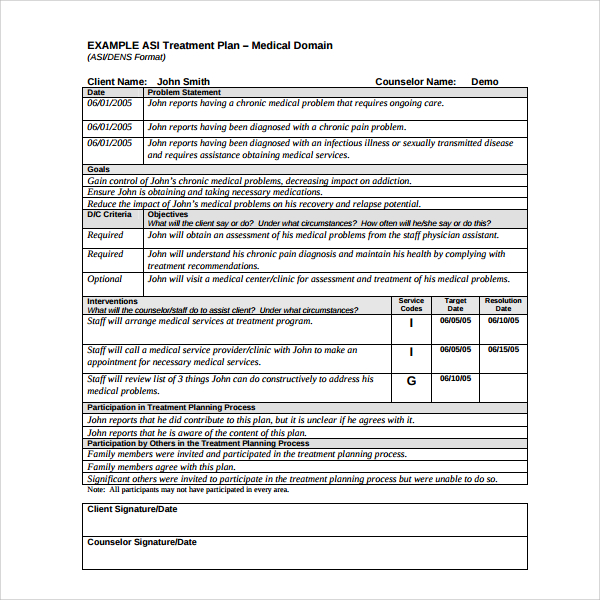
- Record the treatment plan's components. The treatment plan will consist of the goals that the counselor and therapist has decided on.
- Record the goals. Your goals need to be as clear and concise as possible. Remember the SMART goals plan and make each goal specific, measurable, achievable, realistic, and time-limited.
- Express specific interventions you will use. The counselor will include treatment strategies the client has agreed to.
- Sign the treatment plan. Both the client and the counselor sign the treatment plan to show that there is an agreement on what to focus on in treatment.
- Review and improve as needed. You will be expected to complete goals and make new ones as the client progresses in treatment.
How do you write a treatment plan?
The doctor will properly diagnose, recommend, and deliver a treatment plan while you sit in the comfort of your own home. You’ll also have access to your doctor via the online messaging portal which gives you the ability to contact your doctor on your schedule, plus access to Keep’s care consultants in case you have any questions along the way.
How to write measurable goals in counseling?
and deals. Choose the type, level, urgency, and length to start off. Your preferred How To Write Measurable Goals In Counseling writer will begin writing the paper. Offer revision suggestions when you receive the paper and download the completed paper in time to submit it to your school!
What is the purpose of a treatment plan?
Treatment planning is a process that involves multiple steps:
- identification of the problem and the most important issues
- specific definition of the issues
- development of measurable short- and long-term goals
- creation of the interventions that will help reach the goals
How to write treatment goal?
TREATMENT PLAN GOALS / OBJECTIVES. Note: Always make objectives measurable, e.g., 3 out of 5. times, 100%, learn 3 skills, etc., unless they are . measurable on their own as in “ List . and discuss [issue] weekly… ” Abuse/Neglect. Goal: Explore and resolve issues relating to history of abuse/neglect victimization

What are examples of achievable mental health goals?
The first thing to remember in setting your personal goals to improve your mental health is you should not be so hard on yourself. Progress is grad...
What should you expect in your first counseling session?
On your first day of counseling, you don’t just jump right off and start it right away. Your first session is the time for formalities. That said,...
What are the various types of counseling?
Aside from counseling for mental health problems, there are also other types of counseling services. One example is career counseling. In this type...
How to obtain information needed to complete a treatment plan?
To obtain the information needed to complete a treatment plan, a mental health worker must interview the client. The information gathered during the interview is used to write the treatment plan. Steps.
Why do counselors sign a treatment plan?
Sign the treatment plan. Both the client and the counselor sign the treatment plan to show that there is an agreement on what to focus on in treatment.
What is psychosocial evaluation?
A psychosocial evaluation can also examine past and current substance abuse problems as well as any psychiatric drugs the client has used or is currently on.
What is a mental health treatment plan?
A mental health treatment plan is a document that details a client's current mental health problems and outlines the goals and strategies that will assist the client in overcoming mental health issues. To obtain the information needed to complete a treatment plan, a mental health worker must interview ...
How to be ethical in therapy?
Make sure you stick to what you know. Part of being an ethical therapist is about doing what you are competent in so that you do not cause harm to the client. Don’t try to attempt a therapy you are not trained in unless you have plenty of clinical supervision with an expert.
