The authors concluded that in routine clinical care of patients with NSTEMI, fondaparinux was associated with lower odds than LMWH of major bleeding events and death both in-hospital and up to 180 days afterward. Perspective:
Full Answer
Do patients with NSTEMI develop Pathological Q-waves?
Hence, patients with NSTEMI typically do not develop pathological Q-waves. However, in some instances the subendocardial injury may be extensive in patients with NSTEMI, which may result in pathological Q-waves.
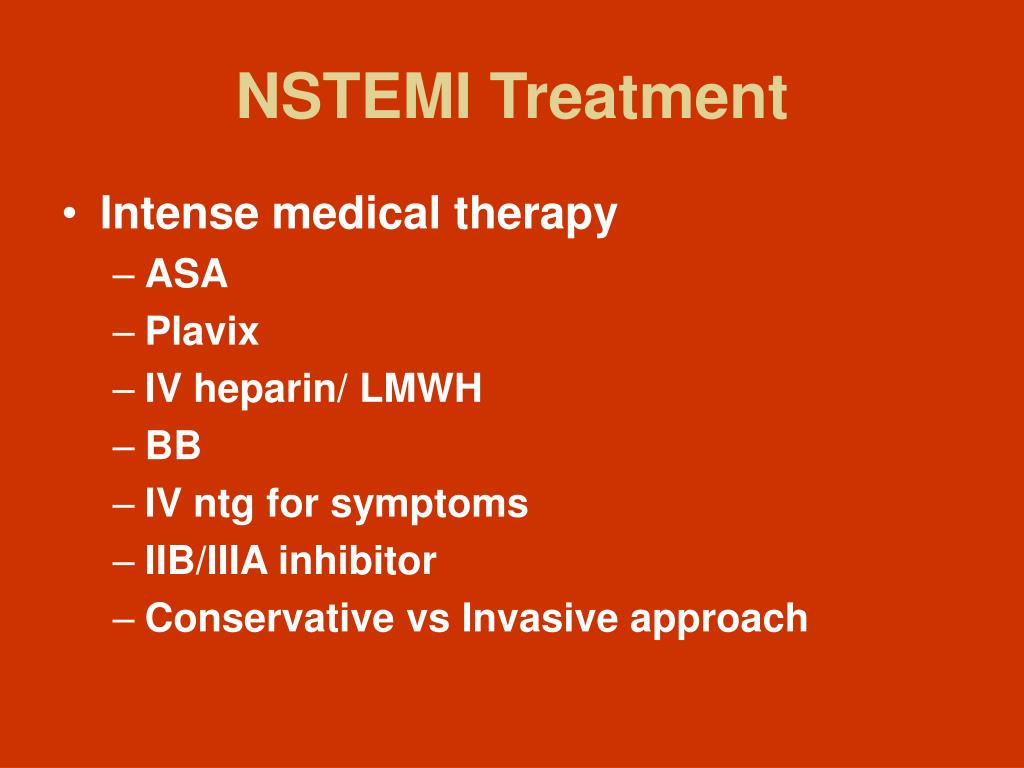
How is NSTEMI treated in unstable angina?
NSTEMI and unstable angina are treated with anti-ischemic (to alleviate ischemia) and anti-thrombotic (to counteract the thrombus) agents. Most patients undergo coronary angiography within 48 hours or earlier if the patient is at high risk of death or other complications.
Do the risks of thrombolysis outweigh the benefits of NSTEMI?
In comparison, the pathology is a fibrin-rich clot (red clot) in STEMI. Thrombolysis or fibrinolysis in NSTEMI may expose and release the underlying platelets into circulation likely leading to further fresh thrombii. Hence, risks of thrombolysis outweigh the benefits in that group of patients. 1 point for each risk factor (maximum score 7).
When should PCI be done after NSTEMI?
Guidelines do not recommend acute angiography in patients with NSTEMI or unstable angina. Guidelines recommend that PCI should be done within 24 hours of NSTEMI/unstable angina, if possible. Low-risk patients may be evaluated after 48–72 hours.

Which drug is contraindicated in NSTEMI?
Contraindications include the recent use of phosphodiesterase inhibitors and hypotension. Nitrates should be used with extreme caution in patients with concerns for right-sided infarction. Continuous intravenous nitroglycerin should be considered in patients with persistent signs of heart failure or hypertension.
Do you give heparin for NSTEMI?
