Symptoms
Reactive thrombocytosis. Treatment for this condition depends on the cause. If you've had significant blood loss from a recent surgery or an injury, your elevated platelet count might resolve on its own. If you have a chronic infection or an inflammatory disease, your platelet count likely will remain high until the condition is under control.
Causes
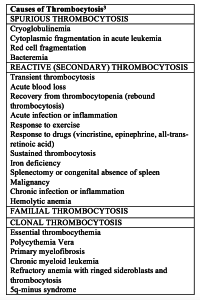
Reactive thrombocytosis is an elevated platelet count ( > 450,000/mcL [ > 450,000 × 10 9 /L]) that develops secondary to another disorder. (See also Overview of Myeloproliferative Neoplasms .) Some causes of reactive thrombocytosis include.
Prevention
Reactive Thrombocytosis (Secondary Thrombocythemia) Platelet function is usually normal. Unlike in essential thrombocythemia, reactive thrombocytosis does not increase the risk of thrombotic or hemorrhagic complications unless patients have severe arterial disease or prolonged immobility. With secondary thrombocytosis,...
Complications
Secondary thrombocytosis subsides when the underlying process causing the elevated platelet count resolves (treatment of infection, recovery from surgery, etc.). Even though the platelet count is elevated for a short time (or even indefinitely after splenectomy), secondary thrombocytosis does not...
What are the treatment options for reactive thrombocytosis?
What is reactive thrombocytosis (reactive platelet count)?
What is the prognosis of reactive thrombocytosis (secondary thrombocytes)?
When does secondary thrombocytosis subside?

When should you start treating thrombocytosis?
Treatment of essential thrombocythemia depends on your risk of blood clots or bleeding episodes. If you're younger than 60 and have had no signs or symptoms, you may simply need periodic medical checkups. Your doctor may prescribe medication if: You're older than 60 and have had previous blood clots or TIAs.
Do you treat reactive thrombocytosis?
Reactive thrombocytosis If you've had significant blood loss from a recent surgery or an injury, your elevated platelet count might resolve on its own. If you have a chronic infection or an inflammatory disease, your platelet count likely will remain high until the condition is under control.
How high do platelets need to be for thrombocytosis?
A normal platelet count ranges from 150,000 to 450,000 platelets per microliter of blood. Having more than 450,000 platelets is a condition called thrombocytosis; having less than 150,000 is known as thrombocytopenia. You get your platelet number from a routine blood test called a complete blood count (CBC).
Is thrombocytosis an emergency?
Summary. Thrombocytosis—having too many platelets in the blood—does not normally have symptoms. However, once diagnosed with thrombocytosis, any symptoms of blood clots should warrant seeking emergency medical help.
Does Covid cause reactive thrombocytosis?
These results provide new insights into the biology of thrombosis and hemostasis in COVID-19 patients where abnormalities in hematologic findings are common and difficult to interpret directly. The reactive thrombocytosis in COVID-19 patients seems to have important clinical correlations and deserves further research.
Is thrombocytosis serious?
Primary thrombocytosis, or essential thrombocythemia, can cause serious bleeding or clotting complications. These can usually be avoided by maintaining good control of the platelet count with medications. After many years of having the disease, however, bone marrow fibrosis (scarring) can develop.
Is 500 a high platelet count?
Normal platelet counts are in the range of 150,000 to 400,000 per microliter (or 150 - 400 x 109 per liter), but the normal range for the platelet count varies slightly among different laboratories. An elevated platelet count is known as thrombocytosis.
Does Covid affect platelet count?
In COVID-19 patients, platelet count differs between mild and serious infections. Patients with mild symptoms have a slightly increased platelet count, whereas thrombocytopenia is a hallmark of severe COVID-19 infections.
Is 600 a high platelet count?
Essential Thrombocythemia is also known as Essential Thrombocytosis or ET. ET is considered one of the myeloproliferative disorders and is characterized by persistently elevated platelet counts, usually >600.
Can thrombocytosis lead to leukemia?
In rare cases, essential thrombocytosis develops into polycythemia vera (PV), myelofibrosis, a myelodysplastic syndrome or acute myelogenous leukemia (AML).
Can stress cause high platelets?
Stressful life events and anxiety usually cause an increase in platelet volume and activity through various mechanisms. Mean platelet volume (MPV), which is indicative of platelet size, is accepted as an indication of platelet activity.
Is a platelet count of 450 high?
Diagnostic tests Platelets are the cells that help your blood to clot, and if you have ET, your bone marrow may be producing too many of these cells. A normal platelet count is 150 to 450 –– counts above 450 are considered higher than normal.
What is thrombocytosis in blood?
What is thrombocytosis? Thrombocytosis refers to having too many platelets in your blood. Platelets are blood cells in plasma that stop bleeding by sticking together to form a clot. Too many platelets can lead to certain conditions, including stroke, heart attack or a clot in the blood vessels.
What causes secondary thrombocytosis?
Secondary, or reactive, thrombocytosis is caused by another condition the patient may be suffering from, such as: ++Anemia++ due to iron deficiency. Cancer. Inflammation or infection, Surgery, especially splenectomy (removal of the spleen).
What is the blood cell that stops bleeding?
Platelets are blood cells in plasma that stop bleeding by sticking together to form a clot. Too many platelets can lead to certain conditions, such as stroke, heart attack or a clot in the blood vessels. Cancer Answer Line 866.223.8100. Appointments & Locations. Download a Treatment Guide.
What are the symptoms of a blood clot?
