
Levels of 50 nmol/L (20 ng/mL) or more are sufficient for most people. In contrast, the Endocrine Society stated that, for clinical practice, a serum 25 (OH)D concentration of more than 75 nmol/L (30 ng/mL) is necessary to maximize the effect of vitamin D on calcium, bone, and muscle metabolism [ 11, 12 ].
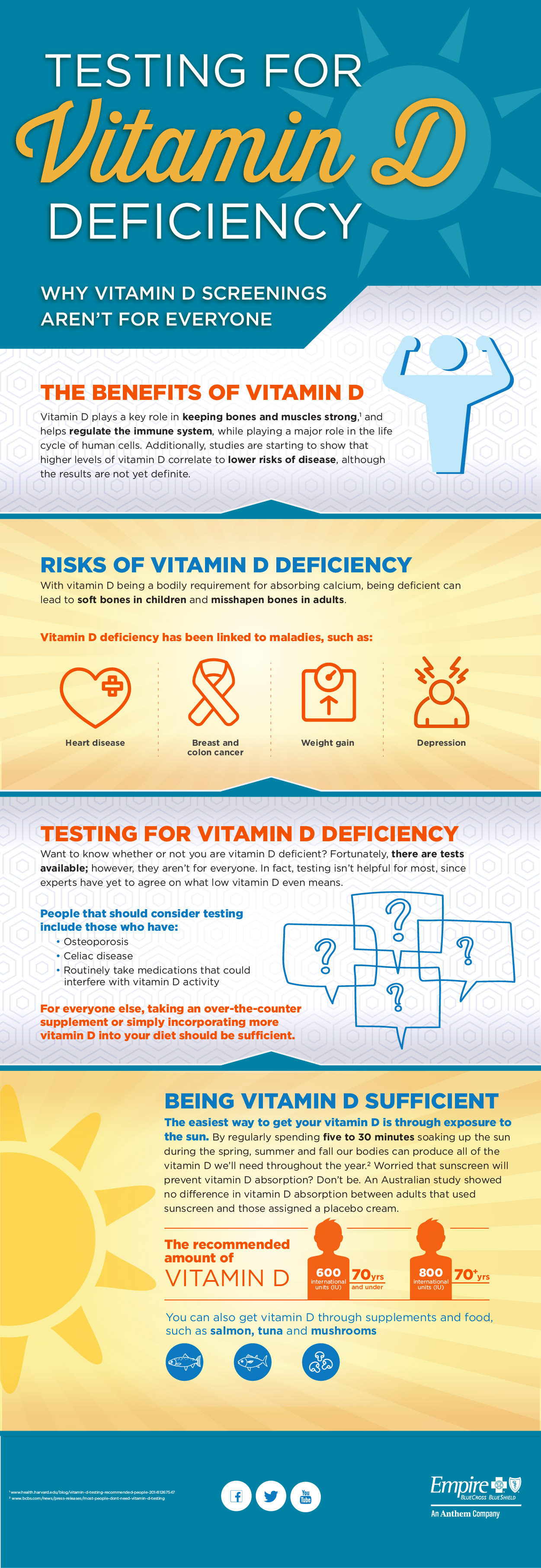
What are the daily recommendations of vitamin D?
- Deficient: Levels less than 12 ng/ml (30 nmol/l).
- Insufficient: Levels between 12–20 ng/ml (30–50 nmol/l).
- Sufficient: Levels between 20–50 ng/ml (50–125 nmol/l).
- High: Levels greater than 50 ng/ml (125 nmol/l).
How can I Raise my vitamin D levels quickly?
Spend time in sunlight
- Skin tone and age. People with darker skin need to spend more time in the sun to produce vitamin D than those with lighter skin.
- Geographical location and season. The closer you live to the equator, the more vitamin D you’ll be able to produce year-round because of your physical proximity to the sun’s rays.
- Sunscreen and clothing. ...
What is the best treatment for vitamin D deficiency?
- Stay out in the sun 15–20 minutes each day.
- Eat fatty fish.
- Take vitamin D supplement.
How much vitamin D should I take?
