What is pheresis used to remove?
May 06, 2022 · Phone. (516) 321-7455. Reach out to a lipid specialist. Request an appointment. Dr. Hirsh placed Ms. Mohip on five different medications, all to no avail. “Despite all of these medications, her LDL (bad cholesterol) remained in the 190s and our goal was to bring it down to under 70,” he continued. “It was clear that she was a perfect ...
Who will perform pheresis on my child?
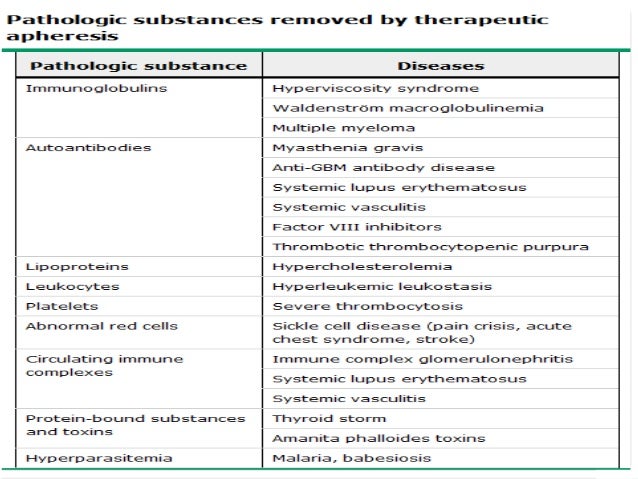
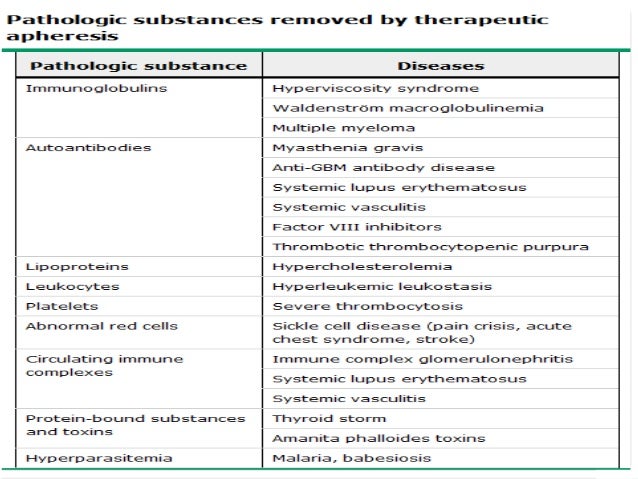
Pheresis is a treatment done to remove a harmful substance that is causing swelling in one or more of your child’s organs. It may also remove a “bad” substance (s) causing the body to work incorrectly. Pheresis is used to remove: Excess white blood cells, as in leukemia. Misshapen red blood cells, as in sickle cell disease. Extra red ...
How often does apheresis need to be done?
Oct 28, 2019 · Though most apheresis treatments are scheduled during the day, Yale Medicine’s center is open 24 hours a day, 7 days a week, in case of emergency. “Our staff is dedicated to ensuring patient safety, patient comfort and appropriate medical care,” says Dr. Snyder. “We are there for our patients around the clock.”.
What is apheresis therapy?
Overall, evidence in the literature suggests that the frequency of reactions to apheresis donation is less than that seen in whole blood donation.[1,2,6] The most common apheresis-specific reaction is hypocalcaemia due to citrate anticoagulation, which, while usually mild, has the potential for severely injuring the donor. Other reactions to ...
How many times can the patient treat with plasmapheresis?
What are the risks of plasmapheresis?
Does plasmapheresis affect immune system?
What conditions benefit from plasmapheresis?
How do you feel after plasmapheresis?
How long do plasmapheresis side effects last?
Does plasmapheresis remove good antibodies?
How much does it cost to have plasmapheresis?
Can plasma cure autoimmune disease?
What are side effects of plasma exchange?
Why you should not donate plasma?
What is a phenesis?
