| State | State Medicaid Coverage of Methadone for Treatment (2017) |
|---|---|
| Ohio | State Medicaid Program does Cover Methadone |
| Michigan | State Medicaid Program does Cover Methadone |
| Florida | State Medicaid Program does Cover Methadone |
| South Dakota | State Medicaid Program does Cover Methadone |
Is methadone treatment covered by Medicaid?
Only 12 states (24 percent) include methadone services in Medicaid managed care plans. Moreover, two of the 12 states limit coverage for counseling or medication and others permit health plans to set limits.
How do States pay for methadone treatment?
The Society categorized states into three groups, by method of payment for methadone treatment: 1) via Medicaid; 2) only through a SAPT block grant; and 3) no public coverage. (States that had both Medicaid and SAPT block grant coverage were categorized under Medicaid.)
Which states require methadone counseling?
Two states require documentation of counseling, and that is only 17 For Alaska, Kansas, Mississippi, Missouri, Montana, Oklahoma, and South Dakota, we found no evidence of methadone coverage in state Medicaid or MCO documents.
Are methadone clinics legal in America?
Every methadone clinic in America, where these facilities are usually provided, is legally regulated by federal and state laws. The treatments offer various outcomes and you may benefit from them as follows: Avoidance or reduction of the withdrawal symptoms that come when you quit using opioids
Does Medicaid cover methadone in Florida?
Florida Medicaid covers methadone under Fee-For-Service (FFS) plans. In order to receive coverage for methadone for the treatment of opioid use disorder, federal law mandates that patients are enrolled in, or have documented proof of, substance use disorder (SUD) counseling.
Does Arkansas Medicaid cover methadone treatment?
received treatmentα. Arkansas Medicaid does not cover methadone under Fee-for-Service (FFS) plans. medications for the treatment of opioid use disorder.
What state has the most methadone clinics?
In many parts of the United States, methadone clinics are few and far between, which presents problems for addicts seeking methadone treatment who live far from a clinic. The greatest concentrations of clinics are in California, Maryland, New York, and New Jersey.
Does Texas Medicaid cover Suboxone?
Texas covers Suboxone, buprenorphine/naloxone tablets, and buprenorphine tablets as a medical and pharmacy benefit under both FFS and MC plans.
Does Medicaid cover methadone in Georgia?
Georgia Medicaid covers methadone under Fee-For-Service (FFS) plans. In order to receive coverage for methadone for the treatment of opioid use disorder, federal law mandates that patients are enrolled in, or have documented proof of substance use disorder (SUD) counseling.
Does Medicaid cover Suboxone in Michigan?
Michigan covers Suboxone, buprenorphine/naloxone tablets, and buprenorphine tablets as a pharmacy benefit under both FFS and MC plans.
Is methadone free in USA?
Methadone treatment is not free. However, it may be covered fully or partially by health insurance, depending on the type of insurance, the insurance provider, and other factors.
How many years can you take methadone?
Methadone maintenance is a long-term treatment. The length of treatment varies from one or two years to 20 years or more. However, if the person taking methadone and their doctor agree to end treatment, the methadone dose is tapered down gradually over many weeks or months, easing the process of withdrawal.
What is methadone mile?
Mass and Cass, also known as Methadone Mile or Recovery Road, is a tent city located at and around the intersection of Melnea Cass Boulevard and Massachusetts Avenue in Boston, Massachusetts. It has been characterized as "the epicenter of the region's opioid addiction crisis."
Does NC Medicaid cover methadone treatment?
North Carolina Medicaid covers methadone under Managed Care (MC) plans only. In order to receive coverage for methadone for the treatment of opioid use disorder, federal law mandates that patients are enrolled in, or have documented proof of, substance use disorder (SUD) counseling.
Who can prescribe methadone in Texas?
(1) Methadone. The program medical director or program physician shall prescribe methadone in accordance with 42 CFR, §8.12(h)(3-4).