The Department of Health and Social Care recommends that adults and children over four take a daily supplement containing 10 micrograms of vitamin D throughout the year. But one question many people ask is 'when is the best time of day to take Vitamin D?'
At what level should vitamin D Be Treated?
Although there is no consensus on vitamin D levels required for optimal health -- and it likely differs depending on age and health conditions -- a concentration of less than 20 nanograms per milliliter is generally considered inadequate, requiring treatment.
How much vitamin D should I take if my level is 21?
Mayo Clinic recommends that adults get at least the RDA of 600 IU. However, 1,000 to 2,000 IU per day of vitamin D from a supplement is generally safe, should help people achieve an adequate blood level of vitamin D, and may have additional health benefits.
What level of vitamin D is severely low?
Older classifications considered 25(OH)D levels less than 12 ng/mL to be evidence of deficiency because symptoms were uncommon when levels were higher than this. Today, 25(OH)D less than 12 ng/mL is considered evidence of severe vitamin D deficiency.
Is 10000 IU of D3 too much?
The Endocrine Society Practice Guidelines recommend that up to 10,000 IUs daily was safe for adults. This is in contrast to the recommended UL at 4,000 IU/d from the IOM.
Can I take 5000 IU of vitamin D3 daily?
In summary, long-term supplementation with vitamin D3 in doses ranging from 5000 to 50,000 IUs/day appears to be safe.
How long does it take for vitamin D levels to return to normal?
If you've been prescribed high-dose vitamin D, work closely with your doctor to monitor your blood levels. It can take three months or more to bring them back up, but once they're good, you can stop the high doses and return to a lower vitamin D supplement for maintenance.
How quickly do vitamin D levels rise?
It can take anywhere from 1-6 months to raise vitamin D levels with supplements. How much your levels increase and how long it takes will depend on the dose and your baseline vitamin D levels.
How can I raise my vitamin D level quickly?
Spend time in sunlight. Vitamin D is often referred to as “the sunshine vitamin” because the sun is one of the best sources of this nutrient. ... Consume fatty fish and seafood. ... Eat more mushrooms. ... Include egg yolks in your diet. ... Eat fortified foods. ... Take a supplement. ... Try a UV lamp.
How much vitamin D is needed for bone health?
Vitamin D sufficiency is defined in terms of the serum level of the prohormone 25(OH)D required for bone health, which is 30 to 32 ng/mL. Maintenance of a 30 to 32 ng/mL serum level requires approximately 2,200 to 3,000 IU/d of vitamin D from all sources, including ultraviolet light exposure, food, and supplements.20,51,52Recommendations from the Institute of Medicine for vitamin D supplementation suggest 200 IU of vitamin D daily from birth through age 50 years, 400 IU/d for individuals age 51 to 70 years, and 600 IU/d for those age 70 years or older.53These recommendations presume some sun exposure and vitamin D intake from food and are not adequate to treat vitamin D deficiency.54,55Historically, the source of most vitamin D has been ultraviolet light–induced skin manufacture of cholecalciferol. A single whole-body dose of ultraviolet radiation associated with minimal erythema produces 10,000 IU of vitamin D.55Thus, 15 to 20 minutes of daily sun exposure without sunscreen in lower midwestern and southern latitudes between 10:00 amand 3:00 pmis usually sufficient to ensure adequate synthesis of vitamin D metabolites. Large excesses of vitamin D3 from prolonged sun exposure are destroyed in the skin, making vitamin D toxicity from sun exposure improbable.54,55In contrast, with the exception of coldwater ocean fish, food is a poor source of vitamin D.54Three ounces of herring, which few individuals eat, provides 1,300 IU of vitamin D, 3.5 oz of the more commonly ingested salmon provides 350 IU, and 1 teaspoon of cod liver oil provides approximately 400 IU. However, the amount of vitamin D in 1 cup of fortified milk or orange juice is only 100 IU, with 50-100 IU per cup of breakfast cereal or tablespoon of margarine.54,56,57Today, with more time spent indoors and increased use of sunscreen, higher basal intakes of 1,000 to 2,000 IU/d from supplements are recommended to avoid vitamin D deficiency.23,58–60Multiple vitamins generally contain 400 IU of vitamin D, and calcium supplements provide 200 to 400 IU of vitamin D. Vitamin D3 supplements without other additives are readily available over the counter in 400, 1,000, and 2,000 IU strengths at pharmacies and most grocery stores. These supplements are much smaller in size than pills containing calcium and vitamin D and generally cost $10 or less for a 3-month supply. At similar doses, vitamin D3 may be more potent than vitamin D2 (ergocalciferol), which is obtained from plants.61The Institute of Medicine lists 2,000 IU/d as the upper tolerable limit, but in fact, there is little evidence of toxicity unless doses of 10,000 IU of vitamin D3/d are exceeded.53,62
What is vitamin D adequacy?
