Part 3 Creating the Treatment Plan Download Article
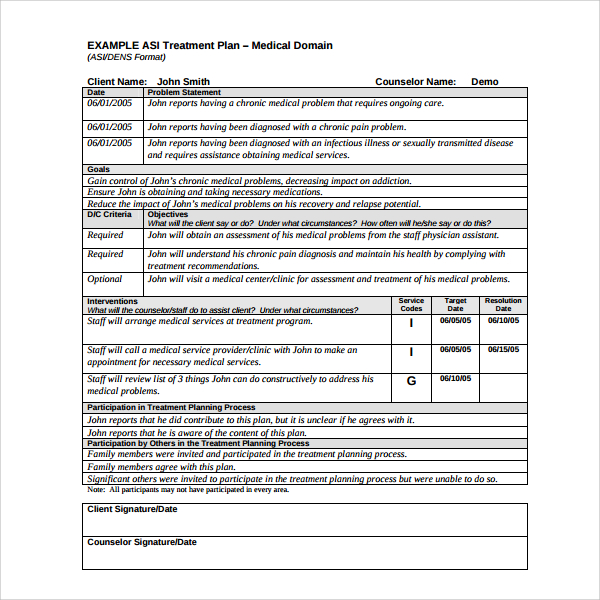
- Record the treatment plan's components. The treatment plan will consist of the goals that the counselor and therapist has decided on.
- Record the goals. Your goals need to be as clear and concise as possible. ...
- Express specific interventions you will use. ...
- Sign the treatment plan. ...
- Review and improve as needed. ...
- The patient's personal information, psychological history and demographics.
- A diagnosis of the current mental health problem.
- High-priority treatment goals.
- Measurable objectives.
- A timeline for treatment progress.
How do I write a treatment plan?
When you write a treatment plan be sure to use these four steps: The behavioral definitions, also known as “problem statements,” are based on the information that was collected from the biopsychosocial assessment. This assessment should few brief sentences outlining your clients' condition (s) for which they are seeking treatment.
What is a sample treatment plan for Medicaid?
This sample treatment plan is for a young Medicaid recipient struggling with symptoms of depression and suicidal thoughts. This treatment plan is written for the treatment of a man suffering from schizoaffective disorder who is experiencing side effects from his medication.
What is a treatment plan as a living document?
The idea is that the treatment plan is treated as a living document, updated regularly throughout the course of treatment, as the client improves and meets target dates on his or her treatment plan.
How is a diagnosis made in a treatment plan?
All diagnoses must be made before a treatment plan can be completed. A diagnosis is chosen based on the client's symptoms and how they fit with the criteria outlined in the DSM. The DSM is the diagnostic classification system created by the American Psychiatric Association (APA).
What is a medical treatment plan?
A detailed plan with information about a patient's disease, the goal of treatment, the treatment options for the disease and possible side effects, and the expected length of treatment.
What should a treatment plan include?
A treatment plan will include the patient or client's personal information, the diagnosis (or diagnoses, as is often the case with mental illness), a general outline of the treatment prescribed, and space to measure outcomes as the client progresses through treatment.
What are the four components of the treatment plan?
There are four necessary steps to creating an appropriate substance abuse treatment plan: identifying the problem statements, creating goals, defining objectives to reach those goals, and establishing interventions.
What is a treatment plan template?
A treatment plan is a detailed plan tailored to the individual patient and is a powerful tool for engaging the patient in their treatment. Treatment plans usually follow a simple format and typically include the following information: The patient's personal information, psychological history, and demographics.
How do you write a treatment?
The point of writing a film treatment is to:Set up the world you want the reader to envision.Lay out the structure of your whole story.Help you identify plot holes, or parts of the film you're missing.Flesh-out characters and figure out the importance of each role.More items...•
How do you write a treatment summary?
How To Write A Therapy Case Summary1 | Therapy Case History. ... 2 | Systemic Client Assessment. ... 3 | Treatment Focus and Progress. ... 4 | Client Strengths and Supports. ... 5 | Evaluation.
What is a smart treatment plan?
S.M.A.R.T. Treatment Planning The treatment plan addresses problems identified in the client assessment, defines and measures interventions in their care and provides a measure for client's progress in treatment.
What are interventions in a treatment plan?
Interventions are what you do to help the patient complete the objective. Interventions also are measurable and objective. There should be at least one intervention for every objective. If the patient does not complete the objective, then new interventions should be added to the plan.
What are the four goals of treatment?
The Four Goals of Drug TherapyIdentifying Drug Use and Problem Behavior. One of the hardest goals is also one of the most important, knowing what to look for when you have concerns about someone's drug use. ... Intervention and Detox. ... Drug Therapy and Treatment Completion. ... Work To Avoid Relapse.
