Explore
Upper GI bleeds occur when part of the upper digestive tract becomes injured or inflamed. A GI bleed is a symptom of another disorder rather than a health condition in itself. Doctors divide GI bleeds into upper and lower bleeds depending on the source of the blood.
What is an upper GI bleed?
Some potential complications of a GI bleed are: 1 cancer that progresses without treatment 2 serious blood loss that may be life threatening 3 heart attack and other heart health symptoms 4 infections 5 shock
What are the potential complications of a GI bleed?
Introduction Upper gastrointestinal (GI) bleeding is a significant cause of morbidity and mortality in the United States despite our best efforts at preventing the occurrence of ulcerations and advanced endoscopic therapies.
What is the prognosis of upper gastrointestinal bleeding (GI)?
Medications for prophylaxis may protect patients from upper GI bleeding. Pharmacologic treatment Aims of antisecretory therapy: Increasing intragastric pH < 6. Treatment of peptic ulcer disease. Control of symptoms.
What are the treatment options for upper GI bleeding?
What is the prognosis of a GI bleed?
Mortality ranged from 13% for Mallory-Weiss tear to 34% for gastritis & duodenitis, 38–41% for duodenal ulcer, gastric ulcer and oesophagitis, 52% for varices and 95% for upper GI malignancy (Table 2). Mortality was also higher for bleeds that occurred as inpatients (54%) than for bleeds presenting at admission (36%).
What is the mortality rate in patient with upper gastrointestinal bleeding?
Upper Gastrointestinal Bleeding is defined as hemorrhage originating from anywhere between the esophagus and the ligament of Treitz [1]. It is one of the most common gastrointestinal emergencies, with an average mortality rate of 10% [2, 3].
Can you survive a GI bleed?
Regardless of treatment, 102 patients survived the initial episode of lower GI bleeding by at least two weeks. During the median follow-up of 16 months, 14 patients (14 percent) had clinically significant rebleeding.
What does an upper GI bleed mean?
Upper GI bleeding (UGIB) is defined as bleeding derived from a source proximal to the ligament of Treitz. The image below depicts an ulcer with active bleeding. Upper gastrointestinal bleeding (UGIB). Ulcer with active bleeding.
What is the incidence of and mortality associated with acute GI tract bleeding?
Upper GI bleeding has been estimated to account for up to 20 000 deaths annually in the United States (international records are not available). The overall incidence of acute upper GI haemorrhage has been estimated to be 50 to 100 per 100 000 persons per year.
Can GI bleed lead to death?
A gastrointestinal bleed can cause: Shock. Anemia. Death.
What to do if bleeding is not severe?
If your bleeding is not severe, you might start by seeing your primary care provider. Or you might be referred immediately to a specialist in gastrointestinal disorders (gastroenterologist). Here's some information to help you get ready for your appointment.
What questions should I ask my doctor about a syringe?
Your doctor is likely to ask you questions, such as: 1 Have your symptoms been continuous or occasional? 2 How severe are your symptoms? 3 What, if anything, seems to improve your symptoms? 4 What, if anything, appears to worsen your symptoms? 5 Do you take non-steroidal anti-inflammatory medication, either over-the –counter or prescribed, or do you take aspirin? 6 Do you drink alcohol?
What is balloon assisted enteroscopy?
Balloon-assisted enteroscopy. A specialized scope inspects parts of your small intestine that other tests using an endoscope can't reach. Sometimes, the source of bleeding can be controlled or treated during this test. Angiography.
What tests are needed for occult bleeding?
Tests might include: Blood tests. You may need a complete blood count, a test to see how fast your blood clots, a platelet count and liver function tests. Stool tests. Analyzing your stool can help determine the cause of occult bleeding. Nasogastric lavage.
Can you take PPI if you have a bleed?
Once the source of the bleeding is identified, your doctor will determine whether you need to continue taking a PPI. Depending on the amount of blood loss and whether you continue to bleed, you might require fluids through a needle (IV) and, possibly, blood transfusions. If you take blood-thinning medications, including aspirin or nonsteroidal ...
Can a CT scan show a GI bleed?
A variety of other imaging tests, such as an abdominal CT scan, might be used to find the source of the bleed. If your GI bleeding is severe, and noninvasive tests can't find the source, you might need surgery so that doctors can view the entire small intestine. Fortunately, this is rare.
