
Nephrotic Syndrome
Excreting too much protein in urine due to a kidney disorder.
What is the best treatment for nephrotic syndrome?
The use of steroids in idiopathic nephrotic syndrome is the major discovery of the twentieth century in the field of pediatric nephrology. At onset of the twenty-first century, steroids remain the first line of treatment at first flare. All the protocols to treat the first flare are similar by a common sequence including a first phase of daily prednisolone/prednisone at a dose of 60 …
What is the prognosis of steroid-resistant nephrotic syndrome?
Mar 18, 2015 · Nephrotic syndrome is a condition where the kidneys leak protein from the blood into the urine. When it is untreated, children can often die from infections. Most children, with nephrotic syndrome, respond to corticosteroid drugs (prednisone, prednisolone) reducing the risk of serious infection.
How dangerous is nephrotic syndrome?
treatment hasgenerally been directed towardsrelievingthe most prominent symptom, the oedema, either by the infusion of plasma-volume expanders, such as concentrated human serum albumin, or by promoting the loss of salt and water from the bodybythe useof diuretics, low-salt diets, andexchangeresins.
Is chemo treatment effective for nephrotic syndrome?
Treatment with CsA or tacrolimus is recommended for patients who continue to show steroid dependence or frequent relapses despite treatment with the above medications. 12 Either of these agents is effective in maintaining remission in most patients with steroid-sensitive nephrotic syndrome. The chief concern with their use is nephrotoxicity, but with careful …
How do corticosteroids treat nephrotic syndrome?
In nephrotic syndrome protein leaks from the blood to the urine through the glomeruli resulting in hypoproteinaemia and generalised oedema. While most children with nephrotic syndrome respond to corticosteroids, 80% experience a relapsing course. Corticosteroids have reduced the mortality rate to around 3%.Mar 18, 2015
Can steroids cure nephrotic syndrome?
Corticosteroids (prednisone), cyclophosphamide, and cyclosporine are used to induce remission in nephrotic syndrome. Diuretics are used to reduce edema.Nov 23, 2021
How does prednisone work in nephrotic syndrome?
Steroid drugs, such as prednisone, work by lowering the activity of the immune system. The immune system is your body's defense system. Steroids work by slowing your body's response to disease or injury. Prednisone can help lower certain immune-related symptoms, including inflammation and swelling.Sep 23, 2015
How do steroids reduce proteinuria?
Steroids probably have the capability of reducing proliferative lesions in the acute phase of IgAN and consequently proteinuria. This possibly limits the development of glomerular and tubular sclerosis later on.
How long do you take steroids for nephrotic syndrome?
On the basis of current evidence and opinion, the Group recommends that the initial episode of nephrotic syndrome be treated with prednisolone at a dose of 2 mg/kg per day (maximum 60 mg in single or divided doses) for 6 weeks, followed by 1.5 mg/kg (maximum 40 mg) as a single morning dose on alternate days for the ...
What causes steroid dependent nephrotic syndrome?
Mutations in the NPHS2 gene, which encodes podocin, can cause a recessive form of SRNS. Mutations in this gene occur in ~40% of familial and 6%–17% of sporadic SRNS cases. Patients typically present from birth to 6 years of age have a steroid-resistant course and reach ESRD before the end of their first decade.Apr 11, 2017
What is the purpose of taking prednisone?
Prednisone is used to treat conditions such as arthritis, blood disorders, breathing problems, severe allergies, skin diseases, cancer, eye problems, and immune system disorders.
What are steroids prescribed for?
Corticosteroid drugs are used to treat rheumatoid arthritis, inflammatory bowel disease (IBD), asthma, allergies and many other conditions. These drugs also help suppress the immune system in order to prevent organ rejection in transplant recipients.
How do steroids work?
How do steroids work? Steroids work by decreasing inflammation and reducing the activity of the immune system. Inflammation is a process in which the body's white blood cells and chemicals can protect against infection and foreign substances such as bacteria and viruses.Jan 20, 2020
Why do steroids cause proteinuria?
protein reabsorption. This suggests that prednisolone increases proteinuria by causing a change in glomerular permselectivity.
