
What is the 12-hour window for thrombolytic therapy?
Thrombolysis is the treatment of choice for acute stroke within 3 hours after symptom onset. Treatment beyond the 3-hour time window has not been shown to be effective in any single trial; however, meta-analyses suggest a somewhat less but …
How is blood pressure monitored during thrombolytic therapy for thrombotic agents?
Jun 17, 2021 · Patients receiving thrombolytic therapy must undergo a constant neurologic and cardiovascular evaluation with blood pressure monitoring every 15 minutes during and after tPA infusion for at least 2 hours, then half-hourly for 6 hours and …
When is thrombolytic therapy indicated in the treatment of myocardial infarction?
Mar 14, 2022 · As a result of ECASS III, many countries have amended the license for stroke treatment with rtPA to 4.5 hours following NCCT assessment. There has been much interest in using advanced imaging to visualise the volume of the penumbra and infarct core, particularly with a view to extending the treatment window for thrombolysis.
When is thrombolysis indicated in the treatment of hemophilia A?
Thrombolytics are drugs that. disintegrate existing blood clots. Thrombolytics are high-alert medications, as indicated by the Institute for Safe Medication Practices. For this reason, thrombolytics should only be given in a setting where patients can be closely monitored (e.g., intensive care unit).
What is the time frame for thrombolytic therapy?
Current US and international consensus guidelines accordingly recommend intravenous thrombolysis when treatment can be initiated within 3 hours from stroke onset, the most well-established treatment timeframe.5 May 2021
Why is there a 4 hour window for thrombolysis?
Thrombolysis can break down and disperse a clot that is preventing blood from reaching your brain. For most people, thrombolysis needs to be given within four and a half hours of your stroke symptoms starting.
What is the window period for thrombolysis in stroke?
Recombinant tissue plasminogen activator (r tPA) is currently the only Food and Drug Administration approved therapy for thrombolysis in acute ischemic stroke. [2,3,4] The recommended therapeutic window, ranges from 3 to 4.5 hours.
What is the golden window for thrombolysis therapy?
Importance: The effectiveness of intravenous thrombolysis in acute ischemic stroke is time dependent. The effects are likely to be highest if the time from symptom onset to treatment is within 60 minutes, termed the golden hour.
What is thrombolysis procedure?
Catheter-directed thrombolysis is a minimally invasive treatment that dissolves abnormal blood clots in blood vessels to help improve blood flow and prevent damage to tissues and organs.
How is thrombolysis administered?
Systemic thrombolysis is used for heart attack, stroke and pulmonary embolism. The “clot-busting” drug will be delivered through a peripheral intravenous (IV) line, usually through a visible vein in your arm. Performed at your bedside in an intensive care unit while your heart and lung functions are monitored.
What is the window of treatment for a stroke?
The full treatment time window for stroke is defined by the stroke onset to successful reperfusion time, and not by an arbitrary 4.5-hour or 6-hour or even 12-hour time window after onset. We recommend dividing this time window into 2 epochs with imaging time as the dividing instrument.25 Jun 2015
What is window period?
The window period refers to the time after infection and before seroconversion, during which markers of infection (p24 antigen and antibodies) are still absent or too scarce to be detectable.11 May 2021
What is window period of stroke?
The All India Institute of Medical Sciences (AIIMS) Rishikesh has set up an ultra modern 'Brian Stroke Treatment Unit' for the treatment of stroke patients. The director of the institute, Ravikant said that a window period of 4.5 hours is very crucial for the stroke patients.4 Aug 2020
What is IV thrombolysis?
Thrombolysis may involve the injection of clot-busting drugs through an intravenous (IV) line or through a long catheter that delivers drugs directly to the site of the blockage.7 Mar 2021
Who is eligible for thrombolysis?
Onset of symptoms less than three hours before beginning treatment. No head trauma or prior stroke in the past three months. No heart attack (myocardial infarction) in the past three months. No gastrointestinal or genitourinary hemorrhage in the past 21 days.7 Oct 2020
What drugs are used in thrombolytic therapy?
The three major classes of thrombolytic agents include tissue plasminogen activator, streptokinase, and urokinase fibrinolytic drugs. Each type dissolves blood clots in a slightly different way.30 Mar 2022
What is tpa therapy?
