Peri-implantitis Treatment
- Nonsurgical Treatment. The different nonsurgical therapy of peri-implant disease comprises mechanical, chemical,...
- Surface Decontamination. Nonsurgical mechanical therapy has a predictable outcome in peri-implant mucositis cases.
- Citric Acid (CA). Although CA is used for cleaning implants, it is also the chemotherapeutic agent with the highest...
Full Answer
Is implantoplasty effective in the treatment of peri-implantitis?
The majority of surgical peri-implantitis treatment protocols suggests adjunctive use of systemic antibiotics to target specific putative bacteria.
What is the prevalence of peri implantitis?
agents or interventions for treating periimplantitis around oral implants. Primary outcome measures were implant failure, radiographic marginal …
What are the treatment options for peri-implant disease?
Authors' conclusions: There is no reliable evidence suggesting which could be the most effective interventions for treating peri-implantitis. This is not to say that currently used interventions are not effective.A single small trial at unclear risk of bias showed the use of local antibiotics in addition to manual subgingival debridement was associated with a 0.6 mm additional …
What is peri-implantitis and how is it treated?
· The only treatment that appears effective at resolving peri-implantitis appears to be surgical therapy. But surgical resective therapy is only partially effective. In 2003, Leonhardt found surgical and antimicrobial treatment effective in just over half of peri-implantitis lesions over a period of five years.
What is an effective method for treatment of peri-implantitis?
Abstract: Based on a high level of success, dental implant therapy has become a preferred means of treatment for a wide variety of oral problems related to historic or impending tooth loss.
How do you treat an infected peri-implant?
Antibiotics: in some cases, following non-surgical treatment, antibiotics may be given to help control the infection before other treatments are tried. Once the inflammation around the implant has been controlled, if the problem requires surgical treatment the dentist or periodontist will decide which approach to use.
How can peri-implantitis be prevented?
Because peri-implantitis often occurs from plaque and bacteria buildup at a dental implant site, it is crucial to practice excellent oral hygiene after dental implant surgery. This includes brushing and flossing twice a day and attending routine periodontal cleaning and maintenance appointments.
Can antibiotics cure peri-implantitis?
Four out of seven included systematic reviews concluded that no evidence exists for use of systemic antibiotics to improve the clinical outcomes in surgical treatment of peri-implantitis.
What happens when an implant gets infected?
As the infection attacks the bone, the bone begins to deteriorate. Thus, the implant loses its base of support and may start to feel loose. In severe cases, the infection can sneak into the bloodstream and cause systemic health issues. Surgical intervention is usually necessary to address peri-implantitis.
Which of the following drugs are used in implants?
Which of the following drugs are used in implants? Explanation: Drugs which are generally used for such implants are steroids like contraceptives, morphine antagonists like naltrexone for opioid-dependent addicts. Polymers used for making such implants are polymethacrylates, elastomers, etc.
How is peri implant mucositis diagnosed?
The diagnostic definition of peri-implant mucositis is based on following criteria: 1) presence of peri-implant signs of inflammation (redness, swelling, line or drop of bleeding within 30 seconds following probing), combined with 2) no additional bone loss following initial healing.
How common is peri-implantitis?
In fact, peri-implantitis is so common that more than 28 percent of patients with dental implants develop this inflammation. You can help avoid it by continuing good oral hygiene to avoid gum disease.
What antibiotics treat peri-implantitis?
Systemic Amoxicillin Plus Metronidazole in Peri-implantitis TreatmentCondition or diseaseIntervention/treatmentPhasePeri-implantitis Periodontal DiseasesDrug: amoxicillin 500 mg + metronidazole 500 mg Procedure: non-surgical periodontal and peri-implant treatmentPhase 4Nov 4, 2019
What are some topical antibiotics?
A variety of topical antibiotics are available such as bacitracin, mupirocin, gramicidin, fusidic acid and gentamycin. There is however some concern regarding the use of antibiotics because of the possible development of antibacterial resistance in the long term.
Which of the following medications are antibiotics?