Can steroids affect GFR?
We conclude that GFR rises during 2 weeks of high-dose prednisone administration, a rise that is not reflected by a decrease in plasma creatinine concentration. On the contrary, both plasma creatinine concentration and urinary creatinine excretion increase, probably as a result of the catabolic effect of prednisone.Sep 18, 1992
Do steroids increase protein in urine?
The investigators studied a group of 10 bodybuilders who took anabolic steroids for years. All developed protein leakage into the urine and severe reductions in kidney function.Dec 10, 2009
How to help nephrotic syndrome?
Your doctor might refer you to a dietitian, who might recommend that you do the following: Choose lean sources of protein. Plant-based protein is helpful in kidney disease. Reduce the amount of fat and cholesterol in your diet to help control your blood cholesterol levels.
What are the best medications for nephrotic syndrome?
Medications include rituximab (Rituxan), cyclosporine and cyclophosphamide.
What to ask when making an appointment for nephrotic syndrome?
What you can do. When you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet. Take a family member or friend along, if possible, to help you remember the information you'll be given. For nephrotic syndrome, some questions to ask include:
What is the best medicine for blood clots?
These might be prescribed to decrease your blood's ability to clot, especially if you've had a blood clot. Anticoagulants include heparin, warfarin (Cou madin, Jantoven), dabiga tran (Pradaxa), apixaban (Eliquis) and rivaroxaban (Xarelto). Immune system-suppressing medications.
What is the name of the drug that reduces blood pressure?
Blood pressure medications. Drugs called angiotensin-converting enzyme (ACE) inhibitors reduce blood pressure and the amount of protein released in urine. Medications in this category include lisinopril (Prinvil, Qbrelis, Zestril), benazepril (Lotensin), captopril and enalapril (Vasotec). Another group of drugs that works similarly is called ...
How to reduce swelling in the blood?
Reduce the amount of fat and cholesterol in your diet to help control your blood cholesterol levels. Eat a low-salt diet to help control swelling. Reduce the amount of liquid in your diet.
Can statins lower cholesterol?
Statins can help lower cholesterol levels. However, it's not clear whether cholesterol-lowering medications can improve the outcomes for people with nephrotic syndrome, such as avoiding heart attacks or decreasing the risk of early death. Statins include atorvastatin (Lipitor), fluvastatin (Lescol XL), lovastatin (Altoprev), ...
What is the problem with nephrotic syndrome?
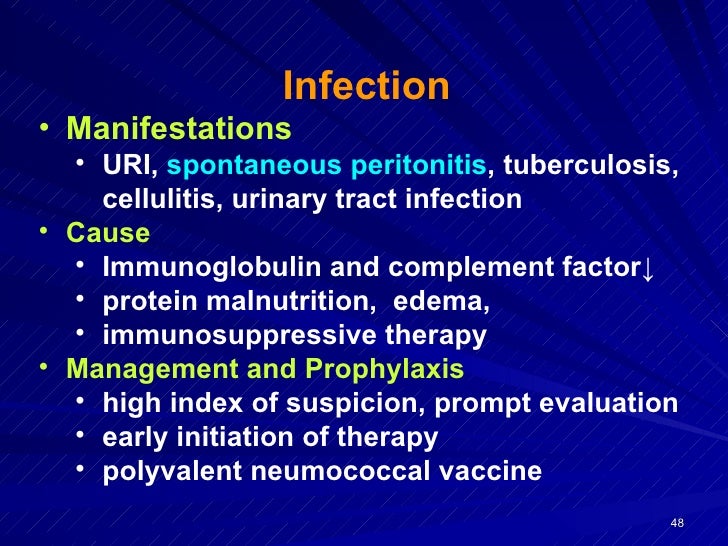
What is the issue? Nephrotic syndrome is a condition where the kidneys leak protein from the blood into the urine. When untreated, children can suffer from serious infections. In most children with nephrotic syndrome, this protein leak resolves with corticosteroid drugs (prednisone, prednisolone) reducing the risk of serious infection.
How does nephrotic syndrome affect the body?