The ACC/AHA Guidelines4 state that patients with NSTEMI should receive heparin, unless contraindicated. Although the optimal duration of heparin therapy is not well established, most trials of UFH involving UA/NSTEMI patients recommend continuing heparin therapy for 2 to 5 days.
Can Lovenox be used for NSTEMI?
Proven outcomes in UA/NSTEMI and STEMI Lovenox significantly reduced the incidence of the combined endpoint of death, MI, or recurrent angina versus unfractionated heparin (UFH) in UA/NSTEMI patients when administered concomitantly with aspirin.
What does heparin do in NSTEMI?
For NSTEMI patients treated with an invasive strategy, heparin makes sense as a temporary bridge to definitive revascularization with stenting or CABG surgery.
Why anticoagulants are used in NSTEMI?
Antiplatelet therapy initiated during a hospitalization for UA/NSTEMI and continued for long-term management has been shown to reduce future cardiovascular events. Anticoagulant medications work by inhibiting blood clotting, either by antagonizing the effects of vitamin K or by blocking/inhibiting thrombin.
Does heparin help in MI?
The roles of heparin and warfarin in reducing morbidity and mortality after acute myocardial infarction (AMI) are reviewed. Full-dose i.v. heparin, with or without thrombolytic therapy, is indicated for the prevention of reinfarction and thromboembolism after AMI.
How is a Nstemi treated?
Drug treatment is used for those who are low risk who've had an NSTEMI. Medications that may be given include anticoagulants, antiplatelets, beta-blockers, nitrates, statins, angiotensin-converting-enzyme (ACE) inhibitors, or angiotensin receptor blockers (ARBs).
Why enoxaparin is given in unstable angina?
Discussion. The results of TIMI 11B indicate that for the acute management of unstable angina/non–Q-wave MI patients, enoxaparin is superior to unfractionated heparin for reducing a composite of death and serious cardiac ischemic events.
When do you start heparin for elevated troponin?
If a patient has a very symptomatic UA/nSTEMI, and does not have other major bleeding risk factors, then I will consider starting a heparin drip in conjunction with my admitting team and consultants if prompt cardiac catheterization is not possible. However, in general, the risks seem to outweigh the benefits.
What are the contraindications of heparin?
Absolute contraindications to heparin include known hypersensitivity, past or present heparin-induced thrombocytopenia and active bleeding. Caution is required when prescribing heparin to patients with conditions that may increase the risk of bleeding (see box).
Does heparin affect troponin?
Objectives: Heparin is thought to play a crucial role in the clinical monitoring of patients with acute coronary syndrome as well as after coronary bypass surgery in that it interferes with different commercial immunoassay test systems for cardiac troponin T (cTnT) and troponin I (cTnI).
Why is heparin used in ACS?
The goal of heparin therapy in acute coronary syndromes is to retard the progression of intracoronary thrombus and thus prevent myocardial infarction and death. The progression of this condition when a patient is on aspirin alone, provides some guide as to the duration of heparin therapy that would be beneficial.
How is a NSTEMI treated?
Drug treatment is used for those who are low risk who've had an NSTEMI. Medications that may be given include anticoagulants, antiplatelets, beta-blockers, nitrates, statins, angiotensin-converting-enzyme (ACE) inhibitors, or angiotensin receptor blockers (ARBs).
When is heparin used for ACS?
The goal of heparin therapy in acute coronary syndromes is to retard the progression of intracoronary thrombus and thus prevent myocardial infarction and death. The progression of this condition when a patient is on aspirin alone, provides some guide as to the duration of heparin therapy that would be beneficial.
What are the contraindications of heparin?
Absolute contraindications to heparin include known hypersensitivity, past or present heparin-induced thrombocytopenia and active bleeding. Caution is required when prescribing heparin to patients with conditions that may increase the risk of bleeding (see box).
Do you treat unstable angina with heparin?
Heparin has been advocated as additional therapy for unstable angina. The theoretic benefit of adding heparin is that it may prevent the propagation of an established thrombus, allowing time for endogenous fibrinolysis to occur.
How long after NSTEMI do you die from fondaparinux?
The authors concluded that in routine clinical care of patients with NSTEMI, fondaparinux was associated with lower odds than LMWH of major bleeding events and death both in-hospital and up to 180 days afterward.
Is fondaparinux a LMWH?
