Explore
· The dosing for macrolides and doxycycline is as follows (see 'Risk factors for Pseudomonas or drug-resistant pathogens' above and "Treatment of community-acquired pneumonia in adults in the outpatient setting", section on 'Empiric antibiotic treatment'): • Azithromycin (500 mg once daily) • Clarithromycin (500 mg twice daily)
What are the guidelines for the management of community-acquired pneumonia in adults?
9 rows · · A CT scan of the chest will allow better definition of the extent of pulmonary infiltrate as well as ...
Which medications are used in the treatment of community acquired pneumonia (CAP)?
· Administration of corticosteroids within 36 hours of hospital admission for patients with severe community-acquired pneumonia decreases the risk of adult respiratory distress syndrome and length ...
What is the meaning of community acquired pneumonia?
for the treatment of community-acquired pneumonia in adults", section on Drug resistance and choice of therapy). Empiric therapy — Antibiotic therapy is typically begun on an empiric basis, since the causative organism is not identified in an
Can a decision aid improve outpatient treatment for pneumonia?
· The contribution of blood cultures to the clinical management of adult patients admitted to the hospital with community-acquired pneumonia: a prospective observational study. Chest . 2003;123:1142 ...
What is the standard treatment for community-acquired pneumonia?
The initial treatment of CAP is empiric, and macrolides or doxycycline (Vibramycin) should be used in most patients.
What is the first line treatment for hospital-acquired pneumonia?
In general, for both hospital-acquired pneumonia (HAP) and VAP, 7 days of treatment with appropriate antibiotics/antibiotics is recommended. This duration may be shortened or lengthened depending on the clinical response of the individual.
What is the first line treatment for pneumonia in adults?
The first-line treatment for pneumonia in adults is macrolide antibiotics, like azithromycin or erythromycin. In children, the first-line treatment for bacterial pneumonia is typically amoxicillin.
How is inpatient pneumonia treated?
The recommended empirical regimen for inpatients diagnosed with severe pneumonia is combination therapy with a beta-lactam plus a macrolide or a beta-lactam plus a fluoroquinolone.
What antibiotics are used to treat hospital-acquired pneumonia?
Treatment of Hospital-Acquired PneumoniaPiperacillin/tazobactam.Cefepime.Levofloxacin.Imipenem.Meropenem.
When Should a hospital be hospitalized for hats?
Answer. Although patients with mild community-acquired pneumonia (CAP) may be treated in an ambulatory setting, patients with CAP who are moderately to severely ill should be hospitalized. Underlying comorbidities often contribute to disease severity.
What IV antibiotics treat pneumonia?
Macrolides provide the best coverage for the most likely organisms in community-acquired bacterial pneumonia (CAP). Macrolides have effective coverage for gram-positive, Legionella, and Mycoplasma organisms. Azithromycin administered intravenously is an alternative to intravenous erythromycin.
How is pneumonia treated in adults?
The options include:Antibiotics. These medicines are used to treat bacterial pneumonia. ... Cough medicine. This medicine may be used to calm your cough so that you can rest. ... Fever reducers/pain relievers. You may take these as needed for fever and discomfort.
What antibiotics treat pneumonia in elderly?
The treatment should include a respiratory fluoroquinolone (levofloxacin or moxifloxacin) as monotherapy or the combination of a β-lactamic (third-generation cephalosporin, ertapenem or ampicillin/sulbactam) medication and a macrolide (azithromycin or clarithromycin).
What is the 2nd line antibiotic for pneumonia?
pneumoniae) are known. For the second agent, an alternative to azithromycin is a respiratory fluoroquinolone (levofloxacin [750 mg daily] or moxifloxacin [400 mg daily]). Regimens containing either a macrolide or fluoroquinolone have been generally comparable in clinical trials [32,37,48-51].
What is the typical duration of treatment for community acquired pneumonia hospitalized?
The guidelines suggested a minimum of 5 days of treatment, patients achieving an afebrile state for 48 to 72 hours, and patients meeting no more than 1 CAP-associated instability criteria before therapy discontinuation.
How is pneumonia treated in ICU?
These infections can be treated with one of the following antibiotics: ceftriaxone or fluoroquinolones (moxifloxacin or ciprofloxacin or levofloxacin) or ampicillin/sulbactam or ertapenem.
Is CAP a serious illness?
CAP is a common and potentially serious illness [ 1-5 ]. It is associated with considerable morbidity and mortality, particularly in older adult patients and those with significant comorbidities. (See "Prognosis of community-acquired pneumonia in adults" .)