Vitamin D adequacy is currently defined as a function of calcium homeostasis, with lower vitamin D levels resulting in reduced absorption of calcium from the gut and/or elevations of parathyroid hormone (PTH) considered in adequate. Blood levels of the prohormone 25(OH)D, with a half-life of 2 to 3 weeks, are used to describe vitamin D sufficiency rather than levels of 1,25(OH)2D, which has a half-life of only 3 to 4 hours.54,58Furthermore, in early vitamin D depletion, blood levels of 1,25(OH)2D can be misleading because they may rise initially in response to elevations in PTH, which is sensitive to reductions in 25(OH)D, before they begin to fall with prolonged precursor depletion.51,63
What are the symptoms of vitamin D deficiency?
Symptoms of vitamin D deficiency can be rather nonspecific and include fatigue, altered mood and depression, insomnia, nonradicular back pain, arthralgias (particularly of the wrists, ankles, shoulders, and shins), proximal muscle weakness, headache, and hair loss.76,77Symptoms are uncommon with 25(OH)D levels greater than 20 ng/mL, and even individuals with mild to moderate deficiency may not spontaneously complain of symptoms unless they are undergoing treatment that results in reduced formation of 1,25(OH)2D or decreased vitamin D receptor activation, such as estrogen depletion as the result of aromatase-inhibitor therapy. In a pilot study, we found that 50,000 IU of vitamin D3 weekly for 12 weeks was effective in treating vitamin D insufficiency in women receiving the aromatase inhibitor letrozole, and higher levels of 25(OH)D were associated with reduced disability from aromatase inhibitor–associated joint pain.78
What is the role of vitamin D in the body?
Vitamin D plays an important role in the homeostasis of a variety of organ systems, but its role in prevention of cancer and recurrence—along with necessary blood levels —has yet to be defined.
Why is vitamin D important?
Vitamin D is important in a number of physiologic processes, including calcium absorption, innate and adaptive immunity, and homeostasis of a number of organs. Chronic vitamin D deficiency in adults results in osteoporosis, osteomalacia, muscle weakness, and increased risk of falls.1–4Poor vitamin D intake and low blood levels of vitamin D metabolites are associated with increased incidence and severity of several autoimmune diseases involving the T helper type 1 lymphocyte,5,6including multiple sclerosis,7rheumatoid arthritis,8type I diabetes,9systemic lupus erythematosis,10and psoriasis.11,12Lower levels of vitamin D, adjusted for body mass index, are also associated with increased risk of hypertension, myocardial infarction, and death as a result of cardiovascular disease.13–16
What is the recommended level of 25(OH)D?
At the present time, 25(OH)D levels in the range of 30 to 60 ng/mL are considered optimal, but higher levels up to 100 ng/mL are often seen in individuals with outdoor occupations receiving intense sun exposure without ill effects.55Correlative studies of 25(OH)D with muscle strength or risk of breast or colon cancer have prompted several investigators to suggest that the optimal 25OHD target for multiple health outcomes is 40 to 50 ng/mL.19,20Garland et al23suggest that increasing 25(OH)D to a range of 40 to 60 ng/mL from the current US average could reduce risk of breast cancer by 25% and colon cancer by 27%. Intakes of at least 4,000 IU daily from all sources would be needed to maintain 25(OH)D levels of 40 to 60 ng/mL. Practically speaking, supplements of 2,000 IU daily plus some sun exposure would probably be required to maintain a 25(OH)D level of 40 to 60 ng/mL year round.23
How much calcium is needed for 25(OH)D?