Does GI bleeding stop on its own?
Often, GI bleeding stops on its own. If it doesn't, treatment depends on where the bleed is from. In many cases, medication or a procedure to control the bleeding can be given during some tests.
How to stop bleeding in GI tract?
He or she can stop the bleeding by inserting tools through an endoscope, colonoscope, or sigmoidoscope to
What causes a bleed in the GI tract?
When infections or ulcers cause bleeding in your GI tract, health care professionals prescribe medicines to treat the problem.
What can a radiologist do to stop GI bleeding?
During an angiogram, a radiologist can inject medicines or other materials into blood vessels to stop some types of bleeding. Learn more about the procedures doctors use to diagnose GI bleeding. During certain diagnostic procedures, such as a colonoscopy, a doctor can stop GI bleeding.
How to treat a bleed?
Treatment during a diagnostic procedure 1 inject medicines into the bleeding site 2 treat the bleeding site and surrounding tissue with a heat probe, an electric current, or a laser 3 close affected blood vessels with a band or clip
What are the risk factors for GI bleeding?
Anyone can have a GI bleed, especially if they experience other digestive issues, such as colitis or peptic ulcers. Risk factors for GI bleeding include: using anticoagulants, which are a group of drugs that can thin the blood and may therefore increase bleeding.
Where does GI bleeding occur?
Gastrointestinal (GI) bleeding is bleeding in the digestive tract, anywhere from the throat to the rectum. A person can experience a small loss of blood, such as when a hemorrhoid bleeds, or a hemorrhage, which causes a substantial blood loss. In this article, we discuss GI bleeding, its symptoms, severity, potential causes, risk factors, ...
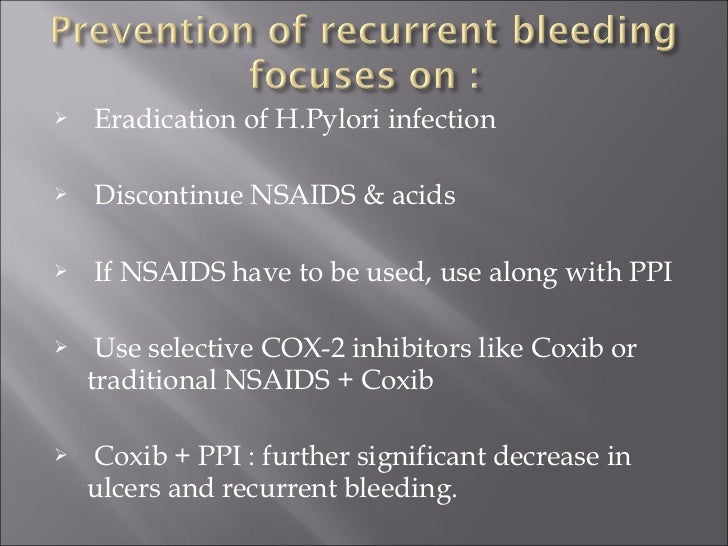
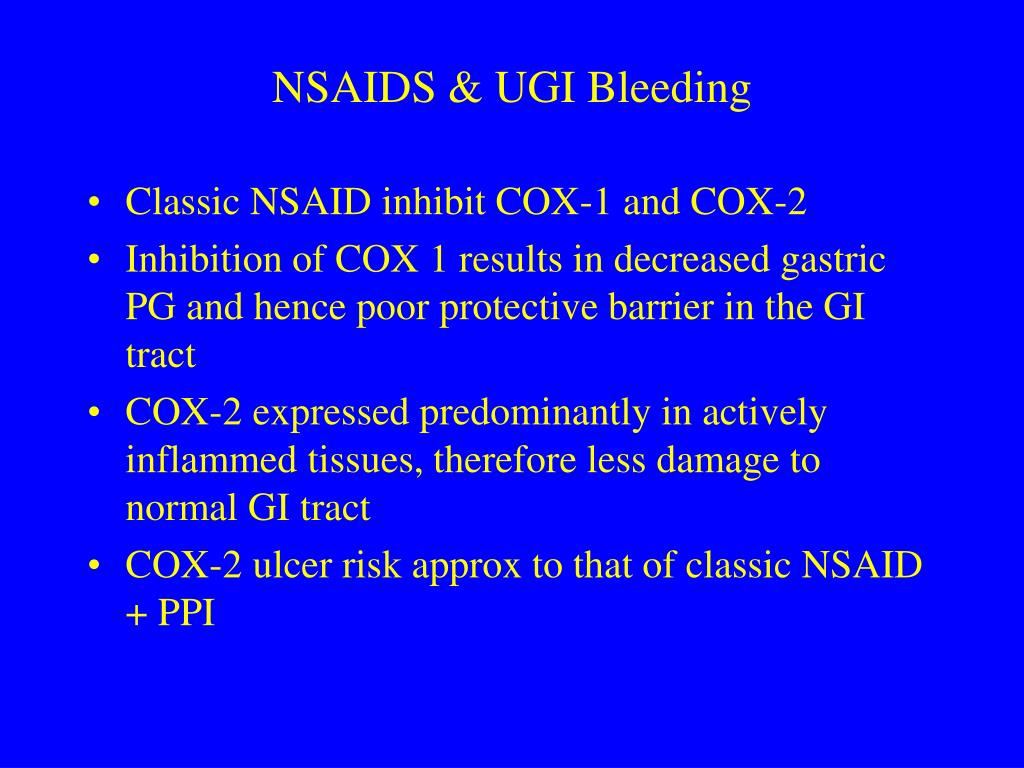
Why does my stomach burn when I have peptic ulcers?
Bleeding peptic ulcers. Peptic, or stomach, ulcers may be due to a Helicobacter pylori infection or overuse of nonsteroidal anti-inflammatory drugs (NSAIDs). A person with peptic ulcers may experience a burning sensation in the stomach. To help treat these, doctors may prescribe medication.
How do you know if you have a GI bleed?
they have lost a significant amount of blood, for example, by constantly bleeding from the rectum or mouth.
What is the name of the enlarged blood vessels in the upper GI tract?
Varices. Varices are enlarged blood vessels in the upper GI tract, usually in the esophagus, or food pipe. They can be a result of cirrhosis, which is a serious liver condition. A doctor may stop bleeding from varices with the use of elastic bands.
