What OTC treatments are the best for diverticulitis?
Dec 05, 2016 · New guidelines for the management of acute diverticulitis suggest that antibiotics be used selectively, rather than routinely, in patients with uncomplicated acute diverticulitis. 1 The guidelines are accompanied by a detailed technical review. 2. The recommendation itself is based on two large multicenter trials.
Which home remedies can help treat diverticulitis?
Apr 22, 2022 · Best Antibiotic for Diverticulitis. Amoxicillin-clavulanate (AC) compared to fluoroquinolone + metronidazole (FM) was not associated with worsened outcomes for outpatient treatment of diverticulitis and may reduce known harm related to …
What pain drugs are safe with diverticulitis?
Apr 19, 2022 · Antibiotics to treat infection, although new guidelines state that in very mild cases, they may not be needed. A liquid diet for a few days while your bowel heals. Once your symptoms improve, you can gradually add solid food to your diet. This treatment is successful in most people with uncomplicated diverticulitis.
What antibiotics are best for diverticulosis?
Apr 21, 2022 · When inflammation and infection of the intestinal diverticula occur, there are several antibiotics for diverticulitis a doctor may prescribe to a patient. For relatively mild cases, oral antibiotics are usually sufficient; some common ones are ciprofloxacin, metronidazole, and doxycycline. Levofloxacin, moxifloxacin, or cephalexin may also be used.
Do I need antibiotics for diverticulitis?
If your symptoms are mild, you may be treated at home. Your doctor is likely to recommend: Antibiotics to treat infection, although new guidelines state that in very mild cases, they may not be needed. A liquid diet for a few days while your bowel heals.
What is the standard treatment for diverticulitis?
How long do you have to take antibiotics for diverticulitis?
What triggers diverticulitis flare ups?
- Over age 40.
- Overweight or obese.
- A smoker.
- Physically inactive.
- Someone whose diet is high in animal products and low in fiber (most Americans)
- Someone who takes non-steroidal anti-inflammatory drugs (NSAIDs), steroids or opioids.
How do I know if my diverticulitis burst?
Will amoxicillin treat diverticulitis?
How do you calm inflamed diverticulitis?
What happens if diverticulitis does not respond to antibiotics?
What is the best antibiotic for diverticulitis?
Best Antibiotic for Diverticulitis. Amoxicillin-clavulanate (AC) compared to fluoroquinolone + metronidazole (FM) was not associated with worsened outcomes for outpatient treatment of diverticulitis and may reduce known harm related to the fluoroquinolone class of antibiotic.
Can antibiotics be used for diverticulitis?
There is some evidence that in select cases, antibiotics could be avoided for diverticulitis, though I remain skeptical. Usually, FM is prescribed for outpatient treatment of diverticulitis. Yet fluoroquinolones are associated with tendon rupture, hypoglycemia, altered mental status, possibly aortic dissection, QT prolongation, ...
What is the best treatment for diverticulitis?
Surgery. You'll likely need surgery to treat diverticulitis if: You have a complication, such as a bowel abscess, fistula or obstruction, or a puncture (perforation) in the bowel wall. You have had multiple episodes of uncomplicated diverticulitis. There are two main types of surgery:
How to treat diverticulitis?
Treatment generally involves: Intravenous antibiotics. Insertion of a tube to drain an abdominal abscess, if one has formed.
How long after diverticulitis can you have a colonoscopy?
Your doctor may recommend colonoscopy six weeks after you recover from diverticulitis, especially if you haven't had the test in the previous year. There doesn't appear to be a direct link between diverticular disease and colon or rectal cancer.
What is the best way to remove a weakened immune system?
You have a weakened immune system. There are two main types of surgery: Primary bowel resection. The surgeon removes diseased segments of your intestine and then reconnects the healthy segments (anastomosis). This allows you to have normal bowel movements.
What tests are done to rule out pelvic disease?
Women generally have a pelvic examination as well to rule out pelvic disease. After that, the following tests are likely: Blood and urine tests, to check for signs of infection. A pregnancy test for women of childbearing age, to rule out pregnancy as a cause of abdominal pain. A liver enzyme test, to rule out liver-related causes of abdominal pain.
Can diverticulitis be diagnosed during an acute attack?
Diverticulitis is usually diagnosed during an acute attack. Because abdominal pain can indicate a number of problems, your doctor will need to rule out other causes for your symptoms.
Does Mayo Clinic help with diverticulitis?
Our caring team of Mayo Clinic experts can help you with your diverticulitis- related health concerns Start Here
What antibiotics are used for diverticulitis?