In nephrotic syndrome protein leaks from blood into the urine through the glomeruli resulting in hypoproteinaemia and generalised oedema. While most children with nephrotic syndrome respond to corticosteroids, 80% experience a relapsing course. Corticosteroids have reduced the death rate to around 3%. However, corticosteroids have well recognised ...
How long does prednisone last in SSNS?
There are now four well designed studies randomising 823 children which have clearly demonstrated that there is no benefit of prolonging prednisone therapy beyond two to three months in the first episode of SSNS. Small studies in children with relapsing disease have identified no differences in the times to remission using half the conventional induction dose of 2 mg/kg or 60 mg/m 2. It is imperative that a much larger study be carried out to confirm these findings.
How long does it take for prednisone to work for nephrotic syndrome?
Children with their first episode of nephrotic syndrome only need two or three months of prednisone since longer courses do not reduce the risk of relapse or reduce the risk that the child will relapse frequently. We need more information to determine whether giving daily prednisone during an infection reduces the risk of relapse.
How long does it take for a child to relapse from prednisone?
What did we find? In high quality studies, there was no difference in the risk of relapse or in the number of children who relapse frequently between long duration (three to seven months) and shorter durations (two to three months) of prednisone (high certainty evidence).
How much do corticosteroids reduce the death rate?
Corticosteroids have reduced the death rate to around 3% . However, corticosteroids have well recognised potentially serious adverse effects such as obesity, poor growth, hypertension, diabetes mellitus, osteoporosis, and behavioural disturbances.
Can you give a child prednisone?
Giving daily rather than alternate-day prednisone during a viral infection may reduce the number of children who relapse with infection. Two very small studies suggested that lower doses of prednisone can be used to achieve and maintain remission.
What is the first step in nephrotic syndrome?
In patients with swelling the first step is to establish a diagnosis of nephrotic syndrome. Laboratory tests should confirm (1) heavy loss of protein in the urine, (2) low blood protein levels, and (3) high cholesterol levels.
What is the most common cause of nephrotic syndrome in children?
The most common cause of nephrotic syndrome in children is minimal change disease (MCD). This disease occurs in 90 percent of cases of idiopathic nephrotic syndrome in young children (under age six) and in 65% of cases in older children.
How long does nephrotic syndrome last?
Treatment of this disease usually lasts for a long period (years).
What are the effects of steroids on the face?
Two independent effects of steroids are increased appetite leading to weight gain and redistribution of fat. These lead to a round or swollen face. Steroid induced moon-shaped face is seen during the third or fourth week of steroid therapy, which mimics swelling of the face due to nephrotic syndrome.
How rare is idiopathic nephrotic syndrome?
Idiopathic nephrotic syndrome is a rare disease that occurs in two to seven cases per 100,000 children per year and has a prevalence of approximately 16 cases per 100,000 [ 1 ]. The disease is characterized by leakage of a large amount of proteins through the glomerular filter, leading to hypoalbuminemia, hyperlipidemia, decreased oncotic pressure, and edema. In overt forms, proteinuria exceeds 50 mg/kg/day or 40 mg/m 2 /h, and the urine protein/creatinine ratio is > 2 mg/mg.
What is SSNS in pediatrics?
Steroid-sensitive nephrotic syndrome (SSNS) is a rare condition that develops primarily in preadolescent children after the age of 1 year. Since the 1950s, oral corticosteroids have been the mainstay of treatment of all children presenting with nephrotic syndrome, with most patients responding within 4 weeks to an oral course of prednisone (PDN). However, corticosteroids have important side effects and 60–80 % of patients relapse, developing frequently relapsing or steroid-dependent forms. For these reasons, many patients require second-line steroid-sparing immunosuppressive medications that have considerably improved relapse-free survival, while avoiding many PDN-related toxicities. Since most patients will eventually heal from their disease with a normal kidney function, the morbidity of SSNS is primarily related to side effects of drugs that are used to maintain prolonged remission. Therefore, treatment is essentially based on balancing the use of different drugs to achieve permanent remission with the lowest cumulative number of side effects. Treatment choice is based on the severity of SSNS, on patient age, and on drug tolerability. This review provides an update of currently available therapeutic strategies for SSNS.
