
Medication
Top Natural Home Remedies for Bed Sores – 15 Useful Treatments
- Honey. Honey is one of the most effective home remedies for bed sores treatment. ...
- Aloe Vera. Aloe Vera contains soothing and healing properties, so it can promote healing and reduce risk of infection.
- Turmeric. ...
- Coconut Oil. ...
- Saline Water. ...
- Papaya Milk. ...
- Comfrey Leaves. ...
- Goldenseal. ...
- Vitamin C. ...
- Zinc. ...
Procedures
💕【Moderate Bedsores】 1.76oz (50g) LMNOOP Bedsore Cream is suitable for moderate bedsore. This type of bedsore is generally less than 2in (5cm) in diameter and 0.4in (1cm) in depth, with obvious tissue defects in the skin.
Self-care
- Eat healthy foods. Getting the right nutrition will help you heal.
- Lose excess weight.
- Get plenty of sleep.
- Ask your provider if it's OK to do gentle stretches or light exercises. This can help improve circulation.
Nutrition
Medications used to treat bed sores are prescribed for two primary reasons: to clear a bacterial infection, and to reduce pain. Your doctor may recommend applying topical antibacterial preparations directly to the sores one or more times a day. Oral or intravenous antibiotics may be prescribed to clear a more severe or resistant infection.
What is the best natural remedy for bed sores?
What is the best cream for treating bedsores?
What will heal bedsores?
How do medications treat bed sores?
See more
How do you treat bed sores?
How are bedsores treated?Removing pressure on the affected area.Protecting the wound with medicated gauze or other special dressings.Keeping the wound clean.Ensuring good nutrition.Removing the damaged, infected, or dead tissue (debridement)Transplanting healthy skin to the wound area (skin grafts)More items...
What is the cause of bed sores?
Bedsores are caused by pressure against the skin that limits blood flow to the skin. Limited movement can make skin vulnerable to damage and lead to development of bedsores.
What bed sores look like?
Symptoms: The sore looks like a crater and may have a bad odor. It may show signs of infection: red edges, pus, odor, heat, and/or drainage. The tissue in or around the sore is black if it has died.
How do you heal bed sores fast?
TreatmentsRelieve the pressure: This might involve using foam pads or pillows to prop up affected areas, changing the body's position.Clean the wound: Gently wash very minor sores with water and mild soap. ... Apply dressings: These protect the wound and accelerate healing.More items...
Can bedsores cause death?
Factors such as proper medical care and preventing complications can help patients live longer. That said, roughly 60,000 people die each year due to bedsore-related complications. Over 50% of those who develop bedsores in hospital settings die in a year or less, according to a 2020 study.
How serious is a bedsore?
A stage 4 bedsore is a large wound in which the skin is significantly damaged. Muscle, bone, and tendons may be visible through a hole in the skin, putting the patient at risk of serious infection or even death. A stage 4 bedsore can be a sign of nursing home abuse since it is usually preventable with proper care.
What do Stage 1 bed sores look like?
A Stage 1 bed sore is a red patch of skin typically appearing over a bony area like the heel or tailbone that does not blanch. Blanching means the paleness or whiteness that results when pressure is applied to the skin. Skin that does not turn white is called “non-blanchable.”
Is Vaseline good for bed sores?
Clean open sores on the skin with salt water (saline, which can be made by boiling 1 quart of water with 1 teaspoon of salt for 5 minutes and kept cooled in a sterile container). Apply a thin layer of petroleum jelly (Vaseline®) and then cover with a soft gauze dressing.
How do you heal bed sores naturally?
Apply aloe vera to cure bed sores, prevent them from returning, and also prevent itching and burning sensations. Apply saline water as a disinfectant to keep the area clean. Mix beetroot with honey to moisturize the area and prevent itchiness and redness. Apply turmeric to reduce pain and provide relief instantly.
Are bedsores painful?
Bedsores can be extremely painful. It is essentially an open wound, and usually develops in areas of the body that are hard to avoid putting pressure on. Even the most mundane of activities can cause serious pain when a patient has a bedsore. A bedsore is also known as a pressure sore or ulcer, or a decubitus ulcer.