Top 10 List of Generic Antibioticsamoxicillin.doxycycline.cephalexin.ciprofloxacin.clindamycin.metronidazole.azithromycin.sulfamethoxazole and trimethoprim.More items...•
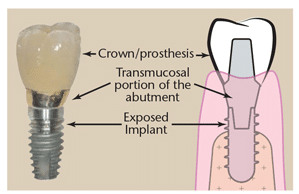
What is periimplantitis in dental implants?
Periimplantitis is one of the complications affecting oral implants. Its real incidence is probably underestimated and might be influenced by various factors including the characteristics of the implant surface and design7. If left untreated, it is very likely that periimplantitis will lead to the failure of the affected implant(s)4. This topic has grown in importance in the oral implant research agenda possibly because of the increased number of oral implants being placed and their longer followup periods, which inevitably means more cases of periimplantitis.
What is implant failure?
Implant failure, defined as implant mobility of previously clinically osseointegrated implants and removal of nonmobile implants because of progressive marginal bone loss or infection.
What is osseointegration in dentistry?
The now wellaccepted concept, osseointegration, has undoubtedly been one of the most significant scientific breakthroughs in dentistry over the past 30 years. A multitude of implant designs have been marketed since, and the clinical situations in which osseointegrated implantretained prostheses are used have expanded enormously.
What is peri-implantitis?
Peri-implantitis has been defined as a localized lesion involving bone loss around an osseointegrated implant.1 Its prevalence has been widely reported4 depending on the chosen threshold and specific study, varying from as low as two percent2 to as high as 58 percent3 of implants. Although a well-accepted threshold and prevalence is currently unavailable, it would appear that peri-implantitis occurs in about one out of every 10 implants.2-4 Despite this high frequency, treatment options for peri-implantitis are poorly studied. A 2011 Cochrane review concluded that the evidence available on peri-implantitis treatment is of insufficient quality and quantity and that more research is needed.28
What are the concerns of implantoplasty?
Implantoplasty provides an absolute decontamination of the implant surface, but four concerns exist: heat production, deposit of implant material into the surgical field, damage to the implant surface and weakening of the implant structure.
Can periimplantitis be regenerated?
Unfortunately, not all peri-implantitis lesions are favourable to regeneration. For implants with thin facial and lingual walls, peri-implantitis typically does not produce a crater-form defect with four walls. In some of these cases, the defect will present as a complete loss of the surrounding bony walls leaving regeneration as an unpredictable treatment choice. Aljateeli et al. (2012) proposed a decision tree based upon the defect morphology.15 If the defect had sufficient walls (two or greater), regeneration was attempted, but if there was zero or one wall, an apically positioned flap (APF) was suggested with implantoplasty (i.e., drilling the implant surface to remove the threads and outer surface).15 The theoretical benefit of implantoplasty is the production of a surface that is less adherent to bacterial colonization and a form of surface decontamination.
Is peri-implantitis a surgical procedure?
The only treatment that appears effective at resolving peri-implantitis appears to be surgical therapy. But surgical resective therapy is only partially effective. In 2003, Leonhardt found surgical and antimicrobial treatment effective in just over half of peri-implantitis lesions over a period of five years.
Does peri-implantitis respond to oral hygiene?
Peri-implantitis lesions do not respond well to improved oral hygiene and professional cleanings as is highly effective with periodontitis.7,19 This is not to understate the importance of oral hygiene and professional maintenance in the prevention of peri-implantitis. But once peri-implantitis develops, conservative therapy appears ineffective.
Is peri-implantitis a serious complication?
Peri-implantitis is not only frequent, but a serious complication. Implants have the potential to last a patient’s entire life and peri-implantitis can lead to disintegration and early loss of implants and their supported prostheses.
Is peri-implantitis hard to treat?
Smoking and early disease development were associated with higher rates of relapse and surgical therapy with lower rates of relapse.27 This means peri-implantitis is not just hard to treat, but treated cases must be watched closely as relapse is common (Fig. 3).
How does antibiotic therapy help with peri-implantitis?
