
An enzyme called acetylcholinesterase breaks down acetylcholine. Some drugs that are used to treat myasthenia gravis act on acetylcholinesterase to stop the breakdown of acetylcholine. These acetylcholinesterase inhibitors increase the amount of acetylcholine available and so help muscle activation and contraction.
What are cholinesterase inhibitors used for in myasthenia gravis?
Oct 13, 2014 · An enzyme called acetylcholinesterase breaks down acetylcholine. Some drugs that are used to treat myasthenia gravis act on acetylcholinesterase to stop the breakdown of acetylcholine. These acetylcholinesterase inhibitors increase the amount of acetylcholine available and so help muscle activation and contraction. Study characteristics
How do medications treat myasthenia gravis?
Jul 24, 2016 · Treatment with Cholinesterase Inhibitors Cholinesterase inhibitors are drugs that prevent the degradation of acetylcholine (ACh) by acetylcholinesterase (also known simply as cholinesterase [ChE]). By preventing the inactivation of ACh, cholinesterase inhibitors enhance the actions of ACh released from cholinergic neurons.
How are cholinesterase inhibitors used to treat multiple sclerosis (MS)?
Secondary outcome measures(1) Improvement in the presenting symptoms more than 14 days after the start of treatment.(2) Change in impairment measured by a recognised and preferably validated scale, such as the quantitative myasthenia gravis score, within one to 14 days and more than 14 days after the start of treatment.(3) Myasthenia Gravis ...
Should acetylcholinesterase inhibitors be the first line of treatment for MG?
Oct 13, 2014 · An enzyme called acetylcholinesterase breaks down acetylcholine. Some drugs that are used to treat myasthenia gravis act on acetylcholinesterase to stop the breakdown of acetylcholine. These acetylcholinesterase inhibitors increase the amount of acetylcholine available and so help muscle activation and contraction. Study characteristics
How do medications that improve the symptoms of myasthenia gravis work?
Acetylcholinesterase inhibitors are the first-line treatment for myasthenia gravis. They relieve MG symptoms by increasing the amount of acetylcholine at the junctions between nerves and muscles. This increases muscle strength and reflex times but does not address the underlying autoimmune condition.Apr 6, 2021
How does a cholinesterase inhibitor work?
How do cholinesterase inhibitor drugs work? Cholinesterase inhibitor drugs stop or inhibit enzymes from breaking down acetylcholine when it travels from one cell to another.
How does myasthenia gravis treatment work?
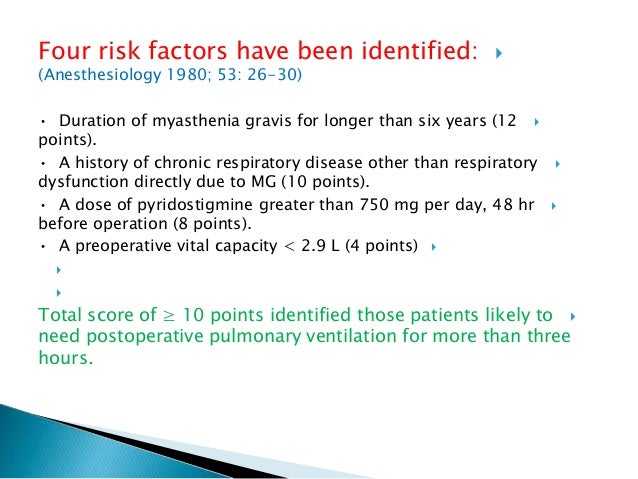
The first medicine used for myasthenia gravis is usually a tablet called pyridostigmine, which helps electrical signals travel between the nerves and muscles. It can reduce muscle weakness, but the effect only lasts a few hours so you'll need to take it several times a day.
Which cholinesterase inhibitor can be used in the treatment of myasthenia gravis?
Now, the most commonly used acetylcholinesterase inhibitors for myasthenia gravis are neostigmine and pyridostigmine. These medications can be administered orally, intravenously, or intramuscularly, while neostigmine can be also given subcutaneously to children.
How do cholinesterase inhibitors work in the treatment of Alzheimer's?
Donepezil, rivastigmine and galantamine all prevent an enzyme called acetylcholinesterase from breaking down acetylcholine. This means there is a higher concentration of acetylcholine in the brain, which leads to better communication between nerve cells. This may ease some symptoms of Alzheimer's disease for a while.Dec 22, 2021
What is the most effective treatment for myasthenia gravis?
