What are the key points of respiratory alkalosis?
Key Points. Respiratory alkalosis involves an increase in respiratory rate and/or volume (hyperventilation). Hyperventilation occurs most often as a response to hypoxia, metabolic acidosis, increased metabolic demands (eg, fever), pain, or anxiety.
How to treat respiratory alkalosis caused by overbreathing due to panic and anxiety?
The following strategies and tips are useful for respiratory alkalosis caused by overbreathing due to panic and anxiety. Fill the paper bag with carbon dioxide by exhaling into it.
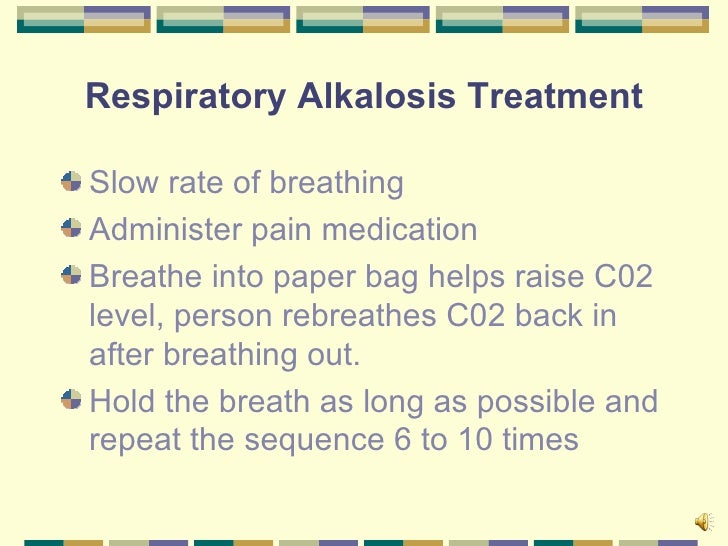
What is the treatment for respiratory alkalosis?
The treatment for respiratory alkalosis depends on the underlying cause. Treating the condition is a matter of raising carbon dioxide levels in the blood. The following strategies and tips are useful for respiratory alkalosis caused by overbreathing due to panic and anxiety. Fill the paper bag with carbon dioxide by exhaling into it.
What is the prognosis of respiratory alkalosis?
Respiratory alkalosis is not life threatening, so no interventions to lower pH are necessary. Increasing inspired carbon dioxide through rebreathing (such as from a paper bag) is common practice but may be dangerous in at least some patients with CNS disorders in whom CSF pH may already be below normal.

Do you give oxygen for respiratory alkalosis?
Respiratory alkalosis occurs when high levels of carbon dioxide disrupt the blood's acid-base balance. It often occurs in people who experience rapid, uncontrollable breathing (hyperventilation). Treatment includes supplemental oxygen and therapies to reduce the risk of hyperventilation.
Does respiratory alkalosis causes tachypnea?
Respiratory alkalosis can be acute or chronic. The chronic form is asymptomatic, but the acute form causes light-headedness, confusion, paresthesias, cramps, and syncope. Signs include hyperpnea or tachypnea and carpopedal spasms.
What happens to oxygen in respiratory alkalosis?
Respiratory alkalosis occurs when the levels of carbon dioxide and oxygen in the blood are not balanced. Your body needs oxygen to function properly. When you inhale, you introduce oxygen into the lungs. When you exhale, you release carbon dioxide, which is a waste product.
How do you compensate for respiratory alkalosis?
The kidney compensates in response to respiratory alkalosis by reducing the amount of new HCO3− generated and by excreting HCO3−. The process of renal compensation occurs within 24 to 48 hours. The stimulus for the renal compensatory mechanism is not pH, but rather Pco2.
What is immediate treatment of respiratory alkalosis?
Treatment is aimed at the condition that causes respiratory alkalosis. Breathing into a paper bag -- or using a mask that causes you to re-breathe carbon dioxide -- sometimes helps reduce symptoms when anxiety is the main cause of the condition.
Does hyperventilation increase o2?
