
Medication
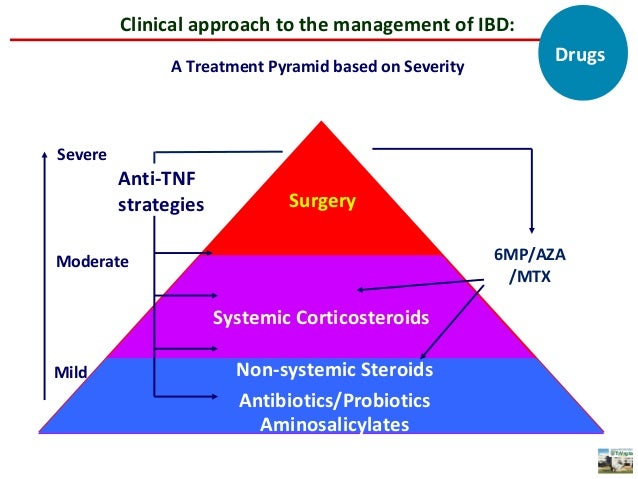
What kind of treatments are there for IBD?
- Several healthcare providers
- Medications
- Surgery
- Symptom management
- Complementary/alternative medicine
Procedures
Some that work well in the workplace include:
- Breathing exercises.
- Meditation.
- Guided imagery (a technique that focuses the imagination in a positive way, often with words or music).
- Recordings that promote relaxation.
Nutrition
What does treat to target really mean in IBD? By Brendan Halloran, MD Volume 2 - Issue 11. Runs 1:44. A major goal of the treat-to-target approach is achieving mucosal healing in patients with inflammatory bowel disease (IBD).(1) Appropriate drug levels can facilitate reaching this goal, which can reduce the occurrence of flares and the need ...
What are the different treatment options for IBD?
The discovery could also one day lead to the development of more targeted treatments for the condition, which currently has no cure. Shiokawa and Kuwada’s revelations on the key players behind ulcerative colitis came off the back of their previous ...
How do IBD patients cope with IBD?
What does treat to target really mean in IBD?
Is there a cure for IBD?

What is the first line treatment for ulcerative colitis?
Aminosalicylates. Aminosalicylates, also known as 5-ASAs, are medicines that help to reduce inflammation. This in turn allows damaged tissue to heal. They're usually the first treatment option for mild or moderate ulcerative colitis.
What is the first line therapy for inflammatory bowel disease in the outpatient setting?
The first step in medication therapy for mild IBD is usually aminosalicylates. There are several different aminosalicylates, but none have been consistently demonstrated to be superior to the others for all patients.
What is the first line treatment for Crohn's disease?
Anti-inflammatory drugs are often the first step in the treatment of inflammatory bowel disease. They include: Corticosteroids. Corticosteroids such as prednisone and budesonide (Entocort EC) can help reduce inflammation in your body, but they don't work for everyone with Crohn's disease.
What is treat to target IBD?
In 2015, the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) committee defined the treat-to-target (T2T) approach for inflammatory bowel disease (IBD), which shifted the goal of UC treatment to long-term prevention of disease complications (dysplasia/cancer, hospitalizations, colectomy) and ...
How much prednisone should i take for IBD?
The most common range for moderate flares of IBD is prednisone at 10-40 mg/day. For more severe flares, doses up to 60 mg/day may be used, but there are no supportive data. Once a clinical response is seen, the dose is tapered.
How long does prednisolone take to work for IBD?
HOW LONG DO STEROIDS TAKE TO WORK? Oral steroids normally improve symptoms within one to four weeks, while intravenous steroids take four to 10 days. Around one in five people shows no response to steroid treatment (this is known as being steroid refractory). If your condition is not improving, contact your IBD team.
When should you start a biologic for Crohn's?
The American College of Gastroenterology recommends a biologic if you have moderate-to-severe active Crohn's that hasn't gotten better using other medications. Certolizumab pegol (Cimzia) is one biologic prescribed to adult patients who haven't been helped enough by traditional drugs.