Because increases in intestinal calcium absorption continue until 25(OH)D reaches a minimum of 30 ng/mL, and PTH continues to decrease until this level is reached,64,65a 25(OH)D serum level of 30 to 32 ng/mL is considered sufficient and levels of 20 to 29 ng/mL insufficient.
What is the relationship between calcium and phosphorus?
In people with healthy kidneys and bones, normal serum levels of calcium and phosphorus are maintained predominantly through the interaction of 2 hormones: parathyroid hormone (PTH) and calcitriol. In the setting of vitamin D deficiency, secondary HPT causes both release of calcium stored in bone and resorption of calcium by the kidney to maintain normal serum calcium and phosphorus levels. Thus, vitamin D deficiency is usually accompanied by normal blood levels for calcium and phosphorus, high-normal or elevated levels of PTH, normal to elevated levels of total alkaline phosphatase, a low 24-hour urine calcium excretion rate, and low levels of total 25(OH)D. Patients with severe and long-standing vitamin D deficiency may present with overt hypocalcemia and/or hypophosphatemia, but this is the exception. Clinicians should not measure 1,25(OH)2D levels to diagnose hypovitaminosis D. Doing so can lead to an erroneous interpretation of vitamin D status because calcitriol levels are often normal or even elevated in patients with vitamin D deficiency as a result of elevated PTH levels.
What vitamin is needed for CKD?
Superimposed nutritional deficiency may aggravate secondary HPT both directly (as a result of low vitamin D levels) and indirectly (as a result of impaired vitamin D –mediated intestinal calcium absorption). Patients with stage I to III CKD should be tested and supplemented with vitamin D as needed to achieve optimal levels of 25(OH)D in addition to modifying calcium and phosphate intake. Emerging evidence is challenging our understanding of bone and vascular health in stage IV to V CKD, such that vitamin D, calcitriol, or vitamin D analogs should be used according to current CKD guidelines and under the guidance of a nephrologist.
How is vitamin D produced?
Vitamin D is produced by skin exposed to ultraviolet B radiation or obtained from dietary sources, including supplements. Persons commonly at risk for vitamin D deficiency include those with inadequate sun exposure, limited oral intake, or impaired intestinal absorption. Vitamin D adequacy is best determined by measurement of the 25-hydroxyvitamin D concentration in the blood. Average daily vitamin D intake in the population at large and current dietary reference intake values are often inadequate to maintain optimal vitamin D levels. Clinicians may recommend supplementation but be unsure how to choose the optimal dose and type of vitamin D and how to use testing to monitor therapy. This review outlines strategies to prevent, diagnose, and treat vitamin D deficiency in adults.
How much vitamin D should I take daily?
Since 1997, the Food and Nutrition Board has advised an AI of vitamin D of 200 to 600 IU/d.18The AI is “believed to cover the needs of all individuals” but “lack of data or uncertainty in the data” limit the ability to confidently determine a recommended daily allowance. The AI for vitamin D is based on maintenance of a total serum 25(OH)D level of at least 11 ng/mL.18Although these recommendations are the basis for the amounts of vitamin D used to fortify foods and provided in many supplements, it is widely accepted that they are outdated.22Revised dietary reference intakes from the Institute of Medicine are expected in 2010.
What is the best test for vitamin D?
Ingested and cutaneously produced vitamin D is rapidly converted to 25(OH)D, but in serum only a fraction of 25(OH)D is converted to its active metabolite 1,25(OH)2D. Thus, measurement of the total 25(OH)D level is the best test to assess body stores of vitamin D. The total 25(OH)D level allows for the diagnosis and monitoring of vitamin D deficiency, whereas quantification of 25(OH)D2and 25(OH)D3fractions may facilitate treatment monitoring. For example, in patients without clinical improvement after D2or D3supplementation, lack of increase in the corresponding 25(OH)D2or 25(OH)D3and total 25(OH) D levels may indicate inadequate dosing, nonadherence, or malabsorption. Some laboratory assays for vitamin D cannot differentiate between 25(OH)D2and 25(OH)D3and will only report a total 25(OH)D level. Some laboratory assays underdetect D2metabolites, which may give the appearance of ineffective D2supplementation.
