Elements of purposeful and thorough progress notes include: Client’s SUD goal in his/her own words Client’s overall treatment objectives and SMART goals Client’s past history and current presentation Current issues, barriers to progress, experiences, and/or reactions to care provided
Full Answer
How to make progress notes for substance abuse clients?
Beginning to Make Progress Notes for Substance Abuse Clients Assuming you are writing progress notes as a counselor, you have certain clinical responsibilities. These demands will change from client to client, however you should have a clear working knowledge of the terminology you will use within your discipline.
How do you write a progress note for therapy?
Examples of Therapy Notes Progress notes should include the following as a header or footer, along with the relevant information: Client Name: Date: Number: Medicaid ID: Diagnoses (with DSM5 number/CPT code): Below are some specific examples of therapy notes, and what each might look like as written by a practitioner.
What are group therapy notes for substance abuse treatment?
Group therapy notes. Substance abuse group notes detail the group type, patients present, group leader interventions, appearance and behavior, mental status exam, stage of change, treatment plans and any additional notes. After your sessions, our software will provide you with resources to create an inpatient discharge summary.
What are the demands of writing progress notes as a counselor?
One of the strongest demands will be for organized progress notes. Assuming you are writing progress notes as a counselor, you have certain clinical responsibilities. These demands will change from client to client, however you should have a clear working knowledge of the terminology you will use within your discipline.

How do you write a therapy progress note?
5 Tips for Writing Better Therapy NotesBe Clear & Concise. Therapy notes should be straight to the point but contain enough information to give others a clear picture of what transpired. ... Remain Professional. ... Write for Everyone. ... Use SOAP. ... Focus on Progress & Adjust as Necessary.
How do you write a progress note example?
Progress Notes entries must be:Objective - Consider the facts, having in mind how it will affect the Care Plan of the client involved. ... Concise - Use fewer words to convey the message.Relevant - Get to the point quickly.Well written - Sentence structure, spelling, and legible handwriting is important.
What should a progress note include?
Progress notes can and should be relatively brief, focusing on developments since the previous note, and recapitulating only relevant, ongoing, active problems. Cutting and pasting from previous notes without editing or updating is not permitted, and outdated and redundant information should be eliminated from notes.
How do you develop a treatment plan for substance abuse?
Treatment plans should consider how substance abuse impacts all aspects of your life, including your mental, physical, social, and financial health....Here are the main elements of a treatment plan.Diagnostic Summary. ... Problem List. ... Goals. ... Objectives. ... Interventions. ... Tracking and Evaluating Progress. ... Planning Long-Term Care.
What are the 7 legal requirements of progress notes?
Be clear, legible, concise, contemporaneous, progressive and accurate. Include information about assessments, action taken, outcomes, reassessment processes (if necessary), risks, complications and changes.
What is the most recommended format for documenting progress notes?
SOAPThe SOAP (Subjective, Objective, Assessment and Plan) note is probably the most popular format of progress note and is used in almost all medical settings.
How do I write a daily progress report?
Here are a 4 best practices on writing a daily progress report:Know the Purpose and the Nature of the Daily Progress Report. ... Determine the Organization's Preferred Type of Reporting. ... Add in Some Graphs, Tables, and Charts. ... Ensure That the Report Stays on Topic.
How do you write a good care note?
Care Notes & Reports – Training Course OutlineStructure your notes and reports effectively.Write in a clear, concise style.Avoid common grammatical mistakes.Get your message across clearly and unambiguously.
How do you write a treatment plan example?
Treatment plans usually follow a simple format and typically include the following information:The patient's personal information, psychological history and demographics.A diagnosis of the current mental health problem.High-priority treatment goals.Measurable objectives.A timeline for treatment progress.More items...•
What are some examples of treatment goals?
Treatment Plan Goals and Objectives Examples of goals include: The patient will learn to cope with negative feelings without using substances. The patient will learn how to build positive communication skills. The patient will learn how to express anger towards their spouse in a healthy way.
What are the four steps of treatment planning?