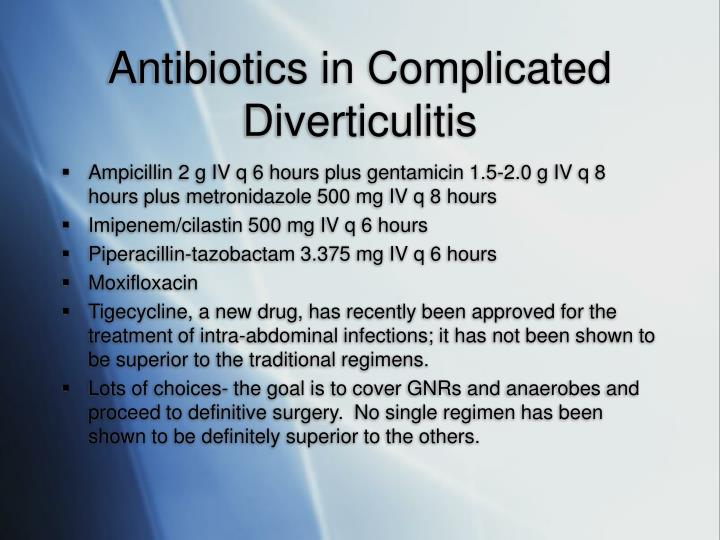
When inflammation and infection of the intestinal diverticula occur, there are several antibiotics for diverticulitis a doctor may prescribe to a patient. For relatively mild cases, oral antibiotics are usually sufficient ; some common ones are ciprofloxacin, metronidazole, and doxycycline. Levofloxacin, moxifloxacin, or cephalexin may also be used. Patients who have more severe cases of diverticulitis may need to be admitted to a hospital where antibiotics can be administered intravenously while their digestive systems are allowed to rest and recover.
What is the best treatment for diverticulitis?
Antibiotic treatment for diverticulitis depletes the body of good bacteria that helps with digestion and may require a probiotic supplement to replenish a healthy supply.
When is intravenous antibiotics needed?
When a patient is suffering from a severe infection from diverticulitis, intravenous antibiotics may be necessary. Patients will need to stay in a hospital so doctors can administer the drugs and monitor how effectively they are fighting the infection. A variety of different antibiotics may be used; some possibilities can include aztreonam, cefoxitin, or ertapenem.
Can antibiotics cause headaches?
Headaches are a common side effect of antibiotics that are typically prescribed for diverticulitis.
Is intravenous antibiotics necessary for severe infection?
Intravenous antibiotics and hospital monitoring may be necessary for a severe infection.
What are the symptoms of diverticulitis?
But it’s still important to look out for warning signs, including severe abdominal pain, fever, a hard and tense tummy, and nausea. Symptoms like this should be checked out by a doctor as soon as possible.
How long does it take for diverticulitis to go away?
In about 95 out of 100 people, uncomplicated diverticulitis goes away on its own within a week. In about 5 out of 100 people, the symptoms stay and treatment is needed. Surgery is only rarely necessary.
How long does diverticulitis take to clear up?
In about 80 out of 100 people, complicated diverticulitis clears up within a few weeks of having treatment with antibiotics. About 20 out of 100 people have surgery.
Can diverticulitis be blocked?
Sometimes the inflammation has even already spread or the wall of the intestine has torn (intestinal perforation). The intestine may also become blocked or the inner lining of the tummy may become inflamed (peritonitis).
Can you have diverticulitis surgery on the bowel?
Even if a long-lasting infection with pus goes away after treatment with antibiotics, doctors still often recommend operating on the bowel. The aim of this surgery is to prevent people from developing diverticulitis again. Research has shown that almost half of all people who have previously had successful treatment with antibiotics go on to develop diverticulitis again within a few years – and new episodes sometimes lead to serious complications. People who have a weakened immune system or chronic kidney disease are also at higher risk of serious complications.
Can diverticulitis come back?
Acute diverticulitis that has been successfully treated may come back again after some time. The risk of this happening is greater after having the complicated form.
When to see a doctor for diverticulitis?
In uncomplicated diverticulitis, it’s important to see a doctor regularly – particularly in the first few days – in order to detect any complications early enough. The doctor can do blood tests to monitor the level of inflammation in your body, for example. The treatment is often possible on an outpatient basis (without a hospital stay).
Diverticular Disease of the Colon
1. Choose citation style Select style Vancouver APA Harvard IEEE MLA Chicago
Abstract
Diverticulosis is a common disease among Western and developed nations. Approximately 20% of patients with diverticulosis will become symptomatic. Acute diverticulitis is a common manifestation of diverticular disease. Different classifications exist to try to categorize it but, it is generally considered as complicated or uncomplicated.
1. Introduction
Diverticulosis is a common disease among the Western and developed nations; its prevalence increases with age, being 10% in adults over 40 years and around 70% in patients over 80 years. Approximately 20% of patients with diverticulosis will become symptomatic [ 1 ].
2. Discussion
Diverticulitis treatment has been modified throughout time. The prescription of antibiotics used to be the therapeutic foundation of it, but it could be avoided now in well-selected patients [ 10 ]. The nonantibiotic treatment strategy was formulated more than a decade ago when diverticular physiopathology was reassessed.