What should happen before the treatment plan is implemented?
1. Preclinical exam—Before the examination begins, it is important that the dentist or team member conducts a preclinical exam to understand why the patient is there, past experiences, desired changes, any problems occurring, and more. 2.
What is a treatment plan and why is it important?
A treatment plan is a document that identifies problems you want to work on in therapy, what your goals for these problems are, and steps you can take to work towards accomplishing these goals.
What are the steps needed to develop a systematic treatment plan for a client?
These domains include: (1) patient predisposing qualities, (2) treatment context, (3) relationship variables, and (4) intervention selection. These main principles provide the basis for which guidelines have been developed to systematically individualize treatment plans.
Who is responsible for writing the medical assessment and plan?
The treatment plan must lay out the route the patient is to take on their own to care for the issue diagnosed. The clinician is responsible for writing the medical assessment and plan as well as directing the patient toward appropriate treatment.
What do medical students need to know?
Medical students must learn to write medical assessment and appropriate treatment plans. This is a skill they will use throughout their medical careers. The assessment must be concise and define the issue. The treatment plan must lay out the route the patient is to take on their own to care for the issue diagnosed.
SHOW-NOTES (transcript)
Hi, Patrick Martin here, and in this post I will be sharing with you how to create a CBT treatment plan and this is the second part of the clinical loop.
Create A Treatment Plan Using The S.M.A.R.T. Model
Alright, another acronym that can help us out complements the smart model, and this is known as the P.O.W.E.R. model.
Final Thoughts On Creating A Treatment Plan
So, when it comes to making measurable goals right, those objectives we can use some tools and counseling to help us do that.
What is a mental health treatment plan?
At the most basic level, a mental health treatment plan is simply a set of written instructions and records relating to the treatment of an ailment or illness. A treatment plan will include the patient or client’s personal information, the diagnosis (or diagnoses, as is often the case with mental illness), a general outline ...
Why do we need treatment plans?
Treatment plans can reduce the risk of fraud, waste, abuse, and the potential to cause unintentional harm to clients. Treatment plans facilitate easy and effective billing since all services rendered are documented.
What is the treatment contract?
Treatment Contract – the contract between the therapist and client that summarizes the goals of treatment. Responsibility – a section on who is responsible for which components of treatment (client will be responsible for many, the therapist for others)
What is the part of effective mental health?
Part of effective mental health treatment is the development of a treatment plan. A good mental health professional will work collaboratively with the client to construct a treatment plan that has achievable goals that provide the best chances of treatment success. Read on to learn more about mental health treatment plans, how they are constructed, ...
What is intervention in therapy?
Interventions – the techniques, exercises, interventions, etc., that will be applied in order to work toward each goal. Progress/Outcomes – a good treatment plan must include space for tracking progress towards objectives and goals (Hansen, 1996)
What is blended care in therapy?
Blended care involves the provision of psychological services using telecommunication technologies.
What is a goal in counseling?
Goals are the broadest category of achievement that clients in mental health counseling work towards. For instance, a common goal for those struggling with substance abuse may be to quit using their drug of choice or alcohol, while a patient struggling with depression may set a goal to reduce their suicidal thoughts.
How to obtain information needed to complete a treatment plan?
To obtain the information needed to complete a treatment plan, a mental health worker must interview the client. The information gathered during the interview is used to write the treatment plan. Steps.
What should a treatment plan include?
A treatment plan should include direct input from the client. The counselor and client decide, together, what goals should be included in the treatment plan and the strategies that will be used to reach them. Ask the client what he would like to work on in treatment.
How long does it take for a client to heal from depression?
Long term goal (such as client stating, “I want to heal my depression.”) Short terms goals or objectives (Client will reduce depression severity from 8/10 to 5/10 within six months). A good treatment plan will have at least three goals.
What information is needed for a treatment plan?
A basic treatment plan will have the following information: Name of client and diagnosis.
What is a mental health treatment plan?
A mental health treatment plan is a document that details a client's current mental health problems and outlines the goals and strategies that will assist the client in overcoming mental health issues. To obtain the information needed to complete a treatment plan, a mental health worker must interview ...
What can a mental health worker consult during evaluation?
The mental health worker may also consult a client's medical and mental health records during the evaluation process. Make sure appropriate releases of information (ROI documents) have been signed. Make sure you also appropriately explain the limits to confidentiality.
What are some examples of mental health assessments?
An example of sections for a mental health assessment include (in order): Reason for referral.
What is a mental health treatment plan?