What is HCAP in healthcare?
Health care-associated pneumonia (HCAP; no longer used) referred to pneumonia acquired in health care facilities (eg, nursing homes, hemodialysis centers) or after recent hospitalization [ 6,7 ]. The term HCAP was used to identify patients at risk for infection with multidrug-resistant pathogens.
Is omadacycline FDA approved?
Omadacycline is US Food and Drug Administration (FDA) approved for the treatment of CAP and has in vitro activity against common atypical and typical CAP pathogens, MRSA, many gram-negative rods (but not Pseudomonas spp), and anaerobes [ 124,125 ].
What is CA-MRSA?
Community-associated methicillin-resistant S. aureus (CA-MRSA) typically produces a necrotizing pneumonia with high morbidity and mortality. (See "Epidemiology, pathogenesis, and microbiology of community-acquired pneumonia in adults", section on 'S. aureus' .)
Is empirical therapy necessary for respiratory pathogens?
Initial empirical therapy active against these respiratory pathogens may be necessary only in selected patients presenting with specific epidemiologic, clinical, or immunologic risk factors for infection due to a particular pathogen. These risk factors and the specific pathogens that are involved are discussed below.
How many physicians are involved in the consensus document?
This consensus document was created by a multidisciplinary panel of 45 physicians with experience in the treatment of CAP in immunocompromised patients. The Delphi survey methodology was used to reach consensus.
What is CAP in medical terms?
Guidelines for the treatment of patients with community-acquired pneumonia (CAP) have been published by medical societies from several countries. These guidelines have improved the treatment and outcomes of patients with CAP, primarily by standardization of initial empirical therapy. But current society-published CAP guidelines exclude immunocompromised patients.
Why do we need a CT scan of the chest?
A CT scan of the chest will allow better definition of the extent of pulmonary infiltrate as well as better recognition of complications of pneumonia such as abscesses or pleural effusions. This information, gained by CT imaging of the chest, may help in the decision regarding hospitalization.
Why is deescalation important?
Deescalation of therapy is important because continuing broad-spectrum therapy for the full duration of therapy is associated with selection of multidrug-resistant organisms, increased risk of toxicity, drug-drug interactions, and impaired antimicrobial stewardship for the entire community.
What antibiotics are used for pneumonia?
Patients requiring hospitalization should be treated with a fluor oquinolone or a combination of beta-lactam plus macrolide antibiotics.
Do corticosteroids help with pneumonia?
For patients with severe community-acquired pneumonia, corticosteroids decrease the risk of adult respiratory distress syndrome and modestly reduce intensive care unit and hospital stays, duration of intravenous antibiotic treatment, and time to clinical stability without increasing major adverse events.
Is pneumonia a leading cause of death?
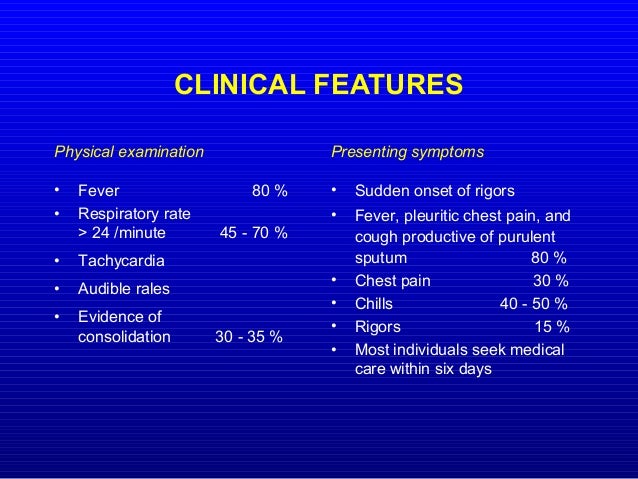
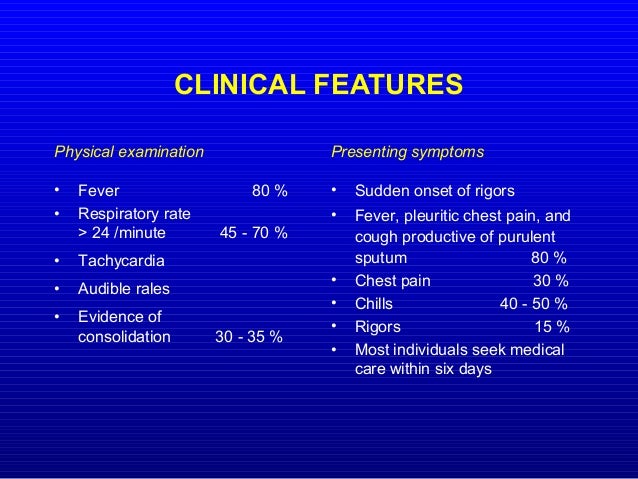
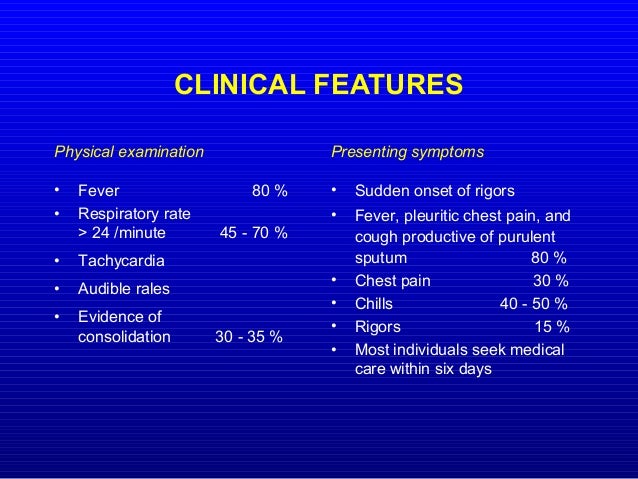
References. Community-acquired pneumonia is a leading cause of death. Risk factors include older age and medical comorbidities. Diagnosis is suggested by a history of cough, dyspnea, pleuritic pain, or acute functional or cognitive decline, with abnormal vital signs (e.g., fever, tachycardia) and lung examination findings.