First, the clinician behaviorally defines the counseling problems to be addressed. Second, achievable goals are selected. Third, the modes of treatment and methods of interven- tion are determined. Fourth, the counselor explains how change will be measured and how outcomes will be demonstrated.
Inpatient Substance Abuse Therapy Notes
With our behavioral health EHR software, you'll begin by conducting a series of initial assessments, documenting all your patient's key medical, social and behavioral information. These evaluations include the bio-psychosocial, initial psychiatric and chemical dependency initial nursing assessments.
Outpatient Substance Abuse Progress Notes
Like inpatient evaluations, all outpatient substance abuse therapy notes will begin with numerous assessments, starting with the chemical dependency assessment. This examination outlines six patient risk ratings, such as mental health and treatment acceptance relapse.
Use Our Advanced EHR Software Today
You can solidify and perfect your behavioral health documentation process with ICANotes. Our charting solutions are fast and efficient to help improve your note-taking processes.
When to write therapy notes?
Writing Efficient Therapy Notes. Some therapists write notes during or right after each session, while others need time to decompress before they tackle client notes. Whenever you decide to do your notes, the key to efficiency is knowing what information is important before you start writing.
What are the three main types of progress notes?
There are a lot of different formal approaches to taking progress notes, but the three main types are SOAP notes, BIRP notes, and DAP notes: 1. SOAP notes: SOAP notes are the most common type, containing four separate types of information in four distinct rows: S = Subjective information, such as quotes from the client, ...
What is process notes?
Process notes are sometimes also referred to as psychotherapy notes—they’re the notes you take during or after a session. They tend to be more freeform notes about the session and your impressions of the client’s statements and demeanour. Since these notes often contain highly sensitive information, HIPAA grants them special protection. Unlike progress notes, you’re not legally obligated to release these notes to your client by federal law—although some states may require you to share them if the client asks for them.
How to make note taking more efficient?
One way group therapists make note-taking more efficient is to write a generalized note about the group interaction (with all names in initials), including group interventions planned. Then, you can include this note in each group member’s progress notes.
Why is it important to take notes in therapy?