Does WV Medicaid cover Suboxone tablets?
West Virginia covers Suboxone, buprenorphine/naloxone tablets, and buprenorphine tablets as a pharmacy benefit under both FFS and managed care plans. Only Suboxone is listed on West Virginia's preferred drug list for FFS plans.
How to treat methadone overdose?
Most methadone treatment programs will advise you to: 1 Are careful while operating machinery or driving 2 Avoid consuming alcohol while on the medication 3 Get in touch with emergency medical services in case you overdose 4 Keep the methadone away from light sources 5 Store your medications at room temperature
How long does methadone last?
Methadone is a legal medication used to alleviate withdrawal symptoms from opiate drugs for 24 to 36 hours. Having said that, there are a lot of reasons why you may want to enroll in a methadone treatment program. These include, but are not limited to:
How does methadone work?
How methadone programs Work. In all methadone treatment programs, the medication must be provided by trained, registered, and licensed medical professionals and nurses. Patients are mandated to go to the clinic daily to receive their methadone dose, however in some special instances, some clients might receive take-home doses.
How many people were admitted to opiate treatment in 2011?
In 2011, SAMHSA also indicated that close to quarter of a million Americans were admitted into an opiate treatment program, with more than half of them choosing detox and maintenance therapies. Although, only about 22% of patients were receiving maintenance treatment.
Is methadone a pill?
SAMHSA (the Substance Abuse and Mental Health Services Administration) reports that methadone might be provided in wafer, pill, or liquid forms. It is commonly used to block the negative symptoms of such opiate pain medications like oxycodone, codeine, and morphine, along with other semi-synthetic opioids.
Does methadone rehab focus on drug abuse?
In most instances, methadone programs hardly ever just focus on the drug abuse problem only. This is because you may have legal, work related, medical, and social issues that also need to be addressed.
Is methadone clinic more affordable than other alternatives?
Yet, by following the programs strict protocols and recommendations, many clients are able to restore normalcy in their lives. Methadone clinics are also more affordable than other alternative methods since your pricing may be calculated based on your income.
What was the majority of Medicaid patients?
Most patients were women, especially in states that had no public funding for treatment. It’s important to remember that before Medicaid expansion under the Affordable Care Act, which allowed coverage for men, the vast majority of Medicaid enrollees were women .
What is the most common treatment setting for opioid use disorders?
As the table below shows, non-intensive outpatient was the most common treatment setting for patients being treated for opioid use disorders. Fewer than 10% of all patients in residential treatment settings were treated for these disorders.
Does Medicaid pay for methadone?
In 17 states, however, Medicaid does not pay for methadone treatment.
Medicaid Coverage of Medication Assisted Treatment (MAT): A 50-state overview
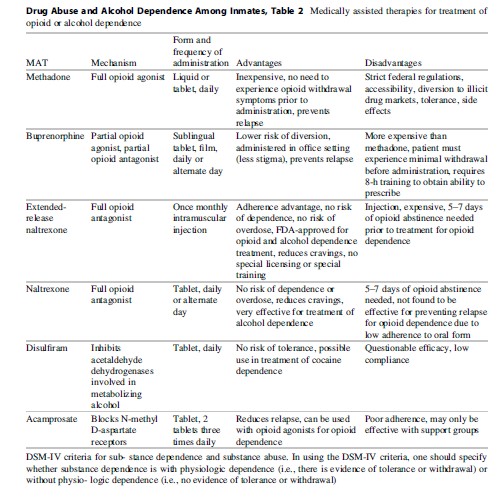
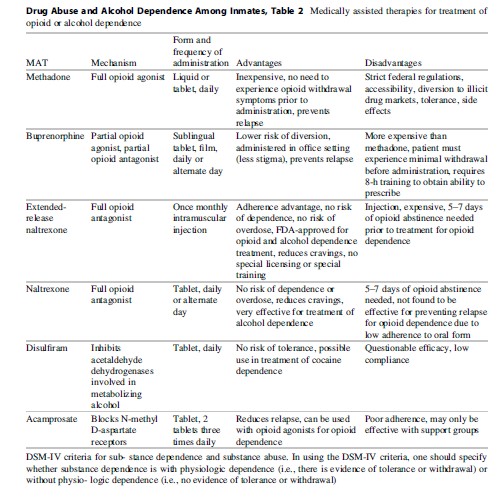
Medication Assisted Treatment (MAT) refers to evidence based therapies used to treat diagnosed opioid dependence. The Centers for Disease Control and Prevention (CDC) has defined an epidemic of overdose deaths related to opioid pain relievers.
