
TYPE 2 DIABETES ADULT OUTPATIENT INSULIN GUIDELINES GENERAL RECOMMENDATIONS Start insulin if A1C and glucose levels are above goal despite optimal use of other diabetes medications. (Consider insulin as initial therapy if A1C very high, such as > 10.0%)
Full Answer
When to consider insulin therapy in patients with T2D hyperglycemia?
AACE Glycemic Control Algorithm: When to Consider Insulin Therapy in Patients With T2D A1C >9.0% and/or symptomatic hyperglycemia; with or without other antihyperglycemic agents In combination with 1-2 other antihyperglycemic agents when A1C is ≥7.5%-9.0%
When is insulin therapy necessary for diabetes?
Insulin therapy becomes necessary for those with advanced disease. Further, some experts recommend electively starting insulin therapy in early diabetes. This review addresses practical approaches to insulin therapy, particularly when it is indicated and which regimen to use.
Does insulin work for type 2 diabetes?
For many patients, it comes after years of having type 2 diabetes and trying multiple weight-loss regimens, diets, and oral medications. For other patients, the decision to take insulin is made when blood glucose levels are simply too high to control with other drugs. The good news is that insulin almost always works.
When is mealtime insulin indicated in the treatment of diabetes mellitus (DM)?
• Patients whose glycemia remains uncontrolled while receiving basal insulin in combination with oral agents or GLP-1 RAs may require mealtime insulin to cover postprandial hyperglycemia. 1,2 DPP4i, dipetydl peptidase 4 inhibitor; GLP -1 RA, glucagon-like peptide-1 receptor agonist; SGLT2i, sodium-glucose cotransporter 2 inhibitor. 1.
See more
When should insulin be started in type 2 diabetes?
Insulin should be initiated when A1C is ≥7.0% after 2–3 months of dual oral therapy. The preferred regimen for insulin initiation in type 2 diabetes is once-daily basal insulin. In addition to timely initiation, rapid titration of the dose is indispensable for successful insulin therapy.
When should a patient start taking insulin?
Insulin therapy will often need to be started if the initial fasting plasma glucose is greater than 250 or the HbA1c is greater than 10%.
When should a diabetic start medication?
For most patients presenting with A1C at or above target level (ie, >7.5 to 8 percent), pharmacologic therapy should be initiated at the time of type 2 diabetes diagnosis (with lifestyle modification).
Which insulin should be given first?
Rapid-acting insulin should always be drawn into the syringe first. This will keep the intermediate-acting insulin from getting into the rapid-acting insulin bottle.
At what blood sugar level should I take insulin?
Insulin is usually recommended as the initial therapy for diabetes if a person's HbA1c level at diagnosis is greater than 10% or if someone's fasting blood glucose level is consistently above 250 mg/dl.
Do I need insulin with type 2 diabetes?
“Someone with Type 1 diabetes will always require insulin injections, because their body produces little or no insulin, but someone with Type 2 diabetes may require insulin injections as part of their treatment plan as well,” said Eileen Labadie, Henry Ford Health diabetes education specialist.
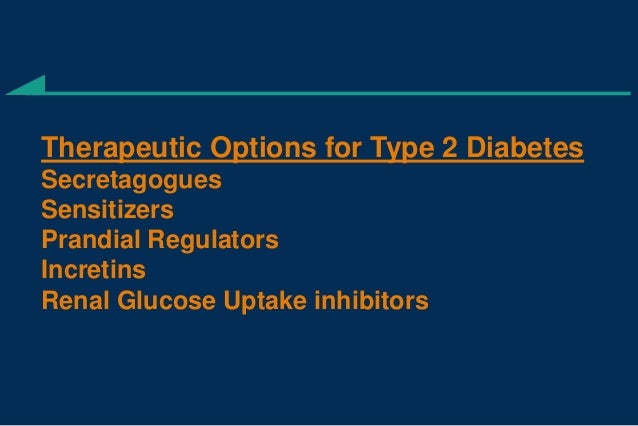
What is first line treatment for type 2 diabetes?
Metformin (Fortamet, Glumetza, others) is generally the first medication prescribed for type 2 diabetes. It works primarily by lowering glucose production in the liver and improving your body's sensitivity to insulin so that your body uses insulin more effectively.
What is a good blood sugar level for type 2 diabetes?
Keep your blood sugar levels close to normal to avoid many of these complications. The American Diabetes Association's goals for blood sugar control in people with diabetes are 70 to 130 mg/dL before meals, and less than 180 mg/dL after meals.
