Medication
Treatment may include: Antibiotics. You'll likely be given a course of antibiotic medication to fight the infection and prevent it from spreading. The type and duration of your antibiotic therapy depend on the severity of your condition and the kind of peritonitis you have.
Procedures
Which IV solution to administer is related to the reason for the fluid loss. Crystalloid solutions contain small particles that that pass easily from the bloodstream to cells and tissues. There are three types of crystalloids, given according to their tonicity, the ability to make water move into or out of a cell by osmosis.
Nutrition
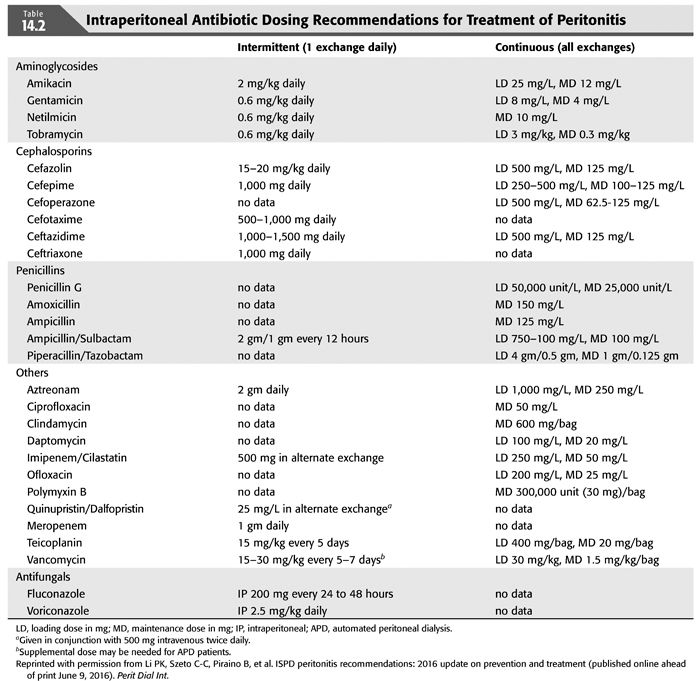
Initial treatment of dialysis associated peritonitis: A controlled trial of vancomycin versus cefazolin. Perit Dial Int1991; 11:31–7.
See more
Omental wrapping or serosal patching are recommended to re-inforce anastomoses in the face of peritonitis. Serosal patching is a technique in which loops of healthy bowel are loosely sutured to the bowel adjacent to the anastomosis.
What are the treatment options for peritonitis?
Which IV solution to administer for fluid loss?
Which medications are used in the treatment of dialysis associated peritonitis?
How is peritonitis treated in the face of anastomosis?

What are the treatment options for peritonitis?
Peritonitis treatment usually involves antibiotics and, in some cases, surgery. Left untreated, peritonitis can lead to severe, potentially life-threatening infection throughout your body. A common cause of peritonitis is peritoneal dialysis therapy.
How is septic peritonitis treated?
Although surgery is the definitive treatment once the diagnosis of septic peritonitis has been made, establishing vascular access and initiating aggressive fluid resuscitation is the first priority. Volume replacement fluids are given to correct hypovolemia and metabolic changes.
How do I choose IV fluids?
2:0013:29IV Fluids for Beginners - When to Use Each IV Fluid Type?? - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo the first thing we're going to be looking at is normal saline and really normal saline is onlyMoreSo the first thing we're going to be looking at is normal saline and really normal saline is only made out of two components. It's made out of sodium. And chloride which is salt.
Why do you give IV fluids in sepsis?
IV Fluids. Antibiotics alone won't treat sepsis; you also need fluids. The body needs extra fluids to help keep the blood pressure from dropping dangerously low, causing shock. Giving IV fluids allows the health care staff to track the amount of fluid and to control the type of fluid.
What is peritoneal sepsis?
Intra-abdominal sepsis is an inflammation of the peritoneum caused by pathogenic microorganisms and their products. The inflammatory process may be localized (abscess) or diffuse in nature.