What to do if patient raises concerns?
If the patient raises these concerns, stop the assessment and follow crisis intervention procedures.
What are some examples of mental health assessments?
An example of sections for a mental health assessment include (in order): Reason for referral.
What is a counseling treatment plan?
A counseling treatment plan is a document that counselors write to list their recommended methods and activities that will be most effective in the progress of the therapy. Counselors incorporate this treatment plan based on their records.
How to keep your treatment plan instructive?
To keep your treatment plan as instructive as possible, you need to pay attention and consider the necessary components of psychotherapy. 1. Refer to Your Therapy Notes. It is a counselor’s responsibility to take down necessary information every session.
What is career counseling?
In this type, the counselor will conduct a career assessment to help the client realize the career development plan is most suitable for their condition.
What is the job of a mental health counselor?
As a professional in this practice, it is your job to offer counseling sessions. Your aim should be to help these people discover ways to respond to their mental health problems. That said, to achieve the goals, the counselor needs to compose an effective counseling treatment plan .
How to improve mental health?
The first thing to remember in setting your personal goals to improve your mental health is you should not be so hard on yourself. Progress is gradual so ensure to set SMART goals. Examples of these goals include practicing to love yourself and your body and seeking support from the people you trust. In addition, you can also aim to establish boundaries with people and find methods to deal with stress.
What to do on the first day of counseling?
On your first day of counseling, you don’t just jump right off and start it right away. Your first session is the time for formalities. That said, it is when you should answer and sign several paper works. After doing so, the procedure is to get to know your therapist and talk about the estimated cost of the fees you need to pay in each session.
What is the importance of an evaluation summary report?
People are different from each other. They have experiences and perceptions about things. That said, even when clients end up with a similar diagnosis, they suffer from conditions unique to each other. In dealing with each of them, you need to analyze to pinpoint what they are experiencing. Writing an evaluation summary report may be helpful in this step.
What is a mental health treatment plan?
At the most basic level, a mental health treatment plan is simply a set of written instructions and records relating to the treatment of an ailment or illness. A treatment plan will include the patient or client’s personal information, the diagnosis (or diagnoses, as is often the case with mental illness), a general outline ...
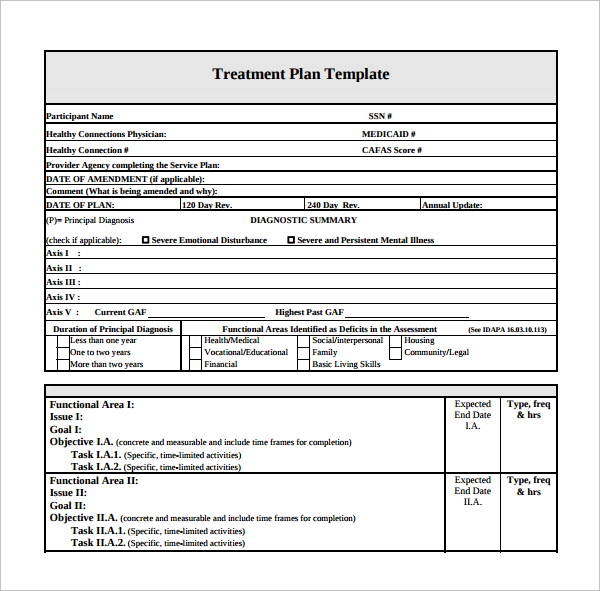
What are the sections of a treatment plan checklist?
The checklist breaks down treatment plans into five sections: Problem Statements, Goals, Objectives, Interventions, and General Checklist.
What is the treatment contract?
Treatment Contract – the contract between the therapist and client that summarizes the goals of treatment. Responsibility – a section on who is responsible for which components of treatment (client will be responsible for many, the therapist for others)
Why do we need treatment plans?
Treatment plans can reduce the risk of fraud, waste, abuse, and the potential to cause unintentional harm to clients. Treatment plans facilitate easy and effective billing since all services rendered are documented.
What is the part of effective mental health?
Part of effective mental health treatment is the development of a treatment plan. A good mental health professional will work collaboratively with the client to construct a treatment plan that has achievable goals that provide the best chances of treatment success. Read on to learn more about mental health treatment plans, how they are constructed, ...
What is intervention in therapy?