Our data indicate that venous blood oxygenation level is higher during voluntary breath-holding and lower during hyperventilation.
What happens to PO2 during hyperventilation?
During hyperventilation, which lowered arterial PCO2 and increased pH of the blood, the average PO2 decreased in proportion to the decrease in arterial PCO2.
Why does metabolic acidosis cause tachypnea?
Metabolic acidosis from a range of causes can lead to tachypnea. As the body attempts to compensate for worsening acidosis, the respiratory rate increases to reduce the pCO2 and maintain a compensated physiological pH.
How do you correct alkalosis?
Metabolic alkalosis is corrected with the aldosterone antagonist spironolactone or with other potassium-sparing diuretics (eg, amiloride, triamterene). If the cause of primary hyperaldosteronism is an adrenal adenoma or carcinoma, surgical removal of the tumor should correct the alkalosis.
What intervention does the nurse provide to prevent respiratory alkalosis in the patient with hyperventilation?
During acute episodes of hyperventilation caused by panic or anxiety, instruct the patient to breathe into a paper bag. This simple yet effective strategy allows the patient to breathe the exhaled air back into the lungs and restore normal levels of carbon dioxide.
What does the compensatory mechanism do in alkalosis?
As a compensatory mechanism, metabolic alkalosis leads to alveolar hypoventilation with a rise in arterial carbon dioxide tension (PaCO2), which diminishes the change in pH that would otherwise occur.
How does hyperventilation correct acidosis?
Hyperventilation to normalize the pH during metabolic acidosis (phase 4), increased arterial O2 tension (313 +/- 44 mmHg, P < 0.05), and reduced shunt (from 20 +/- 5% to 12 +/- 3%, P < 0.05) compared with normal acid-base conditions (phase 1).
What is respiratory alkalosis?
Respiratory alkalosis is a primary decrease in carbon dioxide partial pressure (P co2) with or without compensatory decrease in bicarbonate (HCO 3− ); pH may be high or near normal. Cause is an increase in respiratory rate or volume (hyperventilation) or both. Respiratory alkalosis can be acute or chronic.
What causes cellular acidosis in the arterial blood?
Exhalation of large amounts of CO 2 causes respiratory alkalosis in arterial blood (hence on ABG measurements), but poor systemic perfusion and cellular ischemia cause cellular acidosis, leading to acidosis of venous blood.
What is the mechanism of carpopedal spasm?
Mechanism is thought to be change in cerebral blood flow and pH. Tachypnea or hyperpnea is often the only sign; carpopedal spasm may occur in severe cases due to decreased levels of ionized calcium in the blood (driven inside cells in exchange for hydrogen ion [H + ]).
Why does ventilation increase?
Ventilation increase occurs most often as a physiologic response to hypoxia (eg, at high altitude), metabolic acidosis , and increased metabolic demands (eg, fever) and, as such, is present in many serious conditions. In addition, pain and anxiety and some central nervous system (CNS) disorders (eg, stroke, seizure [post-ictal]) ...
Is alkalosis life threatening?
Treatment is directed at the underlying disorder. Respiratory alkalosis is not life threatening, so no interventions to lower pH are necessary. Increasing inspired carbon dioxide through rebreathing (such as from a paper bag) is common practice but may be dangerous in at least some patients with CNS disorders in whom the pH of cerebrospinal fluid may already be below normal.
Is respiratory alkalosis asymptomatic?
Respiratory alkalosis can be acute or chronic. The chronic form is asymptomatic, but the acute form causes light-headedness, confusion, paresthesias, cramps, and syncope. Signs include hyperpnea or tachypnea and carpopedal spasms. Diagnosis is clinical and with arterial blood gas (ABG) and serum electrolyte measurements.
What is respiratory alkalosis?
Respiratory alkalosis is a primary decrease in carbon dioxide partial pressure (P co2) with or without compensatory decrease in bicarbonate (HCO 3− ); pH may be high or near normal. Cause is an increase in respiratory rate or volume (hyperventilation) or both. Respiratory alkalosis can be acute or chronic.