Which insulin is best for type 2 diabetes?
Initial insulin dose — When insulin is started for type 2 diabetes, health care providers usually recommend "basal" insulin; this means taking intermediate-acting and/or long-acting forms of insulin to keep blood sugar controlled throughout the day.
How do I know which insulin to use?
You will need to calculate how much carbohydrate you will eat, and take a dose of insulin that matches the food. A high blood sugar correction bolus insulin dose to bring your blood sugar back into the target range.
How do you start insulin?
Insulin therapy may be initiated as augmentation, starting at 0.3 unit per kg, or as replacement, starting at 0.6 to 1.0 unit per kg. When using replacement therapy, 50 percent of the total daily insulin dose is given as basal, and 50 percent as bolus, divided up before breakfast, lunch, and dinner.
Who can teach you how to measure insulin?
If your health care provider prescribes insulin, a trained diabetes educator or pharmacist can teach you how to measure out the proper dose and administer your daily injections.
What is the HBA1C level?
Your HbA1c level is higher than 10% at diagnosis, or your blood glucose level is higher than 300 mg/dL at any time of day (or higher than 250 mg/dL after not eating for at least 8 hours). You have side effects to other diabetes medications and have poorly controlled blood glucose.
Is insulin a treatment for type 2 diabetes?
Insulin Treatment in Type 2 Diabetes. The decision to take insulin is never an easy one. For many patients, it comes after years of having type 2 diabetes and trying multiple weight-loss regimens, diets, and oral medications. For other patients, the decision to take insulin is made when blood glucose levels are simply too high to control ...
Treatment Delays and Barriers
Patient and clinician factors contribute to delays in adding insulin to treatment regimens or in transitioning from oral antidiabetic agents (OADs) to insulin.
Advanced Basal Insulin Analogs and Fixed-Ratio Combinations
Advanced insulin analogs and pre-filled pen delivery devices are helping to overcome some of the barriers to insulin initiation and titration experienced by some patients and PCPs.
Current Guidelines for Insulin Initiation and Titration
The American Diabetes Association (ADA) recommends initiation of basal insulin at 10 units/day or 0.1–0.2 units/kg/day, adjusted by 10–15% or 2–4 units once or twice weekly to reach a target fasting plasma glucose (FPG) in patients whose A1C remains uncontrolled after >3 months of triple combination therapy, whose A1C is >10%, whose blood glucose is >300 mg/dL, or who are symptomatic of hyperglycemia ( 37 ).
Insulin Titration Algorithms
A number of titration algorithms have been evaluated that aim to simplify insulin titration and enable patient empowerment through self-titration to effectively participate in the management of their disease ( 4, 39 – 42 ), the details of which are summarized in Table 1.
When Too Much Insulin Has Little Effect on Glycemic Target
Current use of basal insulin has been shaped by treat-to-target trials that have emphasized systematically titrating the insulin dose without limit until an FPG of 100–130 mg/dL is reached ( 50 ). “Overbasalization” is said to occur when FPG is uncontrolled despite uptitration of basal insulin and the A1C target remains unmet ( 51 ).
Managing Insulin Regimens in the Primary Care Setting
It is important to gain an understanding of a patient’s background and lifestyle before initiating insulin to ensure that the treatment regimen takes into account the patient’s needs and preferences as well as clinical characteristics ( 37, 56, 57 ).
Conclusion
Multiple insulin algorithms have been developed to help PCPs with insulin initiation and titration and to enable patient self-management.
When to start NPH insulin?
Start NPH insulin in the evening. Start long- acting insulins in the evening or morning. • When insulin becomes necessary, add a single daily dose of basal insulin to the regimen. • Adjust dosage at regular and initially short intervals, measured in days, to achieve targeted glycemic goal while avoiding hypoglycemia.
Why is basal insulin analog used?
1. • Basal insulin analogs are preferred over NPH insulin because a single basal analog dose provides a relatively flat serum insulin concentration for ≥24 hours. 2. • Long-acting basal analogs (glargine U100 or detemir) have been shown to reduce the risk of symptomatic and nocturnal hypoglycemia vs NPH insulin.
Is inhaled insulin dose dependent?
Responses to inhaled insulin are dose- dependent. Only consider inhaled insulin on an individual basis. Dose conversion is required, as is initial and ongoing evaluation of lung function. Contraindicated in patients with chronic lung disease.
