In fact, in most people, bradycardia does not require treatment unless patients have symptoms that are clearly due to a slow heartbeat. The following are conditions that produce bradycardia that requires treatment: Cardiac arrhythmias resulting from sinus node dysfunction.
How to cure bradycardia naturally?
Feb 03, 2020 · In fact, in most people, bradycardia does not require treatment unless patients have symptoms that are clearly due to a slow heartbeat. The following are conditions that produce bradycardia that requires treatment: Cardiac …
How serious is bradycardia?
Dec 26, 2018 · In which situation does bradycardia require treatment? (a) 12-lead ECG showing a normal sinus rhythm (b) Hypotension (c) Diastolic blood pressure > 90 (d) Systolic blood pressure > 100 (b) Hypotension. A 67 yr old woman has palpitations, chest discomfort, and tachycardia. The monitor shows a regular wide-complex QRS at a rate of 180/min.
When does bradycardia require treatment ACLS?
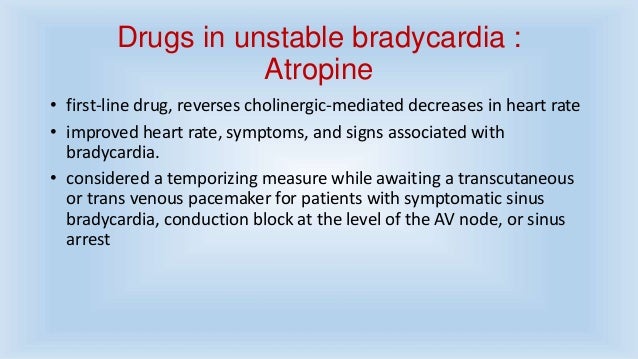
Sep 20, 2021 · Patients with impending heart failure or unstable patients with bradycardia require immediate treatment. The preferred drug is usually 0.5 to 1.0 mg atropine administered intravenously at 3-5 minute intervals up to a dose of 0.04 mg / kg. Other auxiliary drugs that can be given are adrenaline (adrenaline) and dopamine. What drugs are used in ACLS?
What is the most common bradycardia treatment?
Jan 14, 2020 · A bradycardic rhythm is most often treated only when symptoms are present. If reversible causes aren’t immediately identified and/or if reversing the cause is taking too long, pharmacologic interventions are the first-line approach for bradycardia treatment.
/sinus-bradycardia-1746253-01-912dc3d6234044d6a2fe921327efb28d.png)
At what point does bradycardia require treatment?
Regardless of the patient's rhythm, if their heart rate is too slow and the patient has symptoms from that slow heart rate, the bradycardia should be treated to increase the heart rate and improve perfusion, following the steps of the bradycardia algorithm below.
What is the initial treatment for bradycardia?
Atropine. In the absence of reversible causes, atropine remains the first-line drug for acute symptomatic bradycardia (Class IIa).Nov 28, 2005
How is ACLS bradycardia treated?
If the patient is symptomatic, administer atropine 1.0 mg IV or IO bolus and repeat the atropine every 3 to 5 minutes to a total dose of 3 mg: If atropine does not relieve the bradycardia, continue evaluating the patient to determine the underlying cause and consider transcutaneous pacing.
What is the priority intervention for symptomatic bradycardia?
Note: If dealing with primary bradycardia (defined above), atropine is preferred as the first-choice treatment of symptomatic AV block. If dealing with secondary bradycardia, atropine is not indicated for the treatment of AV block, and epinephrine should be used.
Is a heart rate of 48 too low?
A normal resting heart rate for most people is between 60 and 100 beats per minute (bpm). A resting heart rate slower than 60 bpm is considered bradycardia.May 7, 2018
Is a heart rate of 55 too low?
Bradycardia is a heart rate that's too slow. What's considered too slow can depend on your age and physical condition. Elderly people, for example, are more prone to bradycardia. In general, for adults, a resting heart rate of fewer than 60 beats per minute (BPM) qualifies as bradycardia.Sep 30, 2016
What is a first line treatment for a patient with unstable bradycardia?
The American Heart Association recommends atropine sulfate as the first line of treatment for symptomatic bradycardia, regardless of whether it is due to AVB or not.Nov 23, 2019
Can you do CPR on bradycardia?
The CC are performed during bradycardia to optimize organ perfusion, especially to the heart and brain. Among adults and children undergoing cardiopulmonary resuscitation (CPR), CC is indicated only for pulselessness or poor perfusion.Oct 29, 2019
How is bradycardia treated in nursing?