What are the risk factors for pneumonia?
Community-acquired pneumonia is a leading cause of death. Risk factors include older age and medical comorbidities. Diagnosis is suggested by a history of cough, dyspnea, pleuritic pain, or acute functional or cognitive decline, with abnormal vital signs (e.g., fever, tachycardia) and lung examination findings.
How long does it take for corticosteroids to be administered?
Administration of corticosteroids within 36 hours of hospital admission for patients with severe community-acquired pneumonia decreases the risk of adult respiratory distress syndrome and length of treatment.
What are the symptoms of CAP?
Most patients with CAP present with a combination of cough, dyspnea, pleuritic pain, fever or chills, and malaise. Risk and severity of CAP, including infection with less common pathogens (e.g., Legionella species), increase with older age, cardiopulmonary disease, poor baseline functional status, low socioeconomic status, and recent weight loss or underweight status. 4, 9 Although a thorough history is an essential component in the diagnosis of CAP, no individual symptom can adequately predict its presence. Across four studies, the most predictive findings were fever greater than 100°F (37.8°C) (positive likelihood ratio [LR+] is approximately 2.7) and egophony (LR+ = 5.3). 13 Clinical prediction rules that combine symptoms and examination findings ( Table 2 14) can be helpful in generating a likelihood ratio that can be applied to patients with different prior probabilities of CAP and aid in diagnosis and management. 14
What are the tests for pneumonia?
Historically, common laboratory tests for pneumonia have included leukocyte count, sputum Gram stain, two sets of blood cultures, and urine antigens. However, the validity of these tests has recently been questioned after low positive culture rates were found (e.g., culture isolates of S. pneumoniae were present in only 40 to 50 percent of cases). 9 Such low positive culture rates are likely due to problems with retrieving samples from the lower respiratory tract, previous administration of antibiotics, contamination from the upper airways, faulty separation of sputum from saliva when streaking slides or plates, 9 or viral etiology. Furthermore, sputum samples are adequate in only 52.3 percent of patients with CAP, and only 44 percent of those samples contain pathogens. 10 Nonetheless, initial therapy often is guided by the assumption that the presenting disease is caused by a common bacterial pathogen.
What is pneumonia in lungs?
Pneumonia is an inflammation or infection of the lungs that causes them to function abnormally. Pneumonia can be classified as typical or atypical, although the clinical presentations are often similar. Several symptoms commonly present in patients with pneumonia.
What is a chest radiograph for pneumonia?
Chest radiography (posteroanterior and lateral views) has been shown to be a critical component in diagnosing pneumonia. 8 According to the latest American Thoracic Society (ATS) guidelines for the diagnosis and treatment of adults with CAP, “all patients with suspected CAP should have a chest radiograph to establish the diagnosis and identify complications (pleural effusion, multilobar disease).” 8 Chest radiography may reveal a lobar consolidation, which is common in typical pneumonia; or it could show bilateral, more diffuse infiltrates than those commonly seen in atypical pneumonia. However, chest radiography performed early in the course of the disease could be negative.