Mental health treatment plans are versatile, multi-faceted documents that allow mental health care practitioners and those they are treating to design and monitor therapeutic treatment. These plans are typically used by psychiatrists, psychologists, professional counselors, therapists, and social workers in most levels of care.
Why are treatment plans important?
Treatment plans are important for mental health care for a number of reasons: Treatment plans can provide a guide to how services may best be delivered. Professionals who do not rely on treatment plans may be at risk for fraud, waste, and abuse, and they could potentially cause harm to people in therapy.
What is HIPAA treatment plan?
Treatment Plans and HIPAA. The Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule grants consumers and people in treatment various privacy rights as they relate to consumer health information, including mental health information.
Why do people need treatment plans?
Treatment plans can also be applied to help individuals work through addictions, relationship problems, or other emotional concerns. While treatment plans can prove beneficial for a variety of individuals, they may be most likely to be used when the person in therapy is using insurance to cover their therapy fee.
Do you need a treatment plan for a 3rd party?
Treatment plans are required if you accept 3rd party reimbursement and are just good practice. They are a road map to treatment. They are fluid and are developed with the client/patient. Pretty much necessary if you are doing your job as a therapist.
Do MCOs require treatment plans?
Some commercial insurances and most managed care organizations (MCOs) require that treatment plans be completed for every person in treatment. MCOs offer specific guidelines regarding what should go into a treatment plan and how frequently plans should be updated and reviewed.
Do you avoid writing treatment plans?
Maybe you don’t see them as helpful, or don’t feel you have time, so you don’t write them? Well, you’re not alone — it seems like a large number of therapists I consult with don’t write treatment plans for their clients. But this is something that you might want to rethink.
Start treatment plans in session with 5 questions you can ask your client
Near the end of the intake session, grab your pen (or tablet or laptop) and tell your client you want to be sure that they get what they need from these sessions. Help identify goals with questions like these:
Where practitioners turn into entrepreneurs
Pollen Magazine examines the health and wellness industry through the lens of the professionals that are redefining private practice. Find inspiration, learn from others, and discover insights on how to build the best version of your practice.
Why do clients not follow through with their treatment plans?
Try to catch this as early as possible because it may be an indication that the client does not have a “buy-in” on the treatment plan. Or it could be that a new issue has surfaced that is more immediate for the client. Sometimes the client is confused about what they agreed to do and needs additional clarification or help organizing her/his plan.
What is therapeutic alliance?
While the presence of genuine empathy, concern, and respect are certainly essential components of a good relationship; they are not the sole components in a successful treatment alliance. A successful treatment alliance hinges on three factors which must be present (along with the qualities known as rapport). These factors are: (1) AGREEMENT ON THE TASKS AND GOALS OF
What is the point of contact between a counselor and client?
There are many points of contact that occur between a counselor and client over a treatment episode. Each of those contacts has the potential to provide the clinician with valuable information regarding that client and their specific treatment. If the counselor is aware of that valuable information and seeks to take advantage of those contacts they must rely on their interviewing skills to obtain that valuable information.
Why should transitions in treatment always receive the attention of an individual session?
Transitions in treatment should always receive the attention of an individual session (or multiple sessions where indicated) because treatment transitions frequently impact the ultimate success of the treatment as well as lay the groundwork for the next level of treatment. The clinician seeks to discover the client’s views about successes, problems, continued areas of focus, and expectations of future treatment.
What makes a good clinician?
Through school and work we have all been taught which qualities make a good clinician. Empathy, genuineness, respect, warmth, immediacy, concreteness, potency, and self-actualization are just a few. Understanding, transparency, tolerance, patience, and skillful validation are other important qualities, along with being flexible, curious, and open-minded. And don’t forget the various listening skills, such as clarification, paraphrasing, and reflection. It seems like a lot, and yet these skills are essential to creating an alliance (a partnership or bond) between yourself and your client.
How many goals should a substance abuse treatment plan have?
Typically, a well-written substance abuse treatment plan will have two to three goals to accomplish while in treatment. Unless the treatment stay is short, such as in detox facilities. Keep in mind that along with each goal, you need to write an objective that defines what the patient will do to accomplish the goal, as well as intervention, ...
What is an objective guideline?
A general guideline is that if you cannot actually see the client do something, then it's a goal. A good example of this is patients improving their lives. You can't see that. If you can see the client do something, such as learn new coping strategies, then it is an objective.
What are the steps of EMR?
When you write a treatment plan be sure to use these four steps: Identifying the behavioral definitions/problem statements. Goals.
Is a treatment plan a living document?
It's important for you to remember that once the treatment plan is written it doesn’t end there. The idea is that the treatment plan is treated as a living document, updated regularly throughout the course of treatment, as the client improves and meets target dates on his or her treatment plan.