What is the best treatment for gonorrhea?
Ceftriaxone, a third-generation cephalosporin, is recommended for gonorrhea treatment. For extragenital site infections, especially pharyngeal, failure rates of nonceftriaxone regimens can be substantial. In most clinical settings, patients who report a penicillin allergy are not treated with ß-lactam antimicrobials.
How do you get rid of gonorrhea?
If someone has a penicillin allergy, there is potential to have an adverse reaction to the antibiotic treatment for gonorrhea. Depending on personal health history, a physician will be able to prescribe an effective alternative for treating anyone with a penicillin allergy or who has a history of gonorrhea infection(s).
How to cure gonorrhea without going to the Doctor?
Apr 19, 1975 · Results following treatment of acute gonorrhea with aqueous penicillin combined with probenecid and spectinomycin hydrochloride (2.0 g) are compared and found to be statistically equivalent. Therefore, if a patient is allergic to penicillin, spectinomycin hydrochloride can be regarded as a valuable alternative.
What antibiotics are used to treat gonorrhea?
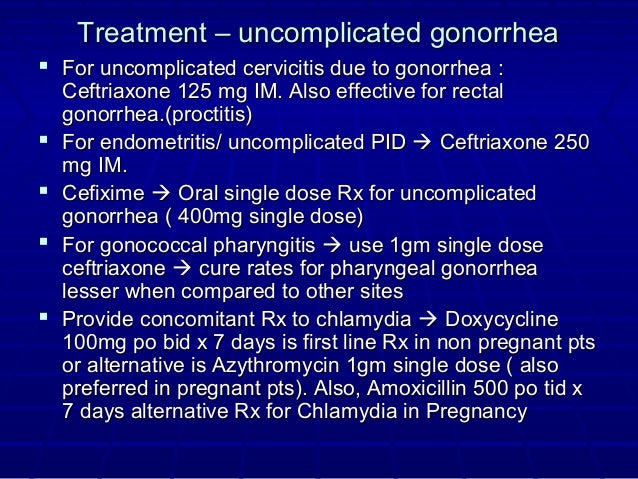
Alternative regimens for uncomplicated gonococcal infections of the cervix, urethra, or rectum if ceftriaxone is not available: • Gentamicin 240 mg IM as a single dose plus azithromycin 2 g orally as a single dose, OR
What is an alternative for penicillin allergy?
Options for penicillin-allergic patients include clindamycin or clarithromycin for 10 days or azithromycin for 5 days. For patients with recurrent or complicated group A streptococcal infections, cephalosporins may be appropriate.Sep 11, 2020
How do you treat gonorrhea if you are allergic to cephalosporins?
Azithromycin 2 g orally in a single dose may be used to treat cervical, urethral, rectal, or pharyngeal gonorrhea in patients with cephalosporin allergy or severe penicillin allergy. Routine use of azithromycin alone should be avoided due to evidence of emerging resistance.
What is the drug of choice and alternative for gonorrhea?
Gonorrhea can be cured with the right treatment. CDC recommends a single dose of 500 mg of intramuscular ceftriaxone. Alternative regimens are available when ceftriaxone cannot be used to treat urogenital or rectal gonorrhea.
What antibiotics can you use if you are allergic to penicillin to fight STDS?
Penicillin allergy warrants an exchange with Azithromycin, Doxycycline, Tetracycline or ceftriaxone.
Can you have ceftriaxone if allergic to penicillin?
Cephalothin, cephalexin, cefadroxil, and cefazolin confer an increased risk of allergic reaction among patients with penicillin allergy. Cefprozil, cefuroxime, cefpodoxime, ceftazidime, and ceftriaxone do not increase risk of an allergic reaction.
Can I take cephalexin if I'm allergic to penicillin?
It is acceptable to use cephalexin in individuals with confirmed or unconfirmed amoxicillin or penicillin allergy. I would use amoxicillin in an individual with an unconfirmed cephalexin allergy if it was the drug of choice.Feb 11, 2020
What is the best drug for treating gonorrhea?
Adults with gonorrhea are treated with antibiotics. Due to emerging strains of drug-resistant Neisseria gonorrhoeae, the Centers for Disease Control and Prevention recommends that uncomplicated gonorrhea be treated with the antibiotic ceftriaxone — given as an injection — with oral azithromycin (Zithromax).Oct 5, 2021
Can cotrimoxazole treat gonorrhea?
The incidence of post-gonococcal non-specific urethritis was 6 per cent. At present cotrimoxazole seems to be the most useful alternative to penicillin in the treatment of gonorrhoea.
Can you treat gonorrhea without injection?
It's sometimes possible to have an antibiotic tablet instead of an injection, if you prefer. If you have any symptoms of gonorrhoea, these will usually improve within a few days, although it may take up to 2 weeks for any pain in your pelvis or testicles to disappear completely.
Can ciprofloxacin cure gonorrhea?
Even though WHO and the US Centers for Disease Control recommend a single-dose of 500 mg ciprofloxacin to treat uncomplicated gonorrhea, the findings of the international studies suggest that a single dose of 250 mg ciprofloxacin effectively treats uncomplicated gonorrhea, even extragenital sites of infection.