Currently, intravenous tPA is the only widely available therapy for acute ischemic stroke that has proved to be beneficial. 3 This therapy is effective for reducing neurological disability in selected patients who can be treated within 3 hours of stroke onset. The cost effectiveness of tPA therapy for acute stroke has been demonstrated. 4 The Food and Drug Administration (FDA) approved tPA for stroke treatment within 7 months of the publication of the NINDS rt-PA Acute Stroke Study, and guidelines endorsing the use of tPA for appropriate stroke patients have been issued by the National Institutes of Health, American Academy of Neurology, American Heart Association, and the American College of Chest Physicians. 567
How long after stroke can you give tPA?
Although intravenous tPA is beneficial when administered within 3 hours of stroke onset, large clinical trials have failed to document significant benefits when given in later time windows. This failure may have resulted in part because of inclusion of subgroups of patients who were unlikely to benefit from thrombolytic therapy. Preliminary data indicate that new MRI techniques are likely to be more effective than CT for identifying patients who may respond favorably to thrombolytic therapy between 3 and 6 hours after symptom onset. Clinical trials designed to convincingly establish whether specific MRI profiles are predictive of a favorable or unfavorable response to thrombolytic therapy are needed.
When was TPA used for stroke?
Background —Effective therapy was not available for treatment of acute stroke until 1995 , when tissue plasminogen activator (tPA) was shown to improve neurological and functional outcome in stroke patients who were treated within 3 hours of symptom onset.
What is diffusion weighted MRI?
Diffusion-weighted MR imaging is a new application of MRI technology that is capable of generating images based on a quantitative assessment of the random movement of water protons (diffusion) within tissues. 1415 This technique is ideal for assessment of acute brain ischemia, because the random movements of water protons are rapidly attenuated in regions of significant acute brain ischemia. 16171819 Although the pathophysiological explanation for the reduced diffusion of water within ischemic tissue is not completely understood, substantial experimental data indicate that this change is mediated by water movement from the extracellular to the intracellular space. 1920 Water within the extracellular space has relatively unrestricted diffusion, whereas the intracellular environment provides greater restriction to the random movements of water protons. During acute brain ischemia, it is well accepted that water moves from the extracellular to the intracellular environment after activation of excitatory amino acid receptors. In addition, loss of ion homeostasis occurs after significant energy depletion. 21 Experimental evidence suggests that cytotoxic edema which results from early energy depletion during acute experimental ischemic stroke is the key factor responsible for the changes seen on DWI during acute stroke. 19222324 Mild degrees of ischemia, insufficient to produce energy failure and cytotoxic edema, do not produce changes on DWI in experimental models. 25
What is PWI in MR?
PWI is another new MR technique that is complementary to DWI. Using a rapidly injected bolus of a contrast agent, a qualitative map of brain perfusion can rapidly be generated. 154445 Brain regions that are substantially hypoperfused are identified by the delayed arrival of the contrast agent to the vascular bed. A variety of hemodynamic maps can be created using PWI. In animal models, PWI lesions can be seen immediately after vessel occlusion and resolve rapidly after successful thrombolysis or reperfusion. 4647 In stroke patients, serial PWI studies can document the evolution of PWI lesions over time and help clarify if and when reperfusion occurs (Figure 1 ). Most stroke patients who do not receive thrombolytic therapy have PWI lesions that persist for at least 24 hours; patients who receive thrombolytics frequently demonstrate early reversal of PWI lesions. 124348
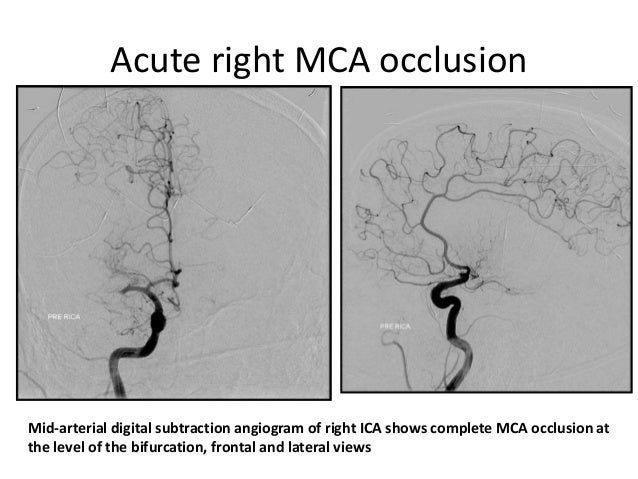
Can a complete occlusion of the distal internal carotid artery be recanal
Several investigators have reported that patients with complete occlusion of the distal internal carotid artery are unlikely to recanalize with intravenous thrombolytic therapy. 56 In contrast, patients with occlusions of proximal MCA branches are more likely to have early recanalization after thrombolysis. MRA can reliably differentiate these subgroups as well as identify patients who have evidence of intracranial or extracranial occlusions of other major vessels. Patients who have normal MRA studies may have undergone early spontaneous recanalization or have occlusions of small, deep penetrating branches. 54 Although it is unknown whether these patients will benefit from thrombolytic therapy, it has been hypothesized that substantial benefits are unlikely. 52
What is the goal of thrombolytic therapy?