3. Conclusions
The nonantibiotic management in patients with uncomplicated diverticulitis still has some unsettled topics like management of the right-sided or recurrent uncomplicated disease; further investigation in different populations and world regions is needed.
What antibiotics should be used for diverticulitis?
Broad-spectrum antibiotic s covering gram-negative rods and anaerobic bacteria should be used in patients with complicated diverticulitis.
What is the best treatment for diverticulitis?
Outpatient management with rest and fluids is effective for patients with mild diverticulitis. Inpatient management is recommended in patients with moderate to severe diverticulitis. Broad-spectrum antibiotics covering gram-negative rods and anaerobic bacteria should be used in patients with complicated diverticulitis.
What are the factors that contribute to diverticulosis?
Factors associated with diverticulosis include alterations in colonic wall resistance, colonic motility, and dietary issues, such as lack of fiber, that contribute to increased intraluminal pressure and weakness of the bowel wall. 1 Genetic susceptibility is an important component for the development of diverticular disease because monozygotic twins are twice as likely as dizygotic twins to develop diverticulosis. 7 Aspirin and nonsteroidal anti-inflammatory drugs increase the risk of diverticulitis (hazard ratio = 1.2 to 1.7). 8 Other risk factors for diverticulitis include increasing age, obesity, and lack of exercise. 1
How to prevent diverticulitis recurrence?
Interventions to prevent recurrences of diverticulitis include increased intake of dietary fiber, exercise, and, in persons with a body mass index of 30 kg per m 2 or higher, weight loss. 36 – 38 Counseling for smoking cessation is recommended because smoking is associated with an increased incidence of complicated diverticulitis and less favorable outcomes (e.g., surgery at a younger age, higher risk of recurrence). 39 Evidence from a prospective cohort study of 47,228 men in the United States found no evidence that avoiding nuts, corn, or popcorn decreases the risk of diverticulosis or diverticular complications, such as diverticulitis. 40 A small prospective study found that mesalamine and Lactobacillus casei are effective in preventing recurrence. 41 A meta-analysis of four randomized controlled trials with 1,660 patients who had experienced at least one episode of diverticulitis found that rifaximin (Xifaxan) plus fiber provided one year of complete symptom relief (number needed to treat = 3) and fewer complications (number needed to treat = 59) compared with fiber alone. 42
How often does diverticulitis recur?
A retrospective study analyzing 954 consecutive patients with diverticulitis found the five-year recurrence rate was 36 percent, with 3.9 percent of patients having a complicated recurrence including abscesses, fistula, or free perforation. 34 Age 50 years or older was associated with lower risk of recurrent diverticulitis (12.2 percent) compared with age younger than 50 years (16.2 percent), with a hazard ratio of 0.68 (95% confidence interval, 0.53 to 0.87). 26 A modeling analysis found that the most cost-effective approach was to perform surgery only after the third episode of acute uncomplicated diverticulitis requiring hospitalization, but the decision to proceed to surgery should be individualized and based on patient preference, comorbidities, and lifestyle. 35
What is the most common type of diverticulitis?
Acute diverticulitis is inflammation of the colonic diverticulum, which may involve perforation or microperforation ( Figures 1 and 2). In Western societies, most diverticula (85 percent) are found in the sigmoid and descending colons; diverticula in the ascending colon are more common in Asian populations. 1 Uncomplicated diverticulitis is localized inflammation, and complicated diverticulitis is inflammation associated with an abscess, phlegmon, fistula, obstruction, bleeding, or perforation. 2 This article reviews acute diverticulitis in adults and excludes special populations, such as children and pregnant women.
How to treat diverticulitis in hospital?
The decision to hospitalize a patient with uncomplicated diverticulitis depends on several factors, including the patient's ability to tolerate oral intake, severity of illness, comorbidities, and outpatient support systems. 2 Hospitalization should be considered if patients have signs of peritonitis or there is suspicion of complicated diverticulitis. Inpatient management includes no food or drink by mouth, intravenous fluid resuscitation (normal saline or lactated Ringer solution), and intravenous antibiotics. 2 Clinical improvement is expected within two to four days and includes decreasing fever, leukocytosis, and pain. 2 A randomized controlled trial including 50 patients found that starting oral antibiotics after clinical improvement with intravenous antibiotics resulted in shorter hospitalizations, greater cost savings, and no increased risk of recurrence compared with longer treatment with intravenous antibiotics. 21
What are the drugs used for diverticulitis?
Select drug class All drug classes amebicides (4) miscellaneous antibiotics (4) quinolones (4) sulfonamides (7) lincomycin derivatives (5) Rx. OTC.
What is the name of the inflammation of the large intestine?
Diverticulitis is inflammation of an abnormal pouch (diverticulum) in the intestinal wall, usually found in the large intestine (colon). The presence of the pouches themselves is called diverticulosis.