What is levamisole used for?
Historically, levamisole has been used to treat infestations, colon cancer, leprosy, and a variety of dermatologic conditions, including skin infections, lichen planus, warts, recurrent oral aphthous ulcers, and Behçet syndrome, in addition to nephrotic syndrome [ 37, 38 ]. Since it was found to be inefficient in many of these conditions, in particular in solid tumors, it is no longer produced in most western countries, but is often used to adulterate cocaine [ 37 ]. Several retrospective reports have suggested efficacy of levamisole in reducing the frequency of relapses of SSNS [ 37 ]. In a systematic Cochrane review, the risk of relapse of NS was calculated to be halved with levamisole treatment for four to 12 months [ 39 ]. In nearly all studies, levamisole has been prescribed on alternate days or in two weekly doses on consecutive days [ 38 ]. The usual dose is 2.0–2.5 mg/kg [ 38 ]. However, these results have not been confirmed in adequately powered randomized studies for many years. Recently, a double blind randomized controlled study including patients with FRNS or SDNS showed more sustained remission at 1 year in children receiving levamisole, compared to placebo (26% vs. 6%) [ 40 ]. A post hoc analysis found significant differences in the response to levamisole between European and Indian children that were most likely related to differences in the severity of SSNS [ 40 ]. Specifically, European patients relapsed more frequently but had SDNS more often (89%), compared to Indian patients (42%) [ 40 ]. Although underpowered, this analysis suggests that levamisole should be prescribed primarily to children with FRNS, as also suggested in other reports [ 41 ]. A second randomized controlled study has compared mycophenolate mofetil (MMF) (750–1000 mg/m 2 /day) with levamisole (2–2.5 mg/kg/alternate days) in 149 Indian children [ 42 ]. Patients had FRNS or SDNS, and PDN was tapered in two to three months [ 42 ]. Therapy with MMF was not found to be superior to levamisole in inducing sustained remission and in reaching a composite outcome that included relapse frequency, treatment failure, and steroid toxicity [ 42 ]. Notably, however, the dose of MMF that was prescribed in this trial was relatively low, which may have significantly influenced results [see below].
Do corticosteroids cause SSNS?
Since 1950, oral corticosteroids have been the mainstay of the treatment of children presenting with SSNS [ 9, 10 ]. However, corticosteroids have well-known side effects, all of which have been reported in SSNS, including obesity, hypertension, osteoporosis, stunted linear growth, adrenal suppression, cushingoid features, striae rubrae, glaucoma, cataract, diabetes mellitus, and psychiatric disorders. In the past, these adverse events were very frequent in patients with FRNS/SDNS. For example, we observed in a group of patients treated in the 1980s and 1990s an average loss of 0.9 ± 0.8 SD in linear growth after a mean follow up of 12 years, correlating with the cumulative dose of PDN [ 11 ]. These side effects are now rarely observed with the prescription of steroid-sparing immunosuppressive drugs. Importantly, no evidence exists indicating that corticosteroids have a disease-modifying effect in SSNS.
Diagnosis
Treatment
- Treatment for nephrotic syndrome involves treating any medical condition that might be causing your nephrotic syndrome. Your doctor might also recommend medications and changes in your diet to help control your signs and symptoms or treat complications of nephrotic syndrome. Medications might include: 1. Blood pressure medications. Drugs called ang...
Clinical Trials
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and Home Remedies
- Changes to your diet might help with nephrotic syndrome. Your doctor might refer you to a dietitian, who might recommend that you do the following: 1. Choose lean sources of protein. Plant-based protein is helpful in kidney disease. 2. Reduce the amount of fat and cholesterol in your diet to help control your blood cholesterol levels. 3. Eat a low-salt diet to help control swelli…
Preparing For Your Appointment
- Start by seeing your primary care doctor. If your doctor suspects you or your child has a kidney problem, such as nephrotic syndrome, you might be referred to a doctor who specializes in the kidneys (nephrologist). Here's some information to help you get ready for your appointment.