Good notes improve your ability to recall details between sessions, and avoid repeating past interventions that didn’t work. Bringing details of past sessions into the therapy room also helps you establish trust and rapport with your new clients , as evidence that you’re really listening.
Why is my client frustrated with my ability to write by hand?
S: Client expressed frustration at compromised ability to write by hand due to cerebral palsy. Said, “I feel like I can do more than people give me credit for.” Client is eager to learn new skills and improve motor functions.
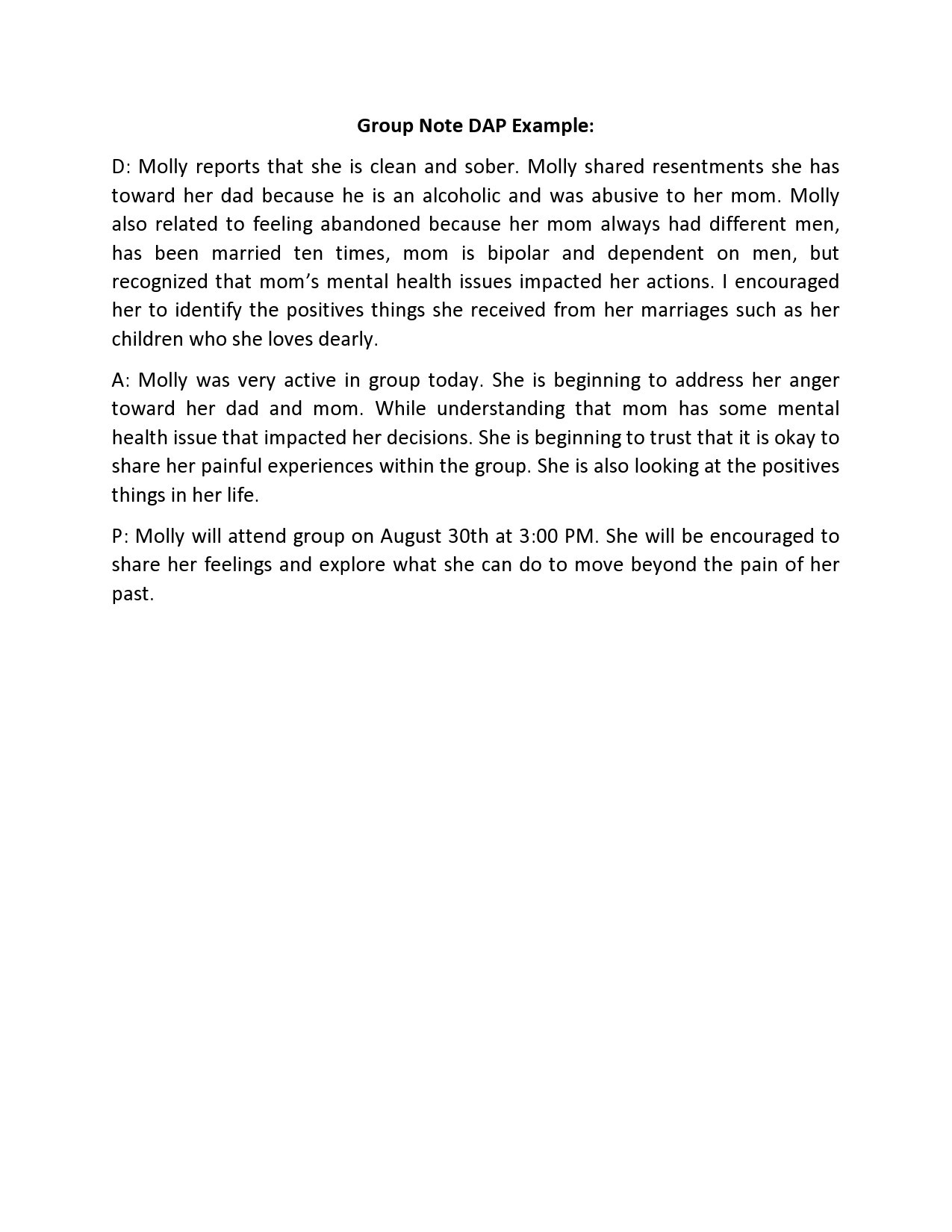
What is a DAP note?
DAP notes: DAP notes are also similar to SOAP notes, except they combine the subjective and objective data categories into one row: D = Subjective and objective data observed in the session (the “S” and “O” sections of SOAP notes combined.
What is progress note in mental health?
What Are Progress Notes in Mental Health? Progress notes are clinical notes made by psychologists, therapists, clinical counselors, psychiatrists, and other practitioners involved in a patient’s treatment and care.
Why are progress notes important in therapy?
They’re instrumental in monitoring a patient’s progress, the efficacy of their treatment, and helping professionals understand their patient’s personal experiences. To be helpful and informative, though, progress notes in mental health need ...
How to integrate subjective data into therapy progress notes?
Another clever way to integrate subjective data into therapy progress notes is by inviting clients to contribute their own notes from sessions.
What is a soap note?
A specific type of progress note, SOAP notes can be shared with any other therapists and care professionals the client may be working with. The four sections of a SOAP method note are: Subjective Data on a patient’s feelings, experiences, or thoughts, such as direct quotes or their observations.
What is assessment information?
Assessment Information that integrates subjective and objective details with a therapist’s professional interpretation, and. Plan details regarding any adjustments or next steps that the counselor and client feel are needed.
Why is a list of frequently used interventions on hand for quick reference useful?
Having a list of frequently-used interventions on hand for quick reference can be particularly useful in multi-provider contexts, helping different practitioners understand what treatments a client is pursuing with other specialists.
Who writes psychotherapy notes?
Also, unlike progress notes, psychotherapy notes are only written by counselors, therapists, and mental health practitioners who are actively involved in their therapy. This table outlines a few more differences between progress and psychotherapy notes. Any care provider involved in a patient’s treatment plan, e.g., Social/Case Workers, GPs.
Why are progress notes important?