What is the mechanism of carpopedal spasm?
Mechanism is thought to be change in cerebral blood flow and pH. Tachypnea or hyperpnea is often the only sign; carpopedal spasm may occur in severe cases due to decreased levels of ionized calcium in the blood (driven inside cells in exchange for hydrogen ion [H + ]).
Why does ventilation increase?
Ventilation increase occurs most often as a physiologic response to hypoxia (eg, at high altitude), metabolic acidosis, and increased metabolic demands (eg, fever) and, as such, is present in many serious conditions. In addition, pain and anxiety and some central nervous system (CNS) disorders (eg, stroke, seizure [post-ictal]) ...
Is alkalosis life threatening?
Treatment is directed at the underlying disorder. Respiratory alkalosis is not life threatening, so no interventions to lower pH are necessary. Increasing inspired carbon dioxide through rebreathing (such as from a paper bag) is common practice but may be dangerous in at least some patients with CNS disorders in whom the pH of cerebrospinal fluid may already be below normal.
Is respiratory alkalosis asymptomatic?
Respiratory alkalosis can be acute or chronic. The chronic form is asymptomatic, but the acute form causes light-headedness, confusion, paresthesias, cramps, and syncope. Signs include hyperpnea or tachypnea and carpopedal spasms. Diagnosis is clinical and with arterial blood gas (ABG) and serum electrolyte measurements.
How do you know if you have tachypnea?
The main symptoms are: feeling short of breath. a blue tint to the fingers and lips. pulling in, or retracting, the chest when breathing. Many diseases and conditions that cause tachypnea are treatable. The following are some of the most common causes.
Why do kids get tachypnea?
Children may get tachypnea when a viral respiratory infection causes fever or wheezing. Bronchitis and asthma can also cause tachypnea in children. More generally, many conditions can cause tachypnea, including pneumonia in its early stages. The main symptoms are: feeling short of breath.
What is the medical term for a lack of oxygen?
Anxiety or panic disorders. Treatment. Takeaway. Tachypnea is a medical term that refers to fast, shallow breathing. A lack of oxygen or too much carbon dioxide in the body is a common cause. It can also result from other health issues.
What is the best way to measure oxygen levels?
A doctor may use a pulse oximetry clamp to measure a person’s oxygen levels. Treatment options for tachypnea vary widely. If a doctor is not already aware of the underlying cause, they will conduct tests, look at a person’s medical history, and consider other symptoms. Some of the checks may involve:
Why does my breath get shorter?
Shortness of breath is a main symptom of tachypnea. One reason why a person breathes faster than normal is to take in more oxygen. The oxygen level in the body may be too low, or the carbon dioxide level may be too high. The body tries to correct this by breathing more quickly.
What happens to the lungs when a baby is born?
During development in the womb, the lungs contain fluid. As a baby reaches full term, their body starts to absorb the fluid so that their lungs can prepare to breathe air after birth. In some newborns, this fluid is not completely absorbed, resulting in rapid breathing.
What are the diseases that affect the lungs?
These diseases and conditions include: asthma . pneumonia. chronic obstruct ive pulmonary disease (COPD) pneumothorax, which is a collapsed lung. a pulmonary embolism, which is a blood clot or blockage in a lung’s artery. pulmonary fibrosis. cystic fibrosis. lung cancer.
What causes respiratory alkalosis?