What is the difference between sepsis and peritonitis?
Symptoms of sepsis are fever, increased breathing and heart rate and infection present in another part of the body, such as a urinary tract infection or an infected tooth. Peritonitis symptoms include abdominal pain, may involve vomiting or diarrhea, dehydration and increased heart rate (so some overlap exists).
Which of the 4 most common IV fluids is used for hydration?
0.9% Normal Saline (NS, 0.9NaCl, or NSS) is one of the most common IV fluids, it is administered for most hydration needs: hemorrhage, vomiting, diarrhea, hemorrhage, drainage from GI suction, metabolic acidosis, or shock.
When do you use lactated Ringers vs normal saline?
In comparison, normal saline (NS) has an osmolarity of about 286 mOsm/L. Ringer's lactate is largely used in aggressive volume resuscitation from blood loss or burn injuries; however, Ringer's lactate is a great fluid for aggressive fluid replacement in many clinical situations, including sepsis and acute pancreatitis.
What is the most common IV solution?
Crystalloid solutions remain by far the most common, largely due to the overwhelming presence of normal saline in most hospital and healthcare settings.Normal Saline. The best-known name is normal saline, sometimes called 9% normal saline, NS, or 0.9NaCL. ... Half Normal Saline. ... Lactated Ringers. ... Dextrose.
Which IV fluid is best for sepsis?
Answer: Crystalloid solutions remain the resuscitative fluid of choice for patients with sepsis and septic shock. Balanced crystalloid solutions may improve patient-centered outcomes and should be considered as an alternative to 0.9% normal saline (when available) in patients with sepsis.
Why is LR better than NS in sepsis?
The difference between the sodium and chloride in LR is 21 (130-109=21), which is nearly equal to a patient's normal bicarbonate of 24 mEq/L and so is considered a “balanced fluid;” it does not cause the acidosis associated with NS.
Can lactated ringers be used for sepsis?
This prospective cohort study found that using lactated Ringers solution for resuscitation in sepsis patients decreased mortality and shortened the lengths of ICU and hospital stays compared with using saline, especially in patients with chronic pulmonary disease, without chronic kidney disease, without moderate to ...
How do you know if you have peritonitis?
Bloating or outward expansion of the abdomen (also known as distention) Nausea and vomiting. Fe ver. Cloudy peritoneal fluid during peritoneal dialysis treatment.
Can peritonitis cause sepsis?
Peritonitis can be life-threatening and may cause serious complications, depending on the cause and severity. It can also lead to sepsis, a life-threatening condition caused by the body’s reaction to an infection. Common symptoms of peritonitis can include: Pain in the abdomen (belly area) Tenderness within abdomen.
Can peritoneal dialysis cause peritonitis?
Peritonitis can also affect people on peritoneal dialysis. Improved technology and self-care methods have lowered the risk of peritonitis for people on peritoneal dialysis, but the risk for infection still remains.
Can antibiotics be given in peritoneal dialysis fluid?
If peritonitis happens with peritoneal dialysis then the antibiotics can be given in the peritoneal dialysis fluid. Sometimes a different form of dialysis might be needed temporarily while the body heals from the infection.
What is IV therapy?
All nursing programs include fluid balance and intravenous (IV) therapy as part of the curriculum. The information about the types of IV solutions and when to use them can be confusing for a nursing student. Nurse.Plus is happy to offer this simple reference guide to the four basic types.
What is the most common solution used in osmosis?
Crystalloid Solutions: Most Commonly Used. Crystalloid solutions contain small particles that that pass easily from the bloodstream to cells and tissues. There are three types of crystalloids, given according to their tonicity, the ability to make water move into or out of a cell by osmosis.
What happens when fluid is lost?
Joint lubrication. When fluid is lost for any reason, electrolytes become imbalanced, body systems are stressed, and cognitive function in the brain is impaired. Blood becomes concentrated, signaling the kidneys to retain water. As a result, urine output is decreased.
Can you give saline solution via IV?