Additional MAT Resources
Medication Assisted Treatment, Substance Abuse and Mental Health Services Administration (SAMHSA), 2016
How much does methadone cost without insurance?
On average, the cost of methadone for an individual without insurance is roughly $10-$15 dollars a day, or around $80-$100 per week. Which type a methadone clinic a person seeks, or how the clinic is funded, will likely factor into the cost of methadone without insurance. It may be best for a person to call the clinic and figure out what ...
How does methadone help with addiction?
Research has shown that methadone maintenance therapy: 1 reduces the number of deaths associated with opioid dependence 2 reduces drug injecting and the spread of HIV 3 reduces criminal activity relating to drug use
Does HMO cover MMT?
Whether or not an HMO or PPO plan covers the cost of MMT depends on a variety of factors. It can come down to whether or not methadone treatment is medically necessary, or whether methadone is a covered medication included in the plan. Some plans may cover the cost of methadone, but still require a co-payment.
Is MMT covered by Medicaid?
Research has found that people are more likely to attend MMT when it’s covered by Medicaid than when it’s not. Only 7% of people enrolled in Medicaid in states that do not cover MMT received some form of methadone or buprenorphine treatment.
Does Medicaid cover methadone?
However, it can be said that well over half of all US states include methadone clinics in Medicaid coverage. There may be at least 17 states where Medicaid does not cover methadone clinics, so it depends on which state the person seeks treatment.
Is methadone based on income?
Many public clinics may also use a sliding scale for payment , meaning the cost of methadone treatment is based on a person’s income. Due to the cost and challenges of getting into a methadone clinic, people dependent to opioids may have more success seeking alternative treatments to methadone maintenance therapy.
Does methadone require a co-payment?
Some plans may cover the cost of methadone, but still require a co-payment. The coverage of methadone is likely to vary from plan to plan, but a person with a PPO plan may have more options than someone with a more traditional, and less expensive, HMO plan.
How many patients can you treat with buprenorphine?
Buprenorphine/ buprenorphine-naloxone . Can be prescribed by a physician, nurse practitioner, or physician assistant to up to 30 or 100 patients at a time after completing required training. Some physicians with added qualification or in specific practices may treat up to 275 patients at a time.
What is the number for SAMHSA?
Substance Abuse and Mental Health Services Administration . SAMHSA’s mission is to reduce the impact of substance abuse and mental illness on America’s communities. 1-877-SAMHSA-7 (1-877-726-4727) • 1-800-486-4889 (TDD) • .
Does Medicaid cover buprenorphine?
A review of Medicaid policies and data revealed that all states reimburse some form of buprenorphine, buprenorphine- naloxone, oral naltrexone, and extended-release naltrexone and that most states cover disulfiram and acamprosate.
Is substance use disorder a treatable disease?
Substance use disorder (SUD) also is associated with high costs to both individuals and society (Substance Abuse and Mental Health Services Administration [SAMHSA], 2014a). Addiction, like many other chronic diseases, is a treatable condition.
Is buprenorphine a preferred drug?
Preferred status varies considerably, however, for buprenorphine- naloxone by formulation across states, with preferred status sometimes given to the generic or to one or more of Suboxone, Suboxone film, Zubsolv, or Bunavail, depending on the state. Forty-three states treat some form of naloxone as preferred.