Other causes of Respiratory Alkalosis include stroke, head injury and pulmonary emboli. Hypoxemia and a struggle to move as much air as possible to maintain adequate oxyenation will also make a person present with tachypnea.#N#Unless you are can do an ABG you will not know it is Respiratory Alkalosis. Even with an ABG it may be necessary to see more labs to determine the orgin which is why a chem panel for an anion gag is also done in the hospital upon arrival and sometimes even before the arterial stick.#N#The tachypnea can be from rising CO2 or a metabolic acidosis where the pH is becoming acidotic. Asthmatics and people with long disease processes are at example as are those who are in the latter stages of respiratory distress and about to go into failure. Children are another example. Placing their face in a paper or plastic bag like a nonrebreather with inadequate or no O2 flow to rebreathe their CO2 can sometimes be fatal.#N#Another bit of confusion is that placing someone on a nonrebreather mask automatically gives them almost 100% O2. If they are moving large tidal volumes and/or have a large overall minute volume, the actual FiO2 delivered may not be much more than a 5 or 6 liter nasal cannula. Real high flow oxygen devices are capable of delivering over 30 liters per minute to meet demand and maintain a high FiO2. It is possible whoever wrote the protocols might know the difference between delivery devices and the many causes for tachypneas which are not always "anxiety". It is impossible to teach all the differentials adequately in a 200 hour course.
Does increasing FiO2 help with respiratory alkalosis?
Increasing the FiO2 won't make a bit of difference for respiratory alkalosis. Not that it's a bad idea, but it's a hypoxia treatment, not an alkalosis treatment. And treatment should be aimed at treating the root cause: while anxiety cause hyperventilation is a common cause, there are other causes out there; we as providers need to use our tools and try to identify what's going on. Common causes of respiratory alkalosis (besides anxiety) are hypoxemia (perhaps due to anemia or hypoxia), sepsis (increased oxygen demand), and aspirin poisoning. Likewise, hyperventilation is a symptom of metabolic acidosis and shouldn't be corrected if it is a compensatory mechanism for something (such as DKA or shock).#N#When it comes to treating respiratory alkalosis, the focus is on reducing the pt's minute volume not increasing FiO2. So decreasing rate and decreasing tidal volume (if they are on a ventilator) is key; I find attentive coaching and calming words works well for conscious, awake patients. If protocols allow for it, a small benzodiazepine dose works wonders for anxiety. I'm curious how many people's protocols do allow for this; mine right now don't, but I've gotten online medical control to okay it in the past for a couple exceptional cases.
Can SImple masks cause CO2 retention?
SImple mask for CO2 retention: no. Especially mask without O2 flow; that is using the device improperly, you are off then reservation with that one. People can suffocate that way.#N#It is not impossible to diagnose differentially between psychologically rooted hyperventilatory alkalosis and some other cause of c/o shortness of breath coupled with deep rapid respirations, but then hanging around and figuring out what's causing it and using that data is asking for a fatality. Is the time worth it, and can the average EMT do it? Nope and nope.#N#O2 plus alkalosis: pt loses consciousness, and if its psychogenic, the situation resolves. If not, and they do need O2, it's already running.#N#Sidebar: aspirin: causes hyperventilation by stimulating the respiratory center? Dang. And the figure quoted on EMed:"Still, more than 10,000 tons of aspirin are consumed in the United States each year". And "Oil of Wintergreen"" (methyl salicylate): "One teaspoon of 98% methyl salicylate contains 7000 mg of salicylate, the equivalent of nearly 90 baby aspirins and more than 4 times the potentially toxic dose for a child who weighs 10 kg".
How to treat tachypnea in COPD?
You may need oxygen therapy if your blood oxygen concentration is low. 1
What are the effects of tachypnea?
Complications. Tachypnea can have some effects on the body. One of the most harmful effects is an acid-base imbalance. 1 This can occur as your rapid breathing causes an alteration in the ratio of gases (carbon dioxide and bicarbonate) in the body.
What is the diagnosis of COPD and tachypnea?
When you have COPD and tachypnea, your diagnosis will involve more factors than your respiratory rate. Your medical team will also work to diagnose the cause of your rapid breathing. Tests that can help identify the cause of tachypnea include: 2 .
How many breaths per minute for COPD?
If you take more than 20 breaths per minute for at least a few minutes, you would be described as having tachypnea. Typically, when you have COPD, you may feel a sense of discomfort during episodes of tachypnea. With COPD, you may experience tachypnea when you exert yourself physically or if you develop an infection.
What causes rapid breathing in COPD?