Can doxycycline cure gonorrhea and chlamydia?
Doxycycline is successful in treating many types of infections, including: Other sexually transmitted infections (STIs): In addition to treating gonorrhea, doxycycline may be prescribed to treat syphilis, chlamydia, or pelvic inflammatory disease.Mar 4, 2022
Can ciprofloxacin cure gonorrhea and chlamydia?
It is concluded that a single oral dose of ciprofloxacin is an effective treatment for uncomplicated gonorrhoea, but is ineffective against C trachomatis.
How to treat gonorrhea?
In order to treat a gonorrhea infection, it must first be medically diagnosed through an STD test. To find out more about the gonorrhea test offered by STDAware, click here. STD testing should be requested anytime there is a change in sexual partner or habits before initiating sexual contact.
How long does it take for gonorrhea to go away?
Once treatment is started, symptoms should start to abate within 2 – 10 days. When treating gonorrhea or any other STD, it is critical to abstain from any sexual activity (oral, manual, vaginal or anal) until treatment is complete and the doctor confirms it is okay to resume sexual activity.
How much does a gonorrhea test cost?
Because treatment cannot be administered without a medical diagnosis, you must first be tested for gonorrhea. A typical doctor’s visit and test without insurance can range anywhere from $100 to $1,000 and will not include the cost of treatment which can range from $100 - $500. STDAware offers a gonorrhea test for less than $100.
Can antibiotics cure gonorrhea?
Although antibiotics will, generally, stop and cure a gonorrhea infection, they will not undo any damage the virus may have caused to the body before it was treated . A gonorrhea infection can cause severe damage to the internal organs of both men and women.
Can penicillin cause gonorrhea?
If someone has a penicillin allergy, there is potential to have an adverse reaction to the antibiotic treatment for gonorrhea. Depending on personal health history, a physician will be able to prescribe an effective alternative for treating anyone with a penicillin allergy or who has a history of gonorrhea infection (s).
Can gonorrhea cause a rash?
In general, side effects from gonorrhea treatment can include temporary itching, rash or redness, and pain or discomfort at the injection site (buttocks), upset stomach, and yeast infections. If symptoms persist for longer than the treatment period, contact your physician immediately.
Can you take gonorrhea medication with an infected partner?
Do not share the medication with an infected partner. Failure to take all of the medication, as indicated, will result in the infection not being eradicated from the system and leaves opportunity for the gonorrhea infection to become further resistant to treatment and harder, if not impossible, to cure.
What percentage of patients with gonorrhea have disseminated gonococcal infection?
Disseminated gonococcal infection is rare, affecting 0.4 to 3 percent of patients with gonorrhea, 4 but it is the most common cause of infectious arthritis in sexually active, previously healthy patients. Because about 15 percent of patients presenting in a primary care setting have joint pain as a primary symptom, disseminated gonococcal infection should be considered. 12 Antibioticresponsive, culture-negative acute arthritis in a sexually active young person is most often caused by disseminated gonococcal infection. 1 Skin lesions are present in 75 percent of patients with bacteremia, including painless or painful petechiae, macules, papules, pustules, vesicles, and bullae. 12, 13 At presentation, some patients have asymmetric arthropathies or polyarthralgia. Joints commonly affected with tenosynovitis or septic arthritis include wrists, ankles, hands, and feet. Rare disease progression may result in perihepatitis, meningitis, or endocarditis. 12, 13
What is gonorrhea swab?
Gonorrhea is characterized by Gram stain of a urethral smear or cervical swab showing gram-negative intracellular diplococci. Speculum examination may not be necessary to diagnose gonorrhea in women because of the comparable effectiveness of blind vaginal swabs. 16 Urine nucleic acid amplification testing in women and men (and urine polymerase chain reaction testing in men) has comparable sensitivity and specificity to cervical and urethral samples. Urine polymerase chain reaction testing in women has a 55.6 percent sensitivity, 17 which is too low to recommend routine use. Cultures from skin lesions in disseminated gonococcal infections are usually negative, but joint aspirate may have greater yield. The workup should include evaluation for other causes of arthritis, and oral, genital, blood, and fluid aspirate cultures. 12, 13 Table 4 lists the diagnostic features of gonococcal infections. 1, 2, 4
How long does it take for gonorrhea to show?
1, 6 When symptoms occur, they typically appear two to five days after infection, but may take as long as 30 days to appear. Common signs and symptoms include dysuria and purulent penile discharge.
What is the purpose of gonorrhea screening?
It also recommends intensive behavioral counseling for persons with or at increased risk of contracting sexually transmitted infections.
Can gonorrhea cause synovial disease?
If left untreated, gonorrhea may cause pelvic inflammatory disease in women, or it may disseminate, causing synovial and skin manifestations. Urogenital N. gonorrhoeae infection can be diagnosed using culture or nucleic acid amplification testing.
Is azithromycin effective for pharyngeal infections?
This dosage is more effective for common pharyngeal infections than the previously recommended dose of 125 mg. Azithromycin may be used as an alternative treatment option for patients with previous allergic reactions to penicillin, but because of the likelihood of antimicrobial resistance, its use should be limited.