50.8%; group 2, 52.6%). Neurologic emergencies were more frequent in patients in group 1, whereas patients with cardiovascular failures were more frequent in group 2.
Conclusions
The decision to forgo life-sustaining treatment is frequently made for children dying in French PICUs. Guidelines must be available to help the medical staff reach this decision. Knowledge of the decision-making process in French PICUs provides the experts with information needed to elaborate such recommendations.
What is life sustaining treatment?
Life-sustaining treatment is any treatment that serves to prolong life without reversing the underlying medical condition. Life-sustaining treatment may include, but is not limited to, mechanical ventilation, renal dialysis, chemotherapy, antibiotics, and artificial nutrition and hydration. There is no ethical distinction between withdrawing ...
What is the discouraging evidence of inadequate end-of-life decision making?
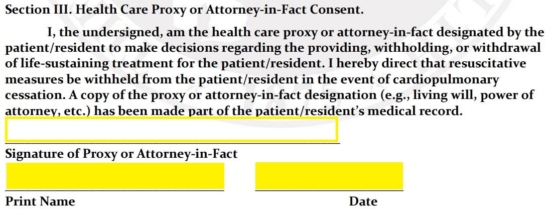
The discouraging evidence of inadequate end-of-life decision making indicates the necessity of several improvement strategies: (1) Patients and physicians should make use of advisory as well as statutory documents. Advisory documents aim to accurately represent a patient’s wishes and are legally binding under law.
What should a physician provide to a surrogate decision maker?
Physicians should provide all relevant medical information and explain to surrogate decision makers that decisions regarding withholding or withdrawing life-sustaining treatment should be based on substituted judgment (what the patient would have decided) when there is evidence of the patient’s preferences and values.
What is the social commitment of a physician?
The social commitment of the physician is to sustain life and relieve suffering. Where the performance of one duty conflicts with the other, the preferences of the patient should prevail. The principle of patient autonomy requires that physicians respect the decision to forgo life-sustaining treatment of a patient who possesses decision-making ...
Is it unethical to discontinue all means of life-sustaining medical treatment?
Even if the patient is not terminally ill or permanently unconscious, it is not unethical to discontinue all means of life-sustaining medical treatment in accordance with a proper substituted judgment or best interests analysis.
Is there an ethical distinction between withdrawing and withholding life-sustaining treatment?
There is no ethical distinction between withdrawing and withholding life-sustaining treatment. A competent, adult patient may, in advance, formulate and provide a valid consent to the withholding or withdrawal of life-support systems in the event that injury or illness renders that individual incompetent to make such a decision.