Normal saline solution can be administered only via intravenous (IV) access. 0.9% Normal Saline (NS, 0.9NaCl, or NSS) is one of the most common IV fluids, it is administered for most hydration needs: hemorrhage, vomiting, diarrhea, hemorrhage, drainage from GI suction, metabolic acidosis, or shock. It is an isotonic crystalloid ...
Is saline a sterile fluid?
It is a sterile, nonpyrogenic crystalloid fluid administered via an intravenous solution. Normal saline infusion is used for extracellular fluid replacement (e.g., dehydration, hypovolemia, hemorrhage, sepsis), treatment of metabolic alkalosis in the presence of fluid loss, and for mild sodium depletion.
Overview
IV fluids are liquids injected into a person’s veins through an IV (intravenous) tube. They prevent or treat dehydration and electrolyte imbalances.
Procedure Details
There are different kinds of IV fluids. Your healthcare provider will decide which type is right for you, depending on why you need them.
Recovery and Outlook
Many people don’t need recovery time or have any restrictions after receiving IV fluids.
When to Call the Doctor
Tell your healthcare provider if the IV fluids seem to be flowing too slowly or too quickly.
How to treat peritonitis in animals?
One of the most important aspects of treating peritonitis is prompt removal of the inciting cause. Whilst the animal should be stabilized before anesthesia and surgery, the underlying source of the peritonitis must be addressed to resolve the peritonitis. Exploratory laparotomy is mandatory to treat the source of the peritonitis, remove peritoneal contamination and exudate, and provide a source for enteral nutrition. A large ventral midline incision is used for exposure. A complete exploratory laparotomy is performed. The source of the peritonitis is identified and isolated from the remained of the abdomen using moistened laparotomy sponges. In animals with generalized peritoneal contamination, the author prefers to lavage the peritoneal cavity with a large volume of warm sterile saline before proceeding with definitive treatment. The fluid is immediately aspirated from the peritoneal cavity.
What happens to the peritoneum when vascular permeability increases?
Chemical injury results in inflammation of the peritoneum. Vasodilation and increased vascular permeability initially results in the loss of isotonic fluid. As vascular permeability increases, albumin is lost into the peritoneal space. Given the large peritoneal surface area, fluid and protein loss can be massive. White blood cells, fibronectin, and fibrin also enter the peritoneal space. Diaphragmatic lymphatics which normally return peritoneal fluid to the systemic circulation become overloaded and plugged with fibrin. Concurrent vomiting and diarrhea exacerbate fluid loss. Fluid loss decreases circulating blood volume and results in a decreased cardiac output and poor tissue perfusion. Poor tissue perfusion results in cellular hypoxia and anaerobic cellular metabolism. Cellular energy depletion causes loss of cell membranae integrity, cell death, and eventually organ failure.
Is peritonitis a septic disease?
In most cases, peritonitis occurs as a sequela to some other disease process. Secondary peritonitis can be aseptic or septic. Aseptic peritonitis may be secondary to foreign bodies (surgical sponges), ruptured neoplasms, or chemical agents such as pancreatic enzymes, bile (which can contain bacteria), urine, and stomach or proximal duodenal contents, in which bacterial concentrations are low.
Is peritonitis a sign of septic peritonitis?
Depression and diffuse abdominal pain of a degree greater than that usually seen following abdominal surgery or trauma are often present. Most animals splint their abdominal wall at the slightest touch. Vomiting is also a prominent sign of peritonitis. Peritoneal inflammation often causes a paralytic ileus and intestinal dilatation, in addition to the massive effusion. In septic peritonitis, fever and leukocytosis are not consistent findings.
Informed consent
is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it.
An IV
is a small tube placed in your vein that is used to give you medicine or liquids.
Intake and output
Healthcare providers will keep track of the amount of liquid you are getting. They also may need to know how much you are urinating.
Medicines
Pain medicine may be given. Do not wait until the pain is severe before you ask for more medicine.