This study compared the anticoagulant fondaparinux with LMWH in a nationwide registry of patients with NSTEMI treated in routine clinical care. The study reports that the use of fondaparinux, compared with LMWH, was associated with a lower risk of bleeding events and death both in short- and long-term follow-up, but with similar rates of MI and stroke. The results support current American College of Cardiology/American Heart Association guidelines, which recommend that either fondaparinux or enoxaparin be used for patients with acute coronary syndrome who do not undergo percutaneous coronary intervention (PCI). It should be noted that fondaparinux was associated with a small, but significant increase in catheter-related thrombi (in patients undergoing PCI) compared to enoxaparin in the OASIS-5 trial. To avert catheter thrombosis when fondaparinux is used alone in patients undergoing PCI, an anticoagulant with anti-IIa activity also needs to be administered.
What is non ST elevation myocardial infarction?
Non-ST elevation myocardial infarction (NSTEMI) is a recognized diagnostic entity that has an unacceptable mortality rate when it goes unrecognized. Following diagnosis, initial treatment with analgesics, nitrates and anti-platelet agents forms the initial approach. New anti-platelet agents such as ticagrelor and prasugrel need to be clearly understood. Simultaneously, risk stratification for ischaemia and bleeding of each such patient into mild, moderate and severe helps determine the course of further treatment that will be provided to the patient. The major decision is the need for and timing of early coronary angiography to determine the anatomy of the culprit vasculature and the decision for coronary revascularization, either by the percutaneous approach or coronary artery bypass grafting. It is at this stage that the need for and type of anticoagulation will require decision making. Choices include fondaparinux, the heparins, bivalirudin and inhibitors of the coagulation cascade.
What is the primary mechanism for occurrence of symptoms?
The primary mechanism for occurrence of symptoms is coronary artery blockage. Various grades of patients constitute the spectrum that is NSTEMI. Those with low risk benefit from conservative management, while those at high risk may require an invasive approach. Whichever is taken would depend on the patient’s clinical condition, presence of co-morbidities and risk factors, severity of lesions seen on coronary angiography, and a clear understanding of the risks and benefits of invasive versus conservative strategies.
What is risk level determination?
Risk-level determination allows one to offer advice regarding a variety of treatment procedures, viz. need for a variety of anti-platelet agents, glycoprotein IIb/IIIa inhibitors (GP23I) and anticoagulants, and allow rational discussion of a choice of early invasive versus conservative management. Figure 1 below outlines a schema for such decision making.
What are the symptoms of atypical symptons?
Atypical symptoms include epigastric discomfort, sharp chest pains, or increasing breathlessness and are more common in older patients (≥75 years age), women, diabetic patients, and those with uraemia or functional decline. Atypical symptoms can lead to under-diagnosis, hence requiring a high index of suspicion.
What is CAD in medical terms?
Coronary artery disease (CAD), by far the commonest variety of cardiovascular disease, includes a spectrum of conditions ranging from silent angina, stable and unstable angina pectoris, acute myocardial infarction, heart failure and sudden death. The first four of these are referred to as “acute coronary syndromes” (ACS).
Does clopidogrel inhibit ADP?
Clopidogrel, a pro-drug activated in the liver by the CYP2C19 isoenzyme of cytochrome P450, irreversibly inhibits the P2Y 12 subtype of ADP receptor and also blocks activation of the glycoprotein IIb/IIIa pathway. Platelet inhibition is evident 2 h after a single dose of oral clopidogrel. Patients with a variant allele for the CYP2C19 isoenzyme have lower levels of active metabolite and are 1.5–3.5 times more likely to die or have complications than those with the high-functioning allele [ 43 – 45 ]. Poor metabolizers apparently make up to about 14 % of the patients and are at high risk of treatment failure. The Food and Drug Administration (FDA) [ 46] has placed a warning on clopidogrel to make doctors and patients aware of this.
Does ischaemia cause pain?
Relief of Ischaemic Pain. Pain relief is one of the most pressing needs of the patient. In acute coronary ischaemia, the increased heart rate, higher blood pressure or high preload result in decreased myocardial oxygen supply and increased myocardial oxygen demand. This oxygen imbalance results in ischaemic pain.
What causes NSTEMI and unstable angina?
This is explained by the fact that NSTEMI and unstable angina are caused by partial (incomplete) coronary artery occlusions; a partial occlusion results in a reduction of coronary blood flow and this causes subendocardial ischemia (i.e ischemia that only affects the subendocardium).
How is unstable angina different from NSTEMI?