Pheresis is a treatment done to remove a harmful substance that is causing swelling in one or more of your child’s organs. Pheresis is used to remove: These disorders may cause organ dysfunction or pain in your child. Pheresis is done to help treat these problems.
How to prevent infection in children?
Help prevent infection by always washing your hands before entering your child’s room and before you leave. Check to make sure everyone does the same. Don’t be afraid to remind anyone who comes into your child’s room to wash their hands. Your child will need to rest quietly during this treatment.
How does apheresis work?
Sometimes, to treat an illness, one of those components may need to be removed or replaced through a process called apheresis. Apheresis uses a centrifuge that separates blood into its components by density. At Yale Medicine’s Transfusion Medicine Service, a team of experts works with more than 1,000 patients a year to provide safe ...
What is donor apheresis?
In donor apheresis, a healthy person donates blood using the apheresis machine, which is programmed to collect the desired blood component – either red blood cells, white blood cells, platelets, or plasma. The component can be stored and distributed to hospitals, to be given to a patient in need. The apheresis collections are drawn ...
What happens when you have too many white blood cells?
Leukemia. Patients with leukemia may have too many white blood cells, which can cause the blood to thicken and interfere with organ function. In the leukapheresis process, abnormal white blood cells are removed, and the rest of the blood is returned to the patient. Myasthenia gravis.
What is the treatment for thrombocytopenic purpura?
The most effective treatment is plasmapheresis, followed by replacement with normal donor plasma, which contains the needed enzyme.
Why do platelets clump?
This rare blood disorder causes platelet clumps to form throughout the body due to a lack of a needed blood enzyme. The most effective treatment is plasmapheresis, followed by replacement with normal donor plasma, which contains the needed enzyme.
What are the components of blood?
Human blood is made up of four components: red blood cells, white blood cells, platelets, and plasma. Sometimes, to treat an illness, one of those components may need to be removed or replaced through a process called apheresis. Apheresis uses a centrifuge that separates blood into its components by density.
Does plasmapheresis reduce immunity?
Plasmapheresis can reduce immunity to disease. This is usually temporary. However, for a time, the donor may become ill more easily. Wash the hands frequently and avoid being around anyone who is unwell.
What is plasmapheresis?
Plasmapheresis is a medical procedure designed to remove some plasma from the blood. During a plasma exchange, unhealthy plasma is swapped for healthy plasma or a plasma substitute, before the blood is returned to the body. The blood vessels contain plasma. It is a fluid made up of blood cells, platelets, and essential nutrients.
How to separate blood?
There are two ways to separate the components of blood: 1 Centrifugation. This process spins the blood, which divides it according to the density of the parts. 2 Filtration. This involves passing the blood through a filter to separate plasma.
What are the benefits of plasma exchange?
A plasma exchange can help to treat a range of medical conditions, including: 1 Brain and nervous system conditions, such as acute Guillain–Barré syndrome. 2 Blood disorders, such as thrombotic thrombocytopenic purpura, a rare disorder that causes blood clots. 3 Some kidney conditions, such as Goodpasture syndrome, a disease that causes antibodies to attack the kidneys and lungs. 4 Hyperviscosity syndromes, including myeloma. These conditions cause the blood to thicken, which can lead to organ damage or a stroke.
What is the process of removing blood from the body?
Pheresis, or apheresis , describes any process that removes the blood, filters and retains elements of it, then returns the blood to the body. Platelets, red blood cells, white blood cells, or plasma may be separated. The procedure is performed using a machine that removes small amounts of blood at a time. There are two ways to separate the ...
How long does plasma exchange take?
Plasma exchange takes between 2 and 4 hours. A person will need to remain as still as possible to help the blood to flow smoothly. It may help to watch television or read as a distraction. A medical professional will be present and check for side effects throughout the process.
Can you stay in the hospital overnight?
Recovery is usually quick, and a person is unlikely to stay overnight in a hospital. However, they may feel tired. Get plenty of rest and avoid driving or exercise. If a person feels unwell or experiences bleeding after leaving the hospital, they should contact a doctor. Last medically reviewed on April 10, 2018.
Who performs leukapheresis?