Interventions – the techniques, exercises, interventions, etc., that will be applied in order to work toward each goal. Progress/Outcomes – a good treatment plan must include space for tracking progress towards objectives and goals (Hansen, 1996)
What is blended care in therapy?
Blended care involves the provision of psychological services using telecommunication technologies.
What is a treatment plan?
A treatment plan is a detailed plan tailored to the individual patient and is a powerful tool for engaging the patient in their treatment. Treatment plans usually follow a simple format and typically include the following information: The patient’s personal information, psychological history and demographics.
How does a mental health treatment plan complement other therapy notes?
A treatment plan is a tool that promotes good communication between staff members and helps provide documentation necessary for billing.
What is the goal of a mental health treatment plan?
Both parties work together to create a shared vision and set attainable goals and objectives. A goal is a general statement of what the patient wishes to accomplish .
What happens if you don't have a treatment plan?
Without a treatment plan, a patient has no clear direction on how to improve behaviors, negative thinking patterns, and other problems impacting their lives.
How to evaluate the effectiveness of a treatment plan?
To evaluate the effectiveness of the treatment plan, you need to keep score of how the patient is doing. Ask the patient to count and keep track of their thoughts, feelings and behaviors in a log so you can monitor their progress.
What is a comprehensive treatment plan?
When a mental health professional creates a comprehensive treatment plan specially designed to meet their patient’s needs, they give their patient directions towards growth and healing.
When is a discharge summary needed?
When patients are ready to leave a treatment program, a discharge summary is needed to document how the patient completed treatment and what their plan for continuing care is. A treatment plan can guide the writing process when it’s time to produce an accurate, detailed discharge summary.
What is a mental health treatment plan?
Mental health treatment plans are versatile, multi-faceted documents that allow mental health care practitioners and those they are treating to design and monitor therapeutic treatment. These plans are typically used by psychiatrists, psychologists, professional counselors, therapists, and social workers in most levels of care.
Why are treatment plans important?
Treatment plans are important for mental health care for a number of reasons: Treatment plans can provide a guide to how services may best be delivered. Professionals who do not rely on treatment plans may be at risk for fraud, waste, and abuse, and they could potentially cause harm to people in therapy.
What is HIPAA treatment plan?
Treatment Plans and HIPAA. The Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule grants consumers and people in treatment various privacy rights as they relate to consumer health information, including mental health information.
What does a therapist do for Chris?
Therapist will provide psychoeducation on positive parenting and will support Chris in developing a concrete parenting plan. Therapist will provide materials for Chris to document the new house rules, rewards, and consequences system.
Why do people need treatment plans?
Treatment plans can also be applied to help individuals work through addictions, relationship problems, or other emotional concerns. While treatment plans can prove beneficial for a variety of individuals, they may be most likely to be used when the person in therapy is using insurance to cover their therapy fee.
What is the principle of evidence based medicine?
The number one principle of evidence based medicine is that each disease, condition, or symptom is treated with the MOST EFFECTIVE treatment available (as identified by science). The essence of a treatment plan is a fundamental assumption that everyone will be treated differently. If everyone is treated differently, then only one person, at most, is receiving the best treatment.
What is progress and outcomes?
Progress and outcomes of the work are typically documented under each goal. When the treatment plan is reviewed, the progress sections summarize how things are going within and outside of sessions. This portion of the treatment plan will often intersect with clinical progress notes.
What information does a counselor need to fill out for a treatment plan?
Patient information: At the top of the treatment plan, the counselor will fill in information such as the patient’s name, social security number, insurance details, and the date of the plan.
How do mental health professionals use treatment plans?
Psychiatrists, psychologists, counselors, social workers, and other health professionals use treatment planning as a tool to effectively treat patients and clients. Without a clear plan in place, it can be hard to track progress, stay organized and keep a record of individual patient care. We understand that every person who enters our intensive outpatient programs is unique. Our experienced clinicians will work with patients to develop a comprehensive treatment plan using evidence-based methods. When health professionals create a comprehensive treatment plan specially designed to meet their patients’/clients’ needs, they give their patients directions towards growth and healing. Although not all mental health professionals are required to produce treatment plans, it’s a beneficial practice for the patient. In this article, we’ll show you why treatment plans are essential and how to create treatment plans that will make a difference in your and your patient’s lives. Each patient must have an individualized, goal and action-oriented treatment plan that is based upon information obtained in the assessment process .