There is no cure for myasthenia gravis, but it is treated with medications and sometimes surgery. You may be put on a drug called pyridostigmine (Mestinon), that increases the amount of acetylcholine available to stimulate the receptors.Mar 8, 2021
What does mestinon do for myasthenia gravis?
Pyridostigmine is used to improve muscle strength in patients with a certain muscle disease (myasthenia gravis). It works by preventing the breakdown of a certain natural substance (acetylcholine) in your body.
How does Thymectomy help myasthenia gravis?
Thymectomy, the surgical removal of the thymus gland (which often is abnormal in individuals with myasthenia gravis), reduces symptoms in some individuals without thymoma and may cure some people, possibly by re-balancing the immune system. Thymectomy is recommended for individuals with thymoma.
What is the effect of cholinesterase inhibitors on muscarinic receptors?
Consequently, cholinesterase inhibitors can be used to overcome excessive muscarinic blockade caused by atropine.
How does cholinesterase affect skeletal muscle?
The effects of cholinesterase inhibitors on skeletal muscle are dose dependent. At therapeutic doses, these drugs increase force of contraction. In contrast, toxic doses reduce force of contraction. Contractile force is reduced because excessive amounts of ACh at the NMJ keep the motor end-plate in a state of constant depolarization, thereby causing depolarizing neuromuscular blockade (see Chapter 16).
What is the effect of cholinesterase inhibitors on ACh?
Hence, the cholinesterase inhibitors can be viewed as indirect-acting cholinergic agonists. Since cholinesterase inhibitors can intensify transmission at all cholinergic junctions (muscarinic, ganglionic, ...
What is the treatment for myasthenia gravis?
Myasthenia Gravis. Pathophysiology. Treatment with Cholinesterase Inhibi tors. Cholinesterase inhibitors are drugs that prevent the degradation of acetylcholine (ACh) by acetylcholinesterase (also known simply as cholinesterase [ChE]). By preventing the inactivation of ACh, cholinesterase inhibitors enhance the actions of ACh released ...
What are the two types of cholinesterase inhibitors?
Cholinesterase inhibitors are also known as anticholinesterase agents. There are two basic categories of cholinesterase inhibitors: (1) reversible inhibitors and (2) “irreversible” inhibitors. The reversible inhibitors produce effects of moderate duration, and the irreversible inhibitors produce effects of long duration.
What happens when you have muscarinic stimulation?
Accumulation of ACh at muscarinic receptors can result in excessive salivation, increased gastric secretions, increased tone and motility of the GI tract, urinary urgency, bradycardia, sweating, miosis, and spasm of accommodation (focusing of the lens for near vision).
What are the drugs that are similar to neostigmine?
Ambenonium, edrophonium, and pyridostigmine. Ambenonium [Mytelase], edrophonium [Enlon, Reversol], and pyridostigmine [Mestinon] have pharmacologic effects much like those of neostigmine. One of these drugs—edrophonium—is noteworthy for its very brief duration of action. All three drugs are used for myasthenia gravis.
What is the purpose of acetylcholinesterase inhibitors in myasthenia gravis
Acetylcholinesterase inhibitors provide temporary symptomatic treatment of muscle weakness but there is controversy about their long-term efficacy, ...
How long does it take for a secondary outcome to be measured?
(2) Change in impairment measured by a recognised and preferably validated scale, such as the quantitative myasthenia gravis score, within one to 14 days and more than 14 days after the start of treatment.
What is the treatment for MG?
People who have moderate to severe MG or MG that is quickly getting worse are often given treatments in addition to acetylcholinesterase Inhibitors. This includes plasmapheresis, IVIG, and large doses of immunosuppressants. 2
Can MG cause side effects?
Side effects can vary depending on the specific drug you are taking. These drugs also work very differently from person to person. Some people with MG see great improvement, while others see little benefit. 2
How does cholinesterase work?
Mechanism of Action. Cholinesterase inhibitors function by inhibiting cholinesterase from hydrolyzing acetylcholine into its components of acetate and choline'; this allows for an increase in the availability and duration of action of acetylcholine in neuromuscular junctions. The cholinesterase enzyme has two active sites: an anionic site formed ...
What is a continuing education activity?
Continuing Education Activity. Cholinesterase inhibitors function to decrease the breakdown of acetylcholine. They SEe use in the treatment of Alzheimer and dementia symptoms. This activity describes the indications, action, and contraindications for cholinesterase inhibitors in treating dementia disorders and other uses within other specialties.
Why are cholinesterase inhibitors toxic?
Toxicity. The potential toxicity of cholinesterase inhibitors is due to their mechanism of action. The spectrum of toxicity can vary from patient to patient, which is also complicated by the type of cholinesterase inhibitor to which a patient suffers exposure.