How long does it take for inflamed intestines to heal?
Treatment often involves intravenous nutrition to allow the bowel to rest, which typically resolves the disease within one or two weeks. However, in some cases, surgery might be necessary.
Does Crohn's always show on colonoscopy?
Gastroenterologists almost always recommend a colonoscopy to diagnose Crohn's disease or ulcerative colitis. This test provides live video images of the colon and rectum and enables the doctor to examine the intestinal lining for inflammation, ulcers, and other signs of IBD.
What is the latest treatment for ulcerative colitis?
Federal regulators have approved the new drug Zeposia for treating moderate to severe ulcerative colitis in adults. The medication is the latest in a line of drugs used to treat symptoms of this particular type of inflammatory bowel disease (IBD).
What is the best medicine for IBD?
Aminosalicylates are anti-inflammatory medicines generally used for longer-term treatment of people with mild-to-moderate IBD
What is the primary part of an IBD treatment plan?
A primary part of any patients IBD treatment plan are medications that are used to directly treat the disease as well as the inflammation that it causes. 2 Patients may need to try different types of medicines or combinations of medicines, in order to find the regimen that works most effectively to treat their disease and manage their symptoms. The goals of treatment with IBD medications are:
What is the autoimmune disease of the bowel?
Inflammatory bowel disease ( IBD) is a chronic condition in which long-term inflammation can cause symptoms and complications affecting the digestive tract. The two major forms of IBD are Crohn's disease and ulcerative colitis. IBD is a complicated autoimmune condition that affects every person in a unique way. This means that finding the best way to treat it can also be a complex process that involves trying a range of different strategies in order to find the most effective one. IBD is also a disease that changes over time, so a treatment strategy that works for a person at one stage may not work as well (or at all) at a different time.
Why do vets say IBD is caused by toxins?
Many holistic vets say an IBD is caused by a reaction to toxins – including toxins in the diet, too many vaccinations, and excessive use of flea and tick medications. As a result, detoxification is an important part of treatment, they say. Finding a diet that is easy on the GI tract is vital.
What to do if my dog has inflammatory bowel disease?
digestive health. steroids. Detoxification could be just what the doctor ordered for the treatment of your dog’s inflammatory bowel disease. Reducing toxins in your dog’s diet is the goal, say holistic vets.
What to give a dog to help with GI issues?
Finding a diet that is easy on the GI tract is vital. Other therapies include adding probiotics, enzymes, glutamine, and herbs such as marshmallow root to the dog’s diet. Detoxification with homeopathics and herbs, such as milk thistle, further assist in healing.
Can dogs have IBD?
Exactly why some dogs come down with an IBD is a mystery, but what they’ve eaten certainly can be a cause or contributing factor . IBD should be suspected in any pet with chronic diarrhea (lasting three weeks or more).
What is the treatment for inflammatory bowel disease?
Current therapy of moderate-to-severe inflammatory bowel disease (IBD) often involves the use of anti-tumor necrosis factor alpha (TNF-α) agents. Although very effective, theses biologics place the patient at increased risk for developing infections and lymphomas, the latter especially when in combination with thiopurines.
How long does it take to start biological therapy for IGRA?
Patients may start biological therapy after 1–2 months of a total of 9 months of anti-tuberculosis treatment [30]. If conditions for performing the IGRA test do not exist, TST associated with chest X-ray can be used, in addition to considering the clinical history and physical examination.
What are the treatments for TNF-?