What does it mean when you have blood on your toilet paper?
blood on toilet paper or baby wipes after wiping. bleeding from the anus. red blood in stool. A serious, significant bleed, especially in the upper GI tract, may cause other symptoms, such as: little or no urine to pass. a drop in blood pressure . confusion. intense nausea. loss of consciousness.
Why do I have GI bleeding?
GI bleeding is a type of bleeding that occurs anywhere in the digestive system. It may be due to an injury, infection, or inflammation. The bleeding may appear suddenly and produce a lot of blood, or a person may notice gradual or periodic bleeding. Sudden, heavy bleeding is more immediately dangerous. However, both types of bleeding may signal ...
How to prevent GI bleeding?
Prevention. To help prevent a GI bleed: Limit your use of nonsteroidal anti-inflammatory drugs. Limit your use of alcohol. If you smoke, quit. If you have GERD, follow your doctor's instructions for treating it. By Mayo Clinic Staff. Gastrointestinal bleeding care at Mayo Clinic.
Why does my upper GI bleed?
Causes can include: Peptic ulcer. This is the most common cause of upper GI bleeding. Peptic ulcers are sores that develop on the lining of the stomach and upper portion of the small intestine. Stomach acid, either from bacteria or use of anti-inflammatory drugs, damages the lining, leading to formation of sores.
What does GI bleeding mean?
Overview. Gastrointestinal (GI) bleeding is a symptom of a disorder in your digestive tract. The blood often appears in stool or vomit but isn't always visible, though it may cause the stool to look black or tarry. The level of bleeding can range from mild to severe and can be life-threatening.
What causes sores in the colon and rectum?
Inflammatory bowel disease (IBD). This includes ulcerative colitis, which causes inflammation and sores in the colon and rectum, and Crohn's disease, and inflammation of the lining of the digestive tract. Tumors.
Why do hemorrhoids bleed?
They're often due to obstructed blood flow through the portal vein, which carries blood from the intestine, pancreas and spleen to the liver. Hemorrhoids are swollen veins in your lower rectum. Internal hemorrhoids are usually painless, but tend to bleed.
What causes a lot of bleeding in the esophagus?
Tears in the lining of the tube that connects your throat to your stomach (esophagus). Known as Mallory-Weiss tears , they can cause a lot of bleeding. These are most common in people who drink alcohol to excess. Abnormal, enlarged veins in the esophagus (esophageal varices).