What is the purpose of acetylcholinesterase inhibitors?
They are a group of drugs that block the normal breakdown of acetylcholine (ACh) into acetate and choline and increase both the levels and duration of actions of acetylcholine found in the central and peripheral nervous system. The acetylcholinesterase inhibitors have a variety of indications.
How do cholinesterase inhibitors affect AChE?
The cholinesterase inhibitor drugs inhibit AChE activity and maintain the ACh level by decreasing its breakdown rate.
What is neostigmine used for?
For example, neostigmine has a solution form used to counteract muscle relaxants at the end of surgeries. For patients with myasthenia gravis, an oral form of neostigmine is available for treatment.
What is the most sensitive sign of cholinergic toxicity?
Miosis is a common sign of cholinergic toxicity. The excess acetylcholine causes the contraction of the sphincter pupillae muscle that encompasses the iris. Miosis is considered one of the most sensitive signs of exposure to aerosol cholinesterase inhibitors (organophosphates, pesticides).
How to get rid of myasthenia gravis?
Lifestyle and home remedies. To help you make the most of your energy and cope with the symptoms of myasthenia gravis: Adjust your eating routine. Try to eat when you have good muscle strength. Take your time chewing your food, and take a break between bites of food.
What is the procedure to remove thymus gland?
Video-assisted thymectomy. In one form of this surgery, surgeons make a small incision in your neck or a few small incisions in the side of your chest. They then use a long, thin camera (video endoscope) and small instruments to see and remove the thymus gland. Robot-assisted thymectomy.
How long does plasmapheresis last?
However, the good effects usually last only a few weeks, and repeated procedures can lead to difficulty accessing veins for the treatment. Risks associated with plasmapheresis include a drop in blood pressure, bleeding, heart rhythm problems or muscle cramps.
What are the side effects of Rituximab?
Side effects, which usually are mild, can include chills, dizziness, headaches and fluid retention. Monoclonal antibody. Rituximab (Rituxan) and the more recently approved eculizumab (Soliris) are intravenous medications for myasthenia gravis. These drugs are usually used for people who don't respond to other treatments.
What is plasmapheresis?
Plasmapheresis (plaz-muh-fuh-REE-sis). This procedure uses a filtering process similar to dialysis. Your blood is routed through a machine that removes the antibodies that block transmission of signals from your nerve endings to your muscles' receptor sites.
How to get double vision?
To help you maintain your energy, try using an electric toothbrush, electric can openers and other electrical tools to perform tasks. Wear an eye patch . If you have double vision, an eye patch can help relieve the problem. Try wearing one to write, read or watch television.
How to prevent stumbles?
Use safety precautions at home. Install grab bars or railings in places where you need support, such as next to the bathtub or next to steps. Keep your floors clean, and move area rugs. Outside your home, keep paths, sidewalks and driveways cleared of leaves, snow and other debris that could cause you to stumble.
What is thymectomy treatment?
Surgical treatment (thymectomy) Drugs known as cholinesterase inhibitors offer relief from symptoms by blocking the action of acetylcholinesterase and increasing the amount of acetylcholine at the neuromuscular junction. (For a more detailed explanation of how these drugs work, see Causes/Inheritance .)
How does Soliris work in MG?
Soliris is thought to work in MG by inhibiting the complement pathway to prevent destruction of the NMJ.
What is the second therapeutic modality in MG?
The second therapeutic modality in MG is the administration of immunomodulating agents called corticosteroids. These drugs (which include prednisone and prednisolone) reproduce the actions of corticosteroid hormones, which are made by the outer layer of the adrenal gland.
How long does it take for azathioprine to work?
Azathioprine acts more slowly than corticosteroids, producing improvement after six to 12 months, and usually has few side effects. Occasionally, however, it can produce serious side effects including inflammation of the pancreas, liver toxicity, bone marrow suppression, and possibly an increased risk of cancer.
What is the best medication for MG?
The one most commonly used is pyridostigmine bromide (Mestinon).
What medications can unmask MG?
These include: Neuromuscular blocking agents used for anesthesia or intubation 1. Aminoglycoside and quinolone antibiotics 2. Cardiac anti-arrhythmics, such as all beta blockers and procainamide.
What is the best medicine for Wilson disease?
Local anesthetics, such as lidocaine and procaine if injected intravenously. Magnesium salts. Penicillamine used in other autoimmune diseases such as Wilson disease; it can induce MG 3. PD-1 inhibitors used as immunotherapy in certain cancers 4, 5, 6. Central nervous system depressants and opioids.