Currently, 4 anti-TNF-α therapies are available for treatment of patients with IBD. These agents are infliximab, adalimumab, certolizumab pegol, and golimumab. Although there are differences in routes and timing of administration of these drugs, the pretreatment evaluation protocol is similar regardless of the biologic agent used. For a variety of other immunosuppressants (e.g., azathioprine, 6-mercaptopurine, and methotrexate), the same considerations also apply, and the principles that will be disputed in this article can be used for treatment with these drugs. Nevertheless, particular precautions associated with each of these immunomodulators should be evaluated prior to initiating treatment. Herein, we review the preparation of the IBD patient for biologic therapy (Table 1), which is a pivotal issue for achieving the final aims of improving the patient’s risk/benefit ratio and outcome.
Can HBV reactivate during immunosuppressive therapy?
Although less common, HBV reactivation can also occur during immunosuppressive therapy in patients with occult HBV infection defined by a quiescent infection in HBsAg/anti-HBc-positive or anti-HBc-positive/anti-HBs-positive patients and DNA persisting in the nucleus of hepatocytes [39].
Can anti-TNF- be used to treat latent infections?
An increased risk of both opportunistic infections and latent infection flare-up is observed during anti-TNF-α therapy; thus, an efficient strategy must be used to try to reduce the occurrence of adverse events. If we consider that in such circumstances infections can have significant morbidity and potential fatal outcome, it is necessary to establish rules to be followed to identify latent and sometimes silent infections before the use of this class of drugs [12]. In particular, we discuss the screening for tuberculosis (TB), hepatitis B and C, varicella zoster virus (VZV), and human immunodeficiency virus (HIV).
Can TNF be used for IBD?
Prior to commencing anti-TNF-α therapy for patients with IBD, other illnesses with a similar presentation need to be excluded. Foremost among these is irritable bowel syndrome. A recent meta-analysis of patients with IBD demonstrated that 25–46% of those in clinical remission have symptoms compatible with a diagnosis of irritable bowel syndrome [10]. Patients who are in remission, but who experience important functional symptoms (e.g., abdominal pain, distension, and diarrhea) may have symptoms that mimic active disease, and thus receive inappropriate and potentially harmful anti-TNF-α therapy.
What is the treatment for IBD?
During your treatment for IBD it's likely you will be given an induction therapy, followed by a maintenance therapy . Find out more about what this means...
What is maintenance therapy for IBD?
Maintenance therapy in IBD is used to keep you well when your Crohn’s disease or ulcerative colitis is under control (in remission). Maintenance treatments are long-term treatments that you may stay on for many years if they work for you. Which maintenance therapy you will be given to keep your IBD under control will depend on your unique ...
What are the best treatments for Crohn's disease?
Induction treatments for Crohn’s disease include: 1 Steroids (such as prednisolone and budesonide) 2 Exclusive enteral nutrition (EEN) - usually only used in children 3 Biologics (such as infliximab, adalimumab, vedolizumab and ustekinumab) 4 Aminosalicylates may also be used, however research indicates they may not be as effective in Crohn’s disease as they are in ulcerative colitis 1
What is induction therapy for Crohn's disease?
What is induction treatment for Crohn’s disease and ulcerative colitis? Induction therapy in inflammatory bowel disease (IBD) is used to get you well and into remission by quickly reducing the inflammation in your digestive system. If you are newly diagnosed with Crohn’s disease or ulcerative colitis, or you are in a flare of your IBD, ...
Why is it important to keep IBD under control?
Keeping your IBD under control is really important to avoid having complications. That’s why you should keep taking your maintenance treatment, even if you aren’t experiencing any symptoms of your Crohn’s disease or ulcerative colitis.
How long does it take for a corticosteroid to go into remission?
You will take a short course of a corticosteroid, such as prednisolone, for six to eight weeks before slowly tapering (reducing) the dose.
How long does it take for immunomodulators to work?
As immunomodulators can take up to three months to reach their therapeutic range in your body, it is likely you will be started on an immunomodulator at the same time as starting steroids, or shortly after, to give it plenty of time to start working.
Diagnosis
Clinical Trials
Lifestyle and Home Remedies
Alternative Medicine
Specialist to consult
Coping and Support
Preparing For Your Appointment
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.