Systemic antibiotic therapy increases the host defense to eliminate the infection by combating subgingival pathogens that remain following mechanical therapy . The combination of antibiotics (local and systemic) can be more beneficial in peri-implant infections. Furthermore, systemic antibiotic prophylaxis by injecting antibiotics at the lesion lowers the risk of postoperative infection. The surgical treatment of peri-implantitis can be combined with hydrogen peroxide and systemic antibiotics. A study found that the surgical treatment of peri-implantitis is effective and that therapy outcomes are affected by implant surface characteristics. 47However, the benefits of systemic antibiotics are not sustained for over 3 years.
What are the causes of peri-implant disease?
4Periodontal health is influenced by various factors such as oral hygiene, genetic and epigenetic factors, systemic health, and nutrition. 56Peri-implantitis and periodontitis lesions both harbor Gram-negative anaerobic bacteria compared with healthy sites. However, peri-implantitis has higher microbial diversity than periodontitis. 7Moreover, peri-implantitis is penetrated predominantly by inflammatory cells, B-lymphocytes and plasma cells, and frequently lacks a protective tissue layer over the bone, which is typically present in periodontitis. Histologically, peri-implantitis lesions were twice as large and had more blood vessels and the infiltrate in the connective tissue compared with perodontitis. 8Peri-implantitis demonstrated a 97% higher matrix metalloproteinases (MMP) level, such as MMP-8, which was only 78% greater in chronic periodontitis compared with healthy gingiva. 9Furthermore, peri-implantitis tissue contains extracellular matrix antibodies. 10The disease progression rate is faster in peri-implantitis, which generates a faster and more severe loss of bone compared with periodontal disease. A nonlinear form of progressive bone destruction occurs over time in peri-implantitis, which maybe because of the differences in microorganisms at the implant sites, the host's defense mechanism, and absence of a periodontal ligament. 1112
What antibiotics are used for periimplantitis?
In peri-implantitis, the most commonly used local antibiotics are minocycline (MNO), doxycycline, gentamicin, and cefazolin. 434445
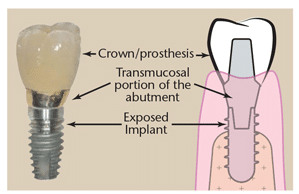
What is periimplant health?
Generally, a healthy peri-implant tissue shows no sign of inflammation, bleeding on probing (BOP), or increase in probing depth (PD) compared with the initial or baseline examination. The diagnostic definition of peri-implant health is based on the following criteria: (1) absence of peri-implant signs of soft tissue inflammation (redness, swelling, or profuse bleeding on probing), and (2) the absence of additional bone loss following initial healing. 29An increased PD might indicate attachment loss and supporting bone loss. 17The correct diagnosis is crucial to develop an appropriate treatment plan, leading to the successful treatment of peri-implant diseases.
Why do you need a baseline exam for peri implant?
Clinical and radiograph examination is necessary to diagnose peri-implant health and diseases. Therefore, a baseline clinical and radiographic examination is required when placing an implant. This information serves as a reference for evaluating physical or pathological changes in peri-implant tissues over time.
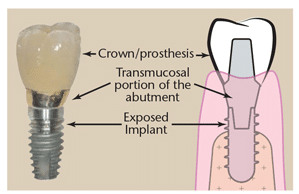
Can mechanical debridement remove mucositis?
However, it is more challenging when implant surfaces are exposed in peri-implantitis cases. Mechanical debridement alone may not completely remove the plaque because the instruments cannot access between the implant threads. 51Adjunctive treatments are proposed for surface decontamination to increase the efficiency of the nonsurgical treatment of peri-implant diseases.
What is the goal of periimplantitis?
The goal of peri-implantitis treatments is re-osseointegration or bone fill of the osseous defect to provide support to peri-implant soft tissue and thereby improve esthetic outcomes [2,22]; surgical regenerative approaches are indicated to achieve this goal. Nevertheless, these techniques are not always applicable due to varying defect morphologies and progressively advancing stages of the disease.
How to verify peri-implant osseointegration?