Leukapheresis can be performed by a blood specialist known as a hematologist or a qualified medical technologist, nurse, or doctor certified in apheresis. Certification is offered by the American Society for Apheresis (AFSA) in conjunction with the American Society for Clinical Pathology (ASCP). 11
How long does it take to get back on your feet after leukapheresis?
It is not uncommon to feel tired after leukapheresis. 7 To get back on your feet faster, limit your activities for the 12 to 24 hours. If you have an IV drip placed in your arm, keep the bandages dry and in place for at least five to six hours.
How is leukapheresis performed?
Leukapheresis is performed in one of two ways: 8 1 Continuous apheresis involves the removal of blood through one venipuncture site and the return of blood through a separate venipuncture site. This is the most common form of apheresis. 2 Intermittent apheresis involves the removal of blood through a venipuncture site which, after spinning, is returned to the body all at once through the same venipuncture site.
What is leukapheresis used for?
Leukapheresis is often used to decrease very high white blood cell (WBC) counts such as can occur with chronic blood cancers like chronic lymphocytic leukemia (CLL). It can also be performed to obtain white blood cells for later transplant, such as to treat steep declines in WBC counts during cancer chemotherapy.
Can leukapheresis be used for granulocytopenia?
Leukapheresis may be used, albeit rarely, to treat people with severe granulocytopenia in people with systemic (whole-body) infections. Granulocytopenia is a condition characterized by low levels of white blood cells called granulocytes, including neutrophils, eosinophils, and basophils .
Can you drink coffee before leukapheresis?
Most doctors will recommend that you drink plenty of fluids several days in advance of a leukapheresis procedure. Caffeine should be avoided as it promotes urination and can reduce the relative pressure in the veins.
Who is James Myhre?
James Myhre is an American journalist and HIV educator. Doru Paul, MD, is board-certified in internal medicine, medical oncology, and hematology. Leukapheresis is a medical procedure in which white blood cells (leukocytes) involved in the body's immune response are separated from a sample of blood.
How to help people with encephalitis?
Connect with people. Social interaction can help manage stress and feelings of depression. It may also stimulate brain development. It is important for people to re-connect with their previous social roles. If friendship patterns change after encephalitis, it is important to consider new avenues for social involvement.
How to heal your brain?
Recovery isn’t always in a straight line, it can be backwards and forwards”. “Be patient, don't push yourself too hard too soon. Your brain needs time and rest to heal as best as it possibly can.
How long does it take to recover from encephalitis?
Recovery from encephalitis may take time. Initial recovery may be rapid but usually falls short of complete. Further recovery takes place more slowly over a period of months, even years. People are different. No two cases of encephalitis will have an identical outcome and people recover at different paces.
How does eating affect your brain?
Also, after a brain injury, the calories intake may increase and it is important to eat food rich in nutrients. Drink plenty of water and avoid alcohol, sugar, saturated fat products, salty food and too much caffeine.
What to say when you have a headache?
Stop and listen to me. Love, your wounded brain”.
What are the nutrients that affect the brain?
Deficiencies in the intake of some nutrients can impact brain functioning. Vitamins ( A, B, B1, B6, B12, E, acid folic) and minerals (iron, magnesium, selenium, zinc) that are important are found in products such as vegetables, fruits, grains, lean meats, poultry, fish, beans and pulses and dairy products.
What is the treatment for GVHD?
The treated white blood cells will then be re-infused into your body through your arm or CVC. The treated cells will help your immune system fight GVHD or CTCL. Another medication called heparin is used during the procedure to prevent your blood from clotting in the photopheresis machine. Back to top.
What is the treatment for white blood cells?
Your white blood cells are treated with a medication called methoxsalen, exposed to ultraviolet (UV) light, and then put back in your vein, along with your other blood cells.
What is the phone number for the Koch Apheresis Unit?
If you have any questions or concerns, call the Blood Donor Room at 212-639-6178 or the Koch Apheresis Unit at 646-608-3142. They can be reached Monday through Friday from 8:00 am to 6:00 pm. After 6:00 pm and on the weekends, call 212-639-2000.