Physical exertion or exercise: Activity can trigger brief periods of rapid, shallow breathing, typically lasting for less than an hour. Lung infections: These are among the most common causes of episodic tachypnea in COPD.
What is the normal respiration rate for a healthy adult?
1 The normal respiratory rate for a healthy adult ranges from 12 to 18 breaths per minute.
What are some ways to treat tachypnea?
When tachypnea is caused by anxiety, strategies such as relaxation breathing, guided imagery, or meditation may help. Preventing Anxiety-Induced Tachypnea.
What are the effects of depletion of ions in the respiratory system?
Depletion of ions, such as potassium and phosphate, affect the respiratory muscles leading to acute respiratory failure [3]. Reduction in colloid osmotic pressure increases lung water content, leading to noncardiogenic pulmonary edema and decrease in lung compliance[4,5].
What is the most serious condition in which a person has a respiratory compromise?
Diabetes ketoacidosis is one of the most serious and acute complications of diabetes. At the time of presentation and during treatment of diabetic ketoacidosis (DKA), several metabolic and electrolyte derangements can ultimately result in respiratory compromise. Most commonly, hypokalemia, hypomagnesemia and hypophosphatemia can eventually lead ...
What are the intracellular ions that decrease in the blood?
Potassium, magnesium and phosphorous are intracellular ions which serum concentrations decrease as a direct consequence of hyperglycemia and ketoacidosis (potassium), or as a consequence of the correction of acidosis with insulin (magnesium and phosphorous).
What ions are retained in the kidneys during acidosis?
In an attempt to maintain osmolality, the kidneys will retain sodium ions at the expense of potassium ions[9]. Furthermore, when acidosis is present, hydrogen ions from the bicarbonate nucleus will be reabsorbed at the expenditure of potassium[10].
Can Kussmaul breathing pattern be hydrostatic?
Furthermore, tachypnea, hyperpnea and more severely, Kussmaul breathing pattern can develop. Also, hydrostatic and non-hydrostatic pulmonary edema can occur secondary to volume shifts into the extracellular space and secondary to increased permeability of the pulmonary capillaries.
Is DKA a respiratory failure?
Since respiratory failure in DKA is associated with increased morbidity and mortality, the recognition and treatment of those derangements have the potential to improve outcomes in DKA. INTRODUCTION. Diabetes ketoacidosis (DKA) is one of the most serious and acute complications of diabetes. It is characterized by moderate hyperglycemia (blood ...
Why do I have tachypnea?
Complications. While tachypnea can result from physiological causes such as exercise, there are pathologic causes that may be of concern.
What is tachypnea 2021?
Last Update: February 28, 2021. Continuing Education Activity. Tachypnea is defined as a breathing rate that is higher than the normal breathing rate. This condition is seen in both the physiologic state as well as as a symptom of pathology.
What is the normal breathing rate for an adult?
Tachypnea is a condition that refers to rapid breathing. The normal breathing rate for an average adult is 12 to 20 breaths per minute. In children, the number of breaths per minute can be a higher resting rate than seen in adults.
What is the term for rapid and shallow breathing?
Tachypnea is a term used to define rapid and shallow breathing, which should not be confused with hyperventilation, which is when a patient's breathing is rapid but deep. Both are similar in that both result from a buildup of carbon dioxide in the lungs, leading to increased carbon dioxide in the blood. [5]
How many breaths per minute is normal?
The normal breathing rate for an average adult is 12 to 20 breaths per minute. In children, the number of breaths per minute can be a higher resting rate than seen in adults. Etiology. Tachypnea does not necessarily have a pathological cause. For example, exercise can cause tachypnea.
How many babies have tachypnea?
It occurs in approximately 1 in 100 preterm infants, whereas, in term infants, it presents in about 4 to 6 per 1000 infants.
Can congestive heart failure cause tachypnea?
Congestive heart failure can also be a cause of tachypnea and , if not managed, can progress to worsening heart failure. Anxiety states and hyperventilation during panic attacks would lead to tachypnea and can lead to hypocapnia or reduced carbon dioxide levels, reducing respiratory drive.