The primary goal of thrombolytic therapy is rapid, complete, and sustained restoration of infarct artery blood flow. The GUSTO-I angiographic substudy strongly correlated 90-minute patency of the infarct-related artery with the mortality reduction achieved with accelerated alteplase. 7 Regardless of the thrombolytic agent used, an occluded infarct-related artery (ie, TIMI grade 0 or 1 flow) 8 at 90 minutes was associated with an 8.9% 30-day mortality rate, and “normal” perfusion (TIMI grade 3 flow) with a 4.0% mortality rate. Patients with “partial” perfusion (TIMI grade 2 flow, ie, infarct-related artery fills to full length but more slowly than adjacent normal vessels) had an intermediate mortality rate of 7.4%. In addition, at 5 to 7 days, left ventricular ejection fractions were higher, end-systolic volumes were smaller, and regional wall motion in the infarct zone was less depressed in patients with TIMI grade 3 flow than in those with lesser TIMI flow grades, 9 confirming the hypothesis that early perfusion at 90 minutes results in preservation of left ventricular function and reduced mortality.
How does thrombolytic therapy work?
Thrombolytic therapy works by lysing infarct artery thrombi and achieving reperfusion, thereby reducing infarct size , preserving left ventricular function, and improving survival.
Why are diabetics less likely to be treated with thrombolytic agents?
Diabetic patients have been less frequently treated with thrombolytic agents because of concerns about the increased risk of bleeding complications. The 1990 American College of Cardiology/American Heart Association guidelines for the management of acute myocardial infarction classified diabetic hemorrhagic retinopathy as an absolute contraindication against the use of thrombolytic therapy. 71 In the FTT analysis, however, the incidence of stroke and major bleeding complications after thrombolytic therapy was only slightly higher in diabetic patients (stroke, 1.9% versus 1.0%; major bleeding, 1.3% versus 1.0%), 38 and in the GISSI-2/International Study Group trial, the incidence of these complications was similar among diabetic and nondiabetic patients. 72 Intraocular hemorrhage and, more specifically, retinal bleeding are extremely uncommon complications of thrombolytic therapy. In the GUSTO-I study, 300 of the 6011 diabetic patients were estimated to have proliferative retinopathy, but none had intraocular hemorrhages, and the calculated upper 95% confidence limit of the possible occurrence of intraocular hemorrhage was only 0.05%. 73 It is unlikely that thrombolytic therapy would increase vitreous hemorrhage, which is due to vitreous detachment, in patients with diabetic retinopathy. Also, the few nondiabetic patients reported have shown no limitation of visual acuity at follow-up. 7475 Thus, the concerns many clinicians have about bleeding complications after thrombolysis in diabetic patients are not supported by the results of large-scale clinical trials.
When was thrombolytic therapy first used?
The first use of thrombolytic therapy in patients with acute myocardial infarction was reported by Fletcher and colleagues in 1958. 3 In the early 1960s and 1970s, 24 trials were performed evaluating the efficacy of intravenous streptokinase. 4 By modern standards, these trials had major design flaws.
Is thrombolysis a treatment for myocardial infarction?
Although thrombolysis has become the mainstay of acute treatment in the majority of patients with suspected acute myocardial infarction, uncertainties still remain with regard to the clinical benefit of this therapy in certain subgroups of patients.
Which protein is 136 amino acid?
Staphylokinase , a 136-amino-acid protein produced by certain strains of Staphylococcus aureus, has a unique mechanism of fibrin selectivity. 123 In two angiographic studies, recombinant staphylokinase (in doses between 20 and 30 mg) was at least as potent as alteplase and significantly more fibrin-specific. 124125
Should patients with anterior or inferior infarcts receive thrombolytic therapy?
Patients with anterior or inferior infarcts should receive thrombolytic therapy . Although inferior infarcts are usually smaller, the GISSI-1 trial showed that the benefit of thrombolytic therapy was related to the amount of ST-segment elevation rather than the site of the infarct. 53