Progress notes are vital to good clinical treatment . Counselors often see progress notes as “busywork” and consequently write them in ways that don’t enhance the client’s treatment episode. Carefully documenting the treatment process can be time consuming, and often tedious, but it is critical to quality treatment. The written record supplies the details of how the client utilized their treatment plan. It is similar to drawing a map, in that it charts the client’s journey through the continuum of care.
Why should transitions in treatment always receive the attention of an individual session?
Transitions in treatment should always receive the attention of an individual session (or multiple sessions where indicated) because treatment transitions frequently impact the ultimate success of the treatment as well as lay the groundwork for the next level of treatment. The clinician seeks to discover the client’s views about successes, problems, continued areas of focus, and expectations of future treatment.
What is acceptance through skillful listening?
Individual sessions are the appropriate setting for making sure the treatment is on track. The effective counselor is regularly monitoring the state of the therapeutic alliance. Crucial to this practice is the counselor’s acceptance of the principle that the client’s perception of the relationship is what makes the difference. The attitude underlying this principle might be called “acceptance through skillful listening”. The clinician seeks to understand the client’s feelings and perspectives without judging, criticizing, or blaming. This kind of acceptance of people as they are seems to free them to change, whereas insistent demands to change (“you’re not OK; you have to change”) can have the effect of keeping people as they are. This attitude of acceptance and respect builds a working therapeutic alliance and supports the client’s self-esteem, an important condition for change.
What is a 1:1 session?
Individual sessions (1:1’s) require an awareness of the intimate nature of information being shared (e.g. feelings of ambivalence, relapse, and feeling stuck). These sessions occur at intervals during treatment to assess and monitor the client’s process of change The following five principles of Motivational Interviewing4 are critical clinician skills for facilitating effective individual sessions.
What is therapeutic alliance?
While the presence of genuine empathy, concern, and respect are certainly essential components of a good relationship; they are not the sole components in a successful treatment alliance. A successful treatment alliance hinges on three factors which must be present (along with the qualities known as rapport). These factors are: (1) AGREEMENT ON THE TASKS AND GOALS OF
Why do clients not follow through with their treatment plans?
Try to catch this as early as possible because it may be an indication that the client does not have a “buy-in” on the treatment plan. Or it could be that a new issue has surfaced that is more immediate for the client. Sometimes the client is confused about what they agreed to do and needs additional clarification or help organizing her/his plan.
How are problem statements created?
Problem statements are created as a direct result of the Treatment Assessment. Through the use of the ASAM Six Dimensions, the Treatment Assessment helps the counselor understand where both the client’s strengths and weaknesses lie. The last page of the Treatment Assessment contains the Problem List, which the counselor uses to identify the client’s most immediate areas of need. The Problem List serves as the springboard from which the problem statements on the treatment plan are taken. A good way to check yourself is to compare the completed treatment plan with the last page of the Treatment Assessment; you should find every problem from your treatment plan contained within the Six Dimensions of the Problem List. Make sure you place the problems on the treatment plan in the correct Dimensions.
What are DAP Notes in Counseling?
The acronym “DAP” refers to a professional note-taking framework used by counselors, psychologists, and other healthcare providers in therapy. Used to create progress notes, psychotherapy notes, and other practice documents, the DAP format offers an organized, efficient way for practitioners to track their clients’ progress.
DAP vs SOAP Therapy Notes Explained
The SOAP acronym is another popular therapy note framework used in mental healthcare settings, with a slightly different layout to DAP notes.
2 Examples of DAP Progress Notes
Here are two examples of DAP Progress Notes in counseling, to paint a clearer picture.
How To Write DAP Case Notes: 7 Tips
DAP notes are simple to write with the right digital templates – here are our tips on formatting the perfect note and recording group sessions in Quenza.
3 Helpful Templates For Your Sessions
If you’re looking for a few DAP note templates to help you get started, some of the following might interest you:
Best Online Solution For Writing DAP Notes
The most efficient, effective way to create DAP notes as a mental healthcare provider is to use specialized software, a HIPAA-compliant software solution, to be precise.
6 Unique Features Included in Quenza
If you’re a general or mental healthcare professional, there are more than a few ways Quenza can help you in addition to writing clear, accurate DAP notes efficiently.