How much vitamin D is needed for winter?
In northern latitude locations in particular, up to 73% of the population may have levels of less than 20 ng/mL during winter.16Thus, it is important to be aware that vitamin D levels are affected by both geographic and seasonal variability and that a person with an “optimal” level in the summer may well become “deficient” in the winter without any change in diet and as a result of changes in sun exposure.
What is the best way to determine vitamin D adequacy?
Vitamin D adequacy is best determined by measurement of the 25-hydroxyvitamin D concentration in the blood.
What vitamin deficiency causes rickets?
Associated with vitamin D deficiency, which can lead to rickets in infants and children and osteomalacia in adults. 30 to <50. 12 to <20. Generally considered inadequate for bone and overall health in healthy individuals. ≥50. ≥20. Generally considered adequate for bone and overall health in healthy individuals. >125.
How many people have osteoporosis?
More than 53 million adults in the United States have or are at risk of developing osteoporosis, which is characterized by low bone mass and structural deterioration of bone tissue that increases bone fragility and the risk of bone fractures [ 71 ]. About 2.3 million osteoporotic fractures occurred in the United States in 2015 [ 72 ]. Osteoporosis is, in part, a long-term effect of calcium and/or vitamin D insufficiency, in contrast to rickets and osteomalacia, which result from vitamin D deficiency. Osteoporosis is most often associated with inadequate calcium intakes, but insufficient vitamin D intakes contribute to osteoporosis by reducing calcium absorption [ 1 ].
Why is vitamin D important for muscle growth?
Vitamin D is also needed for the normal development and growth of muscle fibers. In addition, inadequate vitamin D levels can adversely affect muscle strength and lead to muscle weakness and pain (myopathy) [ 1 ].
How many people take vitamin D supplements?
The analysis of 2015–2016 data also showed that 28% of all individuals aged 2 years and older in the United States took a dietary supplement containing vitamin D [ 38 ]. In addition, 26% of participants aged 2–5 years and 14% of those aged 6–11 years took supplements; rates increased with age from 10% of those aged 12–19 years to 49% of men and 59% of women aged 60 and older. Total vitamin D intakes were three times higher with supplement use than with diet alone; the mean intake from foods and beverages alone for individuals aged 2 and older was 4.8 mcg (192 IU) but increased to 19.9 mcg (796 IU) when dietary supplements were included.
Why are rickets so rare?
The fortification of milk (a good source of calcium) and other staples, such as breakfast cereals and margarine, with vitamin D beginning in the 1930s along with the use of cod liver oil made rickets rare in the United States [ 28, 49 ]. However, the incidence of rickets is increasing globally, even in the United States and Europe, especially among immigrants from African, Middle-Eastern, and Asian countries [ 50 ]. Possible explanations for this increase include genetic differences in vitamin D metabolism, dietary preferences, and behaviors that lead to less sun exposure [ 44, 45 ].
What is the serum concentration of 25?
Serum concentration of 25 (OH)D is currently the main indicator of vitamin D status. It reflects vitamin D produced endogenously and that obtained from foods and supplements [ 1 ]. In serum, 25 (OH)D has a fairly long circulating half-life of 15 days [ 1 ]. Serum concentrations of 25 (OH)D are reported in both nanomoles per liter (nmol/L) and nanograms per milliliter (ng/mL). One nmol/L is equal to 0.4 ng/mL, and 1 ng/mL is equal to 2.5 nmol/L.
What is the role of vitamin D in the body?
Vitamin D has other roles in the body, including reduction of inflammation as well as modulation of such processes as cell growth, neuromuscular and immune function, and glucose metabolism [ 1-3 ]. Many genes encoding proteins that regulate cell proliferation, differentiation, and apoptosis are modulated in part by vitamin D. Many tissues have vitamin D receptors, and some convert 25 (OH)D to 1,25 (OH)2D.