What is treatment planning?
Treatment planning is a team effort between the patient and health specialist. Both parties work together to create a shared vision and set attainable goals and objectives.
What is a goal in a patient's life?
Both parties work together to create a shared vision and set attainable goals and objectives. A goal is a general statement of what the patient wishes to accomplish. Examples of goals include: The patient will learn to cope with negative feelings without using substances.
What is the third section of a treatment plan?
Problems and goals: The third section of the treatment plan will include issues, goals, and a few measurable objectives. Each issue area will also include a time frame for reaching goals and completing objectives. Counselors should strive to have at least three goals.
What is the role of model and technique in a treatment plan?
Treatment plans provide structure patients need to change. Model and technique factors account for 15 percent of a change in therapy. Research shows that focus and structure are critical parts of positive therapy outcomes. Goal-setting as part of a treatment plan is beneficial in itself. Setting goals helps patients:
What is the objective of a recovery program?
A patient in a recovery program might have the objective to keep a daily assertiveness log with the goal to learn healthy communication skills.
Do you avoid writing treatment plans?
Maybe you don’t see them as helpful, or don’t feel you have time, so you don’t write them? Well, you’re not alone — it seems like a large number of therapists I consult with don’t write treatment plans for their clients. But this is something that you might want to rethink.
Start treatment plans in session with 5 questions you can ask your client
Near the end of the intake session, grab your pen (or tablet or laptop) and tell your client you want to be sure that they get what they need from these sessions. Help identify goals with questions like these:
Where practitioners turn into entrepreneurs
Pollen Magazine examines the health and wellness industry through the lens of the professionals that are redefining private practice. Find inspiration, learn from others, and discover insights on how to build the best version of your practice.
Why do clients not follow through with their treatment plans?
Try to catch this as early as possible because it may be an indication that the client does not have a “buy-in” on the treatment plan. Or it could be that a new issue has surfaced that is more immediate for the client. Sometimes the client is confused about what they agreed to do and needs additional clarification or help organizing her/his plan.
What is the point of contact between a counselor and client?
There are many points of contact that occur between a counselor and client over a treatment episode. Each of those contacts has the potential to provide the clinician with valuable information regarding that client and their specific treatment. If the counselor is aware of that valuable information and seeks to take advantage of those contacts they must rely on their interviewing skills to obtain that valuable information.
What is therapeutic alliance?
While the presence of genuine empathy, concern, and respect are certainly essential components of a good relationship; they are not the sole components in a successful treatment alliance. A successful treatment alliance hinges on three factors which must be present (along with the qualities known as rapport). These factors are: (1) AGREEMENT ON THE TASKS AND GOALS OF
What is the role of a counselor in a relationship?
Not only does this communicate to the client that you are interested in their experience, it also helps you make adjustments to their perception of the relationship and stay aligned with them.
What makes a good clinician?
Through school and work we have all been taught which qualities make a good clinician. Empathy, genuineness, respect, warmth, immediacy, concreteness, potency, and self-actualization are just a few. Understanding, transparency, tolerance, patience, and skillful validation are other important qualities, along with being flexible, curious, and open-minded. And don’t forget the various listening skills, such as clarification, paraphrasing, and reflection. It seems like a lot, and yet these skills are essential to creating an alliance (a partnership or bond) between yourself and your client.
Why should transitions in treatment always receive the attention of an individual session?
Transitions in treatment should always receive the attention of an individual session (or multiple sessions where indicated) because treatment transitions frequently impact the ultimate success of the treatment as well as lay the groundwork for the next level of treatment. The clinician seeks to discover the client’s views about successes, problems, continued areas of focus, and expectations of future treatment.
What is acceptance through skillful listening?
Individual sessions are the appropriate setting for making sure the treatment is on track. The effective counselor is regularly monitoring the state of the therapeutic alliance. Crucial to this practice is the counselor’s acceptance of the principle that the client’s perception of the relationship is what makes the difference. The attitude underlying this principle might be called “acceptance through skillful listening”. The clinician seeks to understand the client’s feelings and perspectives without judging, criticizing, or blaming. This kind of acceptance of people as they are seems to free them to change, whereas insistent demands to change (“you’re not OK; you have to change”) can have the effect of keeping people as they are. This attitude of acceptance and respect builds a working therapeutic alliance and supports the client’s self-esteem, an important condition for change.