What antibiotics treat bed sores?
Silver sulfadiazine and nitrofurazone are topical (locally acting) antibiotics while the other treatments are antiseptics.
How long do bed sores take to heal?
Pressure ulcers, also known as bedsores or decubitus ulcers, can take anywhere from three days to two years to heal. How quickly a pressure ulcer heals depends on how far advanced the sore is and what steps are taken to treat it.
How to help a bed sore?
Providing soft padding in wheelchairs and beds to reduce pressure. Providing good skin care by keeping the skin clean and dry. Providing good nutrition because without enough calories, vitamins, minerals, fluids, and protein, bed sores can’t heal, no matter how well you care for the sore.
How to prevent bed sores from getting worse?
Other methods of preventing bedsores and preventing existing sores from getting worse include: Turning and repositioning every 2 hours.
Why do people get bedsores?
If an immobile or bedridden person is not turned, positioned correctly, and given good nutrition and skin care, bedsores can develop. People with diabetes, circulation problems, and poor nutrition are at higher risk.
What is a bedsore?
Bedsores are ulcers that happen on areas of the skin that are under pressure from lying in bed, sitting in a wheelchair, and/or wearing a cast for a prolonged period. Bedsores can happen when a person is bedridden, unconscious, unable to sense pain, or immobile. Bedsores can be prevented by inspecting the skin for areas of redness ...
What is it called when you are bedridden?
Bedsores can happen when a person is bedridden or otherwise immobile, unconscious, or unable to sense pain. Bedsores are ulcers that happen on areas of the skin that are under pressure from lying in bed, sitting in a wheelchair, or wearing a cast for a prolonged time. Bedsores are also called pressure injuries, pressure sores, pressure ulcers, ...
What causes a bedsore to turn purple?
What causes bedsores? A bedsore develops when blood supply to the skin is cut off for more than 2 to 3 hours. As the skin dies, the bedsore first starts as a red, painful area, which eventually turns purple. Left untreated, the skin can break open and the area can become infected. A bedsore can become deep.
How long does it take for a bedsore to heal?
Once a bedsore develops, it can take days, months, or even years to heal. It can also become infected, causing fever and chills. An infected bedsore can take a long time to clear up. As the infection spreads through your body, it can also cause mental confusion, a fast heartbeat, and generalized weakness.
What is a bedsore?
Close. Bedsore. Bedsore. Bedsores are areas of damaged skin and tissue caused by sustained pressure — often from a bed or wheelchair — that reduces blood circulation to vulnerable areas of the body. Bedsores — also called pressure ulcers and decubitus ulcers — are injuries to skin and underlying tissue resulting from prolonged pressure on the skin.
How to treat pressure sores on skin?
Protect the skin. Use moisture barrier creams to protect the skin from urine and stool. Change bedding and clothing frequently if needed. Watch for buttons on the clothing and wrinkles in the bedding that irritate the skin. Inspect the skin daily. Look closely at your skin daily for warning signs of a pressure sore.
How to tell if you have a bedsore?
Warning signs of bedsores or pressure ulcers are: Unusual changes in skin color or texture. Swelling. Pus-like draining. An area of skin that feels cooler or warmer to the touch than other areas. Tender areas. Bedsores fall into one of several stages based on their depth, severity and other characteristics.
What are the complications of pressure ulcers?
Complications of pressure ulcers, some life-threatening, include: Cellulitis. Cellulitis is an infection of the skin and connected soft tissues. It can cause warmth, redness and swelling of the affected area. People with nerve damage often do not feel pain in the area affected by cellulitis. Bone and joint infections.
Where do bedsores occur?
For people who use wheelchairs, bedsores often occur on skin over the following sites: Tailbone or buttocks. Shoulder blades and spine. Backs of arms and legs where they rest against the chair. For people who need to stay in bed, bedsores may happen on: The back or sides of the head. The shoulder blades.
Can a skin ulcer cause sepsis?
Cancer. Long-term, nonhealing wounds (Marjolin's ulcers) can develop into a type of squamous cell carcinoma. Sepsis. Rarely, a skin ulcer leads to sepsis.