Atropine. If adverse signs associated with bradycardia are identified following assessment, atropine is the first drug treatment (Wyatt et al, 2006). Atropine blocks the action of the vagus nerve and the aim is to increase the heart rate.Feb 1, 2010
What can a nurse do for bradycardia?
Nursing management includes: Careful physical assessment of the patient. Assessment of vital signs, with special attention to heart rate. Especially, prior to administering a medication which may have an effect on heart rate or blood pressure.Aug 9, 2021
In what situations should bradycardia be treated?
If a patient with bradycardia presents with evidence of poor blood flow, treatment is recommended. Bradycardia with poor circulation can be life-threatening in some cases. Initial treatment includes airway support to ensure that the patient is adequately ventilated.
What is the best procedure to treat a patient with asystole?
The only two medications recommended or accepted by the American Heart Association (AHA) for adults with asystole are adrenaline and vasopressin. Atropine has not been recommended in children and infants since 2005 and in adults with heartless electrical activity (EPA) and heart failure since 2010.
Likewise, how is ACS treated for bradycardia?
There are 3 drugs used in the ACLS Bradycardia Algorithm. These are atropine, dopamine (infusion) and adrenaline (infusion). Dopamine: Another drug for symptomatic bradycardia when atropine is ineffective. The dosage is 220 micrograms / kg / min by infusion.
Can bradycardia cause a stroke?
Collectively referred to as bradycardia-tachycardia or tachybradia syndrome. This is a type of sick sinus syndrome and can be associated with atrial fibrillation of the heart rhythm and increase the risk of complications such as stroke and sudden death or cardiac arrest.
Does caffeine help bradycardia?
The effects of low and high doses of caffeine on idiopathic bradycardia and hypoxemia were tested in preterm infants. A low dose of caffeine significantly reduced the incidence of bradycardia (less than 0.01) but not the incidence of hypoxemia.
When should you not use atropine?
The required dose of atropine is 0.5 mg IV. every 35 minutes and the maximum total dose to be administered is 3 mg. Atropine should be avoided in hypothermic bradycardia and is in most cases not effective in Mobitz type II / 2nd degree type 2 block or complete heart block.
How much atropine should I take for bradycardia?
The recommended dose of atropine for bradycardia is 0.5 mg IV. every 3-5 minutes with a maximum total dose of 3 mg.
Answer
Bradycardia is a slower than normal heart rate. The average heartbeat of an adult at rest is usually between 60 and 100 times a minute. If one has their heart beats fewer than 60 times a minute. bradycardia is not considered a health problem but in cases of Hypotension bradycardia requires treatment
New questions in Social Studies
3 Type the correct answer in the box. Spell all words correctly. What are the three ways through which a company tries to sell its products? Businesse …
What are the symptoms of bradycardia?
5. Common bradycardia symptoms include: syncope. presyncope. transient dizziness or lightheadedness. fatigue. dyspnea on exertion. heart failure symptoms.
What is bradycardia heart rate?
What is bradycardia? The National Institutes of Health defines bradycardia* as a heart rate <60 bpm in adults other than well-trained athletes. 9 The determination on whether or not treatment is necessary for bradycardic events is generally based on the presence of bradycardia symptoms. The clinical manifestations of bradycardia can vary widely from insidious symptoms to episodes of frank syncope. 5
What percentage of patients with sleep apnea have sinus bradycardia?
The prevalence of sinus bradycardia in patients with sleep apnea can be as high as 40%, with episodes of second- or third-degree AV block in up to 13% of patients. 8
How much atropine is given?
Atropine 0.5 mg intravenous (IV) is given up to a total of 3 mg. 1 Atropine sulfate acts by reversing the cholinergic-mediated decreases in the heart rate and AV node conduction. 1. If atropine is ineffective, two treatment pathways are available.
What pharmacologic choice is given for heart pacing?
The two pharmacologic choices are dopamine 2 to 20 mcg/kg/min and/or epinephrine 2 to 10 mcg/min. 1.
When a patient is evaluated for symptomatic bradycardia, an in-depth history and physical is
When a patient is evaluated for symptomatic bradycardia, an in-depth history and physical is important, along with the identification of possible reversible causes. The following is a list of conditions associated with bradycardia and conduction disorders: 11
Can exercise be used to diagnose ischemia?
Exercise Testing. Although not routinely recommended for assessment of ischemia, exercise testing can be considered in patients with symptoms temporally related to exercise, asymptomatic second-degree AV block, or for suspected chronotropic incompetence. 11.