What is CAP in healthcare?
Community-acquired pneumonia (CAP) is defined as pneumonia not acquired in a hospital or a long-term care facility.
What are the symptoms of CAP?
Common clinical symptoms of CAP include cough, fever, chills, fatigue, dyspnea, rigors, and pleuritic chest pain. Depending on the pathogen, a patient’s cough may be persistent and dry, or it may produce sputum. Other presentations may include headache and myalgia. Certain etiologies, such as legionella, also may produce gastrointestinal symptoms.
What are the goals of pharmacotherapy for CAP?
The primary goals of pharmacotherapy for patients with CAP include eradicating the causative pathogens, resolving the clinical signs and symptoms, minimizing hospitalization, and preventing reinfection. 23 – 27 Physicians should choose a medication based on the pharmacokinetic profile, adverse reactions, drug interactions, and cost-effectiveness. 23 – 27 Further, patient evaluation should focus on severity of illness, patient age, comorbidities, clinical presentation, epidemiologic setting, and previous exposure. 9 The majority of patients with CAP are treated empirically based on the most common pathogen (s) associated with the condition. 23 – 27
What percent of CAP cases are fatal?
S. pneumoniae, which accounts for 60 to 70 percent of all bacterial CAP cases, can affect all patient groups and can cause a fatal form of CAP. The alarming rate of resistance to many commonly used antibiotics raises great concern. Penicillin-resistant S. pneumoniae was uncommon in the early 1990s but has since become increasingly prevalent. 29, 31
What is HCAP in nursing home?
HCAP was defined for those patients who had any one of several potential risk factors for antibiotic-resistant pathogens, including residence in a nursing home and other long-term care facilities, hospitalization for ≥2 days in the last 90 days, receipt of home infusion therapy, chronic dialysis, home wound care, or a family member with a known antibiotic-resistant pathogen. The introduction of HCAP was based on studies identifying a higher prevalence of pathogens that are not susceptible to standard first-line antibiotic therapy, in particular MRSA and P. aeruginosa, in some subsets of patients with CAP ( 123 ). Since then, many studies have demonstrated that the factors used to define HCAP do not predict high prevalence of antibiotic-resistant pathogens in most settings. Moreover, a significant increased use of broad-spectrum antibiotics (especially vancomycin and antipseudomonal β-lactams) has resulted, without any apparent improvement in patient outcomes ( 124 – 133 ).
What are the arguments for trying to determine the etiology of CAP?
Arguments for trying to determine the etiology of CAP are that 1) a resistant pathogen may be identified; 2) therapy may be narrowed; 3) some pathogens, such as Legionella, have public health implications; 4) therapy may be adjusted when patients fail initial therapy; and 5) the constantly changing epidemiology of CAP requires ongoing evaluation.
What test is used to test for influenza?
When influenza viruses are circulating in the community, we recommend testing for influenza with a rapid influenza molecular assay (i.e., influenza nucleic acid amplification test), which is preferred over a rapid influenza diagnostic test (i.e., antigen test) (strong recommendation, moderate quality of evidence).
What should be the focus of future RCTs?
Future well-designed RCTs should focus on therapies for patients at highest risk of death with severe pneumonia, as these are needed to assess the benefits and risks of combination β-lactam and macrolide therapy compared with β-lactam and respiratory fluoroquinolone therapy. Studies of fluoroquinolone monotherapy in severe CAP are also needed.
Can anaerobes be isolated?
Although older studies of patients with aspiration pneumonia showed high isolation rates of anaerobic organisms, more recent studies have shown that anaerobes are uncommon in patients hospitalized with suspected aspiration ( 119, 120 ). Increasing prevalence of antibiotic-resistant pathogens and complications of antibiotic use highlight the need for a treatment approach that avoids unnecessary use of antibiotics.
Can you take oseltamivir with CAP?
We recommend that antiinfluenza treatment, such as oseltamivir, be prescribed for adults with CAP who test positive for influenza in the inpatient setting, independent of duration of illness before diagnosis (strong recommendation, moderate quality of evidence).
How long does it take to stop antibacterial therapy?
Randomized controlled studies are needed to establish whether antibacterial therapy can be stopped at 48 hours for patients with CAP who test positive for influenza and have no biomarker (e.g., procalcitonin) or microbiological evidence of a concurrent bacterial infection.