What happens if you bleed suddenly?
If your bleeding starts abruptly and progresses rapidly, you could go into shock. Signs and symptoms of shock include: Drop in blood pressure. Not urinating or urinating infrequently, in small amounts. Rapid pulse.
What is GI bleeding?
Gastrointestinal (GI) bleeding is when bleeding occurs in any part of the gastrointestinal tract. The GI tract includes your esophagus, stomach, small intestine, large intestine ( colon ), rectum, and anus. GI bleeding itself is not a disease, but a symptom of any number of conditions.
What causes a lower GI bleed?
gastritis (bleeding in the stomach), esophageal varices, cancers, and. inflammation of the GI lining from ingested materials. The most common causes and risk factors for lower GI bleeding include. Diverticular disease ( diverticulitis) gastrointestinal cancers,
How to treat anal fissures?
Hemorrhoids or anal fissures may be treated with a diet high in fiber, fluids to keep stools soft may be helpful, and stool softeners if necessary. If they do not heal, they may need to have surgery to remove or fix them. Serious gastrointestinal bleeding can destabilize the vital signs of a patient.
What causes a bleed in the stomach?
Breakdown of the mucosal lining results in damage to blood vessels, causing abdominal bleeding. Gastritis: General inflammation of the stomach lining, which can result in bleeding in the stomach. Gastritis also results from an inability of the gastric lining to protect itself from the acid it produces.
What lab test is used to determine the severity of bleeding?
Lab tests such as complete blood count ( CBC ), serum chemistries, liver tests, and coagulation studies also can be helpful to determine the rate or severity of bleeding and to determine factors that may contribute to the problem. The doctor may need to perform a procedure called an endoscopy or a colonoscopy.
How do you know if you have GI bleeding?
Symptoms of GI bleeding often first appear as blood in the vomit or stool, or black, tarry stools. The person also may experience abdominal pain. Symptoms associated with the blood loss include. fatigue, weakness, pale skin, and. shortness of breath.
What is the best medicine for a large amount of blood in the upper GI tract?
If a large amount of blood is in the upper GI tract, patients may be given prokinetics (medications that help stomach emptying) such as erythromycin or metoclopramide ( Reglan) to help clear the stomach of blood, clots, or food residue before an endoscopy procedure to clear the stomach.
Why does my GI bleed?
The following are common causes: Inflammation, ulcers, or infection in your digestive tract. Swollen blood vessels in your digestive tract that break open and bleed. Tears in the lining of your esophagus caused by forceful, repeated vomiting.
What is the procedure to stop GI bleeding?
Other procedures, such as banding, may be used. Banding uses a plastic band to cut off the blood supply to a blood vessel. This stops the bleeding in your digestive tract. Surgery may be needed to find and stop GI bleeding.
What does it mean when you vomit?
Blood in your vomit, or vomit that looks like coffee grounds. Dark or bright red blood in your bowel movements. Bleeding from your rectum. Cramping or pain in your abdomen. Fatigue, weakness, or dizziness. Shortness of breath. Pale skin or gums, and sweaty or clammy skin. Faster heartbeat than usual.
How to stop bleeding after colonoscopy?
Medicine may be injected into your esophagus, stomach, or intestines to stop bleeding. Heat or an electrical current may also be applied to stop bleeding. Other procedures, such as banding, may be used.
What are some examples of GI conditions?
Manage GI conditions as directed. Examples of GI conditions include gastroesophageal reflux, peptic ulcer disease, and ulcerative colitis. Take all medicines for these conditions as directed. Limit or do not take NSAIDs. Ask your healthcare provider if it is safe for you to take NSAIDs.
Where does GI bleeding occur?
GI bleeding may occur in any part of your digestive tract. This includes your esophagus, stomach, intestines, rectum, or anus. Bleeding may be mild to severe. Your bleeding may begin suddenly, or start slowly and last for a longer period of time. Bleeding that lasts for a longer period of time is called chronic GI bleeding.
Can blood thinners cause GI bleeding?
You may need medicine to reverse the effects of blood thinner medicine. You may need any of the following to find the cause of GI bleeding: Blood tests may be done to measure your blood cell levels. This information will tell healthcare providers how much blood you have lost.