The classic method for verifying peri-implant osseointegration is light microscopy analysis of undecalcified sections of the bone to implant connection [14]. This method involves a qualitative and quantitative analysis. The qualitative analysis focuses on the identification and description of different tissues, specifically mineralized and unmineralized fibrous connective tissues. The quantitative analysis is defined by histomorphometry as it describes the characteristics at the bone-implant junction and in the surrounding peri-implant bone [15]. The standard parameters analyzed are the bone area fraction occupancy, bone-to-implant contact (BIC), and the mineral apposition rates. These parameter outcomes are related to the quality of the histological specimens and to the recognition of artifacts that can falsify the true nature of the bone–implant interface [16]. BIC has always been measured either histomorphometrically or radiographically.
What is the importance of implant surface decontamination?
The implant surface holds great importance on the success and speed of osseointegration. Different implant brands are characterized by varying treatment surfaces and roughness [30]. The question on implant surface characteristics and healing following surgical therapy to treat peri-implantitis is not new. It is demonstrated that, as part of the regenerative procedure, implant decontamination is essential to obtain positive outcomes [31]. The consensus report from the 8th European Workshop on Periodontology [32] stated that implant surface decontamination is a critical component of surgical treatment. Implant decontamination is aimed at removing bacterial biofilm and resolving infection and inflammation, rendering the surface biocompatible and conducive to bone regeneration and possible re-osseointegration, or at least minimizing bacterial adhesion [2]. Various techniques have been proposed for implant surface decontamination after surgical exposure: mechanical, chemical, laser or photodynamic, or a combination of these [33] (Figure 7). The decontamination process presents multiple challenges. Besides the attempts to solve the infectious process, the implant threads and rough surfaces pose a significant obstacle to the mechanical cleansing that, if not optimal, can lead to the reestablishment of pathogenic microflora and persistence of pathology [33]. In advanced peri-implant defect lesions, surface decontamination alone will not adequately achieve bone regeneration. In these cases, filling the defect with graft materials and growth factors yields better outcomes. Investigations on surgical treatment for peri-implantitis range from in-vitro and animal studies to human clinical trials. Each of these fields provided important insight on outcomes and healing processes. Due to the limitations of each model, study design, length of treatment, materials, outcome measures, and the heterogeneity of data, it is difficult to compare outcome measurements [31,33,34,35,36].
Why is periimplant defect morphology important?
Understanding the peri-implant defect morphology is important because of its potential for determining the likelihood of regeneration therapy success [25]. For situations in which regenerative procedures are unlikely to produce favorable results, resective surgeries may offer more clinical benefits. Of all the defect configurations, circumferential defects (Ie) achieved the highest reduction in PD and clinical attachment level (CAL) [26], while class Ib and Ic defects showed the poorest. Class Ib defects were the most prevalent in many of the studies. Therefore, it is more common to see peri-implantitis defect morphologies that are poorly responsive to reconstructive therapies (Figure 6).
What is the right panel of periimplant defect?
The right panel corresponds to the number of walls present in the representations. The higher the number of walls, the higher is the positive outcomes of regenerative therapy.
What are the factors that affect the success of periimplantitis regenerative procedures?
One of the most important factors related to the success of peri-implantitis regenerative procedures is the peri-implant bone defect configuration. These procedures are not aimed at addressing disease resolution but are an attempt to fill the defect created by the disease. The feasibility of this goal has been shown to be closely associated with the configuration of the peri-implant defect and the number of walls surrounding the lesion (Figure 3).
What is re-osseointegration?
Re-osseointegration or regeneration, by definition, is an event that can only be assessed histologically in experimental models [2,22]. The efficacy of peri-implantitis treatment can vary depending on the outcome variables [22]. In fact, clinical protocols are limited to bone level assessments by radiographs and clinical variables (BOP, PD, REC), while experimental protocols also include histological evaluations regarding inflammation resolution and osseous defect repair [22]. Clinicians cannot truly assess re-osseointegration on their patients unless a histological specimen is harvested and analyzed. Radiographic investigations are commonly used as the other non-invasive tool to assess bone changes after therapy [23], although questions regarding their reliability have been reported [16,24] (Figure 2). The most accurate solution to identify defect configuration is by direct access during the surgical intervention [25].