What are the risk factors for sores?
The following can increase the chances that sores develop: being unable to move unaided. older age, as the skin becomes thinner and more fragile. incontinence, which increases the risk of skin damage and infection. a low or high body mass index, or BMI, either of which can increase pressure.
Why do sores form?
They often form in people who need help changing positions. These sores form when tissues and blood vessels become compressed, then distorted. This can lead to poor circulation, resulting in tissue death and infection. Sores can result from significant pressure over a short period or low pressure over a longer period.
How to clean a wound with a saline solution?
Clean the wound: Gently wash very minor sores with water and mild soap. Clean open sores with a saline solution with each change of dressing. Apply dressings: These protect the wound and accelerate healing. Options that are antimicrobial or hydrocolloid, or that contain alginic acid, may be best.
What is the best way to treat a bacterial infection?
Dressings are available for purchase online. Use topical creams: Antibacterial creams can help combat an infection, while barrier creams can protect damaged or vulnerable skin.
How to tell if you have a pressure sore?
If discoloration does not disappear after removing the pressure for 10–30 minutes, this may indicate that a sore is forming.
What is the best way to relieve pressure on a mattress?
A healthcare provider may use a high-pressure water jet or surgical instruments. Review the bedding: Some mattresses, such as dynamic varieties or those made of static foam, help relieve pressure. Also, some beds have a pump that ensures a constant flow of air into the mattress.
Where do pressure ulcers form?
Also known as pressure ulcers, these sores form due to lasting pressure on specific areas of the body. They can develop anywhere, but the bony parts of the elbows, knees, heels, tailbone, and ankles are often more susceptible.
How to get rid of bed sores?
Massage is an effective home remedy for bed sores by speeding up blood circulation and promote the healing process in getting rid of bed sores. You should massage the body with essential oils and repeat once daily to have the positive result.
What is the best home remedy for bed sores?
1. Honey. Honey is one of the most effective home remedies for bed sores treatment. It is a natural antiseptic agent;
How to get rid of bed sores with papaya milk?
How to use: Soak a bandage in papaya “milk” from either the trunk or green fruit. Apply it on the sores at least 3 times daily.
How to heal bed sores naturally?
Another effective method on how to heal bed sores is turmeric because it has anti-inflammatory, antiseptic and antioxidant properties, which can promote healing process and reduce risk of infection [ 7][ 8]. This is the reason why turmeic is considered as among safe and natural home remedies for bed sore.
How to use zinc for bed sores?
How to use: Take about 15 milligrams of zinc three times a day. You should consume it with food to avoid stomach upset. 11. Witch Hazel. Another method from those home remedies for bed sores and support treating process is witch hazel, which acts as an astringent and myrrh, which acts as a resin.
How to use goldenseal for bed sores?
It become one of the most workable bed sore home treatments. How to use: Steep 1 teaspoon of goldenseal powder in a cup of boiling water for some minutes.
How to get rid of a sore on my bed?
Mix equal amounts of both sugar and honey well to form a thick mixture. Apply directly the mixture on bed sores and cover them with a clean piece of bandage. Use this remedy once a day until you can get rid of bed sores. In addition to bed sores, honey is also great home remedy for many other health problems.
What is bed sore?
Bed sores (also known as pressure ulcers or decubitus ulcers) are injuries to the skin and underlying tissues that are results of prolonged pressure on the skin, which leads to inadequate blood flow to the area.
How much does it cost to treat a bed sore?
The cost to treat them is $9.1 billion to $11.6 billion per year in the US. Individual patient care ranges from $20,900 to $151,700 per bed sore. Each bed sore adds $43,180 in costs to a hospital stay. 60,000 patients die as a direct result of a bed sore each year. Even though we cannot prevent all bed sores, it’s still much easier ...
Why do older adults get bed sores?
Bed sores in older adults form more often than in other age groups because, in addition to frailty and thin skin, they tend to have more risk factors, which include the following: Immobility: Poor health, spinal cord injury, and other causes can lead to immobility.