NSTEMI and unstable angina are different in one fundamental aspect: NSTEMI is by definition an acute myocardial infarction, whereas unstable angina is not an infarction. Unstable angina is only diagnosed if there are no evidence of myocardial infarction (necrosis). However, unstable angina is considered an acute coronary syndrome because it is an imminent precursor to myocardial infarction. Approximately 50% of patients with unstable angina progress to myocardial infarction within 30 days if left untreated. Moreover, the pathophysiology of NSTEMI and unstable angina is very similar: both are due to partial (incomplete) coronary artery occlusions, which implies that there remains residual blood flow in the artery. Moreover, management of NSTEMI and unstable angina is virtually equal and this explains why NSTEMI and unstable angina have traditionally been grouped together.
What is pathological Q wave?
Pathological (infarction) Q-waves. Pathological Q-waves arise arise if the infarction is extensive, which is usually not the case in patients with NSTEMI. Hence, patients with NSTEMI typically do not develop pathological Q-waves.
How long should beta blockers be given?
Oral beta blockers should be given to all patients in maximal tolerated dose and continued indefinitely. Therapy should be initiated within 24 hours. Intravenous beta blockers is potentially harmful in patients with NSTEMI or unstable angina.
What is the oxygen saturation level?
Oxygen is given if oxygen saturation is <90%. There is no evidence that oxygen confers any benefit. There is no data to support or refute any benefit of oxygen in patients with NSTEMI or unstable angina. Guidelines recommend oxygen if oxygen saturation is <90%.
How effective is aspirin for NSTEMI?
Aspirin has an astonishing effect in NSTEMI and unstable angina: it reduces 30-days mortality by 50%. Aspirin is also effective in preventing re-infarction beyond 30-days and must never be discontinued without careful consideration. The optimal dose of aspirin is unknown but studies show that maintenance doses between 80 mg and 1500 mg are equally effective; hence, 80 mg is preferred as it minimizes the risk of gastrointestinal bleedings. Similarly, loading doses greater than 320 mg do not confer any additional benefit, which is why a loading dose of 320 mg is recommended.
What is ACS in medical terms?
The term acute coronary syndrome (ACS) has been discussed previously (refer to Introduction to Ischemic Heart Disease and Classification of Acute Coronary Syndromes ). An acute coronary syndrome is caused by an abrupt reduction in coronary blood flow. The reduction in coronary blood flow is due to atherothrombosis, which occurs when an atherosclerotic lesion disrupts. Atherotrombosis obstructs coronary blood flow and causes ischemia in the myocardium supplied by the artery. Figure 1 shows the process from atherothrombosis to classification of acute coronary syndromes.
Is enoxaparin better than UFH?
Enoxaparin has been proven to be at least non-inferior and likely even superior to UFH when it comes to reducing the risk of death and MI in the setting of NSTEMI.
Is enoxaparin a superior treatment for NSTEMI?
It may seem that as treatment of NSTEMI has evolved to include antiplatelet therapy and early invasive intervention, the superiority of enoxaparin has been negated. However, both the SYNERGY and A to Z trials were potentially confounded by the fact that a majority of patients received pre-randomization therapy.
Which study used heparin followed by warfarin?
Cohen 1994 used heparin followed by warfarin throughout the entire study period. These authors didn't observe a sharp rebound in event rates because they continued anticoagulation throughout the entire study. Gurfinkel 1995 found a benefit of low molecular-weight heparin, but not unfractionated heparin.
Is heparin a noninvasive treatment?
However, there is no evidence to support the use of heparin for a patient who is being treated with a noninvasive approach. Heparin causes a short-term reduction in events, but there is a rebound in ischemic events after it is discontinued.
Does heparin help with reinfarction?
Ultimately, short-term treatment with heparin delays reinfarction without having any sustained benefit. Clinical trials which fail to follow patients after discontinuation of anticoagulation incorrectly conclude that heparin is beneficial. This has previously been discussed by David Newman and on this blog. 0.
Does heparin help with non ST elevation?
The use of heparin for noninvasive management of non-ST elevation MI (NSTEMI) is one of the most deeply entrenched myths of modern medicine. Although heparin reduces reinfarction, when it is discontinued there is a rebound in infarction rates. Ultimately, short-term treatment with heparin delays reinfarction without having any sustained benefit.
Is heparin a transient drug?
0. The authors of this article recognized that the effects of heparin are transient, stating: Because the anticoagulant effects of heparin are brief, any benefit of therapy is unlikely to last beyond the duration of treatment.
Is heparin an IV?
Heparin was administered as an intermittent IV bolus rather than as an infusion. The primary outcome was a composite of MI and death. Compared to aspirin alone, there was no statistically significant advantage to the combination of aspirin plus heparin at any time-point.