Tests
Blood tests are used to check your white blood cell (WBC) count. An increase in WBCs may be a sign of infection. Your blood may also be tested for bacteria or a fungus.
Treatment
A nasogastric (NG) tube may be placed if you are at risk for aspiration (inhaling liquid) because you are bleeding in your esophagus or vomiting. Air or extra fluid may also be removed through the NG tube.
RISKS
You may develop an abscess (collection of pus) in your abdomen that needs to be treated. You may develop gangrene (tissue death) in your bowel. Septic shock may develop. Septic shock is dangerously low blood pressure. You may develop kidney or liver failure, or you may have trouble breathing.
How long does it take to get antibiotics for peritonitis?
In uncomplicated peritonitis in which there is early, adequate source control, a course of 5-7 days of antibiotic therapy is adequate in most cases. Mild cases (eg, early appendicitis, cholecystitis) may not need more than 24-72 hours of postoperative therapy.
What causes peritonitis in the small intestine?
Peritonitis can be caused by perforation of a tubercular ulcer (usually in the small intestine), rupture of a caseous lymph node or as primary tuberculous peritonitis due to involvement of the peritoneum. Diagnosis of tuberculosis is established by histologic examination of the resected bowel, lymph node or peritoneal biopsy.
Is intra-abdominal contamination a risk factor for candidiasis?
Patients with intra-abdominal contamination are at a high risk for candidiasis, and this has led to the increased use of antifungal prophylaxis. Patients who are immunocompromised or who have received long-term, broad-spectrum antibiotic therapy (eg, patients with severe acute necrotizing pancreatitis) or steroid therapy are predisposed to candidal infections.
Is enterococcal coverage warranted?
Enterococcal coverage may be warranted in patients with septic shock who have received prolonged cephalosporin therapy, in patients who are immunosuppressed and are at risk for bac teremia, in patients with prosthetic heart valves, and in patients with recurrent intra-abdominal infections accompanied by severe sepsis.
Is broad spectrum therapy effective against abdominal infections?
Single-agent, broad-spectrum therapy and combination therapies have been used against these infections, although no specific therapy has been found to be superior to another. Infection of the abdominal cavity requires coverage for gram-negative and gram-positive bacteria, as well as for anaerobes.
Is peritoneal infection a secondary infection?
Peritoneal infections are classified as primary, secondary, or tertiary. Primary peritoneal infections arise from hematogenous dissemination, usually in the setting of an immunocompromised state, while secondary infections are related to a pathologic process in an abdominal organ, such as perforation, ischemia and gangrene, trauma, ...
What is the best treatment for peritonitis?
Oxygen therapy. Oxygen therapy by nasal cannula or mask generally promotes adequate oxygenation. Antibiotic therapy. Antibiotic therapy is initiated early in the treatment of peritonitis.
What is the pathophysiology of peritonitis?
The pathophysiology of peritonitis involves: Leakage. Peritonitis is caused by leakage of contents from abdominal organs into the abdominal cavity. Proliferation. Bacterial proliferation occurs. Edema. Edema of the tissues occurs, and exudation of fluid develops in a short time. Invasion.
What is the peritoneum of diverticulitis?
Peritonitis is the inflammation of the peritoneum, the serous membrane lining the abdominal cavity and covering the viscera.
What causes peritonitis in the kidneys?
Inflammation. An inflammation that extends from an organ outside the peritoneal area such as the kidne ys could cause peritonitis. Bacteria. The most common bacteria implicated are Escherichia coli, Klebsiella, Proteus, Pseudomonas, and Streptococcus.
What is the major cause of death from peritonitis?
Sepsis. Sepsis is the major cause of death from peritonitis. Shock. Shock may result from septicemia or hypovolemia. Intestinal obstruction. The inflammatory process may cause intestinal obstruction, primarily from the development of bowel adhesions.
What is the immediate response of the intestinal tract?
Response. The immediate response of the intestinal tract is hypermotility, soon followed by paralytic ileus with an accumulation of air and fluid in the bowel.