How are bed sores classified?
Bed sores are classified into several stages according to their depth, their severity, and other factors. We will describe the signs and symptoms of each stage individually.
What is pressure ulcer?
Pressure ulcers, commonly referred to as bed sores, are one of the most feared complications that can happen to bedridden patients. Because of certain risk factors associated with old age, bed sores in elderly people are particularly prevalent. If we take a look at the data collected by the Agency for Healthcare Research and Quality (AHRQ), ...
How long does it take for a pressure ulcer to heal?
About 70%–90% of pressure ulcers are stage 1 or stage 2. They can heal within one to six weeks. Stage 3 and 4 pressure ulcers can take months to heal, which is another reason for aggressive prevention and treatment that will halt progression into later stages.
What is the first sign of a pressure sore?
What is the first sign of a pressure sore? It’s redness of the skin that’s still intact but doesn’t turn white when pressed. Changes in sensation, temperature, or firmness can also be present. Purple or maroon discoloration does not belong in this stage because it may indicate deep tissue injury.
What is the most common cause of death for patients suffering from chronic bedsores?
According to an article in the Western Journal of Medicine, renal failure and amyloidosis are the most common causes of death for patients suffering from chronic bedsores. It may be considered a wrongful death if a nursing home patient dies from an untreated bedsore.
How do doctors determine the stage of a bedsore?
A doctor determines the stage of a bedsore by its appearance. In the case of a stage 4 bedsore, the large wound has passed the body’s fatty tissue layer, exposing muscles, ligaments, or even bone.
What does a stage 4 bedsore mean?
They often cause residents to suffer extreme pain, infection, invasive surgeries, or even death. A stage 4 bedsore may be an unfortunate sign of nursing home neglect. Residents of nursing homes may develop these sores if the staff fails to treat earlier-stage sores.
What stage of sepsis is a bedsore?
Sepsis develops when the body tries too hard to fight infection. A stage 4 bedsore can trigger the infections that lead to sepsis. In 2014, an elderly nursing home resident from Chicago died after developing a serious bedsore that led to sepsis.
What causes a stage 4 bedsore?
All bedsores are caused when factors like pressure, shear, and friction cut off blood supply to the skin. Without proper treatment, the loss of blood can cause the skin to die and a wound to form. Did You Know.
How long can you live with a stage 4 bedsore?
Patients can live for months or even years after developing a stage 4 bedsore. Factors such as proper medical care and preventing complications can help patients live longer. That said, roughly 60,000 people die each year due to bedsore-related complications.
Can a late stage bed sprain be prevented?
Yes. Like many nursing home injuries, late-stage bedsores are largely preventable with proper care. They can be prevented by treating stage 3 bedsores or lower-stage bedsores from forming in the first place.

Overview
Symptoms
Causes
Risk Factors
Specialist to consult
Complications
- Your doctor will likely look closely at your skin to decide if you have a pressure ulcer and, if so, to assign a stage to the wound. Staging helps determine what treatment is best for you. You might need blood tests to assess your general health.
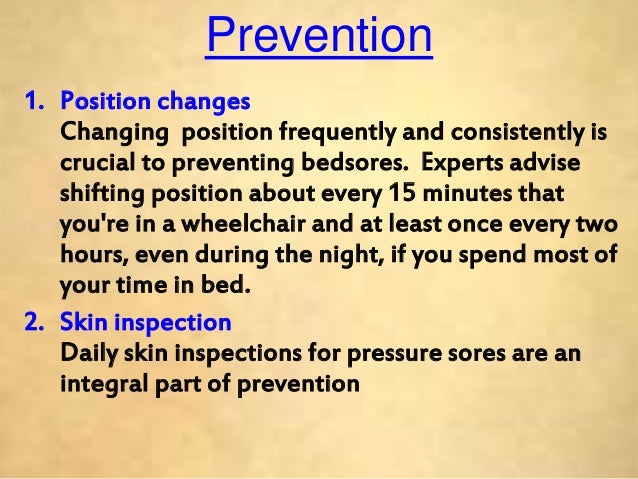
Prevention