If you do have symptoms, they can include: Skin bruising. Bleeding from places like the nose, mouth and gums. Bleeding in the stomach or intestinal tract.. Abnormal blood clotting can also occur, leading to stroke, heart attack and unusual clots in the blood vessels of the abdomen.
Can thrombocytosis cause blood clotting?
Even though the platelet count is elevated for a short time (or even indefinitely after splenectomy), secondary thrombocytosis does not typically lead to abnormal blood clotting. Primary thrombocytosis, or essential thrombocythemia, can cause serious bleeding or clotting complications.
Is thrombocytosis an inherited disease?
It is also called essential thrombocythemia (or ET). The cause is unknown. It isn’t considered an inherited (genetic) condition even though certain gene mutations have been found in the blood or bone marrow.
Can you take aspirin for thrombocytosis?
Secondary forms of thrombocytosis rarely require treatment. For those with symptoms, a few treatment options are available. One is to treat the disease that is causing thrombocytosis. In some cases, you can take aspirin to help prevent blood clots.
Drugs Mentioned In This Article
Thrombotic disorders can be caused by genetic defects, which increase the risk of venous thromboembolism, or acquired defects, which increase the risk of arterial and venous thrombosis. Of the acquired causes, which of the following is most likely to increase a patient’s risk of venous thrombosis?
Merck and the Merck Manuals
Merck & Co., Inc., Kenilworth, NJ, USA is a global healthcare leader working to help the world be well. From developing new therapies that treat and prevent disease to helping people in need, we are committed to improving health and well-being around the world. The Merck Manual was first published in 1899 as a service to the community.
Introduction
Reactive thrombocytosis (RT), also known as secondary thrombocytosis, is a proliferation of platelets caused by a response to growth factors released from an inflammatory or malignant condition, whereas primary thrombocytosis (PT) is caused by an underlying myeloproliferative or myelodysplastic neoplasm. 9
A Common Clinical Finding
Thrombocytosis is a common incidental clinical finding, present in 1.5% to 2.2% of the population older than age 40 who are in a primary care setting. 4 The incidence of PT (also known as essential thrombocythemia), by comparison, is relatively low, at 1-2.5/100,000 per year.
RT: Diagnosis of Exclusion
Given the prevalence of RT in clinical practice (and therefore in underwriting), it is important to understand how it is diagnosed. Several factors point toward a reactive etiology rather than a primary cause.
Clinical Setting Determines Risk
RT is typically a clinically silent and transient condition. No clear correlation exists between symptoms and platelet counts; even patients with platelet counts of >1 million/microL due to RT are usually asymptomatic. 9
RT as a Predictor of Poor Outcomes
The presence of RT in infections and cancer may also be predictive of poor outcomes. In a recent study of 421 patients admitted for acute infectious disease, 32 had thrombocytosis with mean peak platelet counts of 527,000/microL.
Thrombocytosis and COVID-19
non-severe disease. 7 This validation of PLR as a prognostic marker in cardiac conditions, tumors, sepsis, pneumonia, and acute respiratory distress syndrome, suggests that RT might also be used as an independent prognostic marker of disease severity in COVID-19.
Underwriting Considerations
Given what we know about RT, there are several considerations when underwriting thrombocytosis, particularly in light of the ongoing COVID-19 pandemic.
Thrombocytosis care at Mayo Clinic
Mayo Clinic has experts in hematology experienced in diagnosing thrombocytosis. Mayo Clinic doctors are highly skilled at differentiating between essential thrombocythemia and reactive thrombocytosis.
Expertise and rankings
Mayo Clinic doctors see thousands of people with thrombocytosis every year.
Locations, travel and lodging
Mayo Clinic has major campuses in Phoenix and Scottsdale, Arizona; Jacksonville, Florida; and Rochester, Minnesota. The Mayo Clinic Health System has dozens of locations in several states.
Costs and insurance
Mayo Clinic works with hundreds of insurance companies and is an in-network provider for millions of people.
Reactive (Secondary) Thrombocytosis
By far the most common cause of thrombocytosis in general medical populations is a reactive, or secondary, process. The degree of elevation in the platelet count does not clearly differentiate clonal from reactive thrombocytosis.
Familial Thrombocytosis
Rare cases of familial thrombocytosis were initially described as an autosomal dominant disorder in which gain-of-function mutations in the thrombopoietin gene lead to overproduction of thrombopoietin and marked elevation of its plasma levels.
Clonal Thrombocytosis
Essential thrombocythemia is one of the chronic myeloproliferative disorders, a group of related disorders of the hematopoietic stem cells. Other myeloproliferative disorders include polycythemia vera, chronic myelogenous leukemia, and myeloid metaplasia with or without myelofibrosis.
Differential Diagnosis
There are presently no diagnostic findings that can definitively distinguish between clonal and secondary (reactive) thrombocytosis ( Table 2 ). As discussed above, patients with secondary thrombocytosis typically have clinically apparent, coexisting, underlying systemic diseases that account for the elevated platelet count.
Conclusions
Differentiating clonal from secondary causes of thrombocytosis can be extremely difficult, yet the distinction has important therapeutic implications. Secondary thrombocytosis per se does not result in vascular or hemostatic problems, but its underlying cause must be identified and treated, if possible.
Author Affiliations
From the Department of Medicine, University of Pennsylvania School of Medicine and University of Pennsylvania Health System, Philadelphia.
References (47)
1. Kaushansky K. Regulation of megakaryopoiesis. In: Loscalzo J, Schafer AI, eds. Thrombosis and hemorrhage. 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2003:120-39.