Do you have to wear a mask at MSK?
Masks Are Still Required at MSK. Patients and visitors must continue to wear masks while at MSK, including people who are fully vaccinated. MSK is offering COVID-19 vaccines to all patients age 12 and over. To schedule or learn more, read this. For Adult Patients /.
Is plasmapheresis contraindicated for TTP?
Transfusion is contraindicated in thrombotic TTP, as it fuels the coagulopathy. Since the early 1990s, plasmapheresis has become the treatment of choice for TTP. This is an exchange transfusion involving removal of the person's blood plasma through apheresis and replacement with donor plasma ( fresh frozen plasma or cryosupernatant ); the procedure must be repeated daily to eliminate the inhibitor and abate the symptoms. If apheresis is not available, fresh frozen plasma can be infused, but the volume that can be given safely is limited due to the danger of fluid overload. Plasma infusion alone is not as beneficial as plasma exchange. Corticosteroids ( prednisone or prednisolone) are usually given. Rituximab, a monoclonal antibody aimed at the CD20 molecule on B lymphocytes, may be used on diagnosis; this is thought to kill the B cells and thereby reduce the production of the inhibitor. A stronger recommendation for rituximab exists where TTP does not respond to corticosteroids and plasmapheresis.
What is the cause of TTP?
TTP of unknown cause was long known as idiopathic TTP but in 1998 the majority of cases were shown to be caused by the inhibition of the enzyme ADAMTS13 by antibodies. The relationship of reduced ADAMTS13 to the pathogenesis of TTP is known as the Furlan-Tsai hypothesis, after the two independent groups of researchers who published their research in the same issue of the New England Journal of Medicine. These cases are now classed as an autoimmune disease and are known as autoimmune TTP (not to be confused with immune/idiopathic thrombocytopenic purpura ).
What are the factors that determine TTP?
Secondary TTP is diagnosed when the person's history mentions one of the known features associated with TTP. It comprises about 40% of all cases of TTP. Predisposing factors are: 1 Cancer 2 Bone marrow transplantation 3 Pregnancy 4 Medication use:#N#Antiviral drugs ( acyclovir)#N#Certain chemotherapy medications such as gemcitabine and mitomycin C#N#Quinine#N#Oxymorphone#N#Quetiapine#N#Bevacizumab#N#Sunitinib#N#Platelet aggregation inhibitors ( ticlopidine, clopidogrel, and prasugrel)#N#Immunosuppressants ( ciclosporin, mitomycin, tacrolimus /FK506, interferon-α)#N#Hormone altering drugs (estrogens, contraceptives, hormone replacement therapy) 5 HIV-1 infection
What is a TTP?
Thrombotic thrombocytopenic purpura ( TTP) is a blood disorder that results in blood clots forming in small blood vessels throughout the body. This results in a low platelet count, low red blood cells due to their breakdown, and often kidney, heart, and brain dysfunction. Symptoms may include large bruises, fever, weakness, shortness of breath, ...
What are the symptoms of a symtom?
Symptoms may include large bruises, fever, weakness, shortness of breath, confusion, and headache. Repeated episodes may occur. In about half of cases a trigger is identified, while in the remainder the cause remains unknown.
Is TTP inherited?
Less commonly TTP is inherited from a person's parents, known as Upshaw–Schulman syndrome, such that ADAMTS13 dysfunction is present from birth. Diagnosis is typically based on symptoms and blood tests. It may be supported by measuring activity of or antibodies against ADAMTS13.
How do you know if you have TTP?
The signs and symptoms of TTP may at first be subtle and nonspecific. Many people experience an influenza-like or diarrheal illness before developing TTP. Neurological symptoms are very common and vary greatly in severity. Frequently reported symptoms include feeling very tired, confusion, and headaches. Seizures and symptoms similar to those of a stroke can also be seen. Other symptoms include, but are not limited to jaundice or paleness of the skin, a fast heart rate or shortness of breath, or pinpoint-sized purple or reddish dots on the skin known as petechiae.
