What is the best treatment for TMJ?
1. Physical Activity...
2. Cashew...
3. Walnuts...
4. Apply Warm Or Cold Therapy...
5. TMJ Treatment Due To Multiple Teeth Grinding...
6. TMJ Treatment Due To Osteoarthritis...
7. TMJ Treatment Due To Injury...
8. TMJ Treatment Due To Rheumatism...
Learn More...What is TMJ and what can I do for it?
Treatments You Can Try at Home
- Eat soft foods. Jaw pain can be exacerbated by a lot of chewing or biting on hard or chewy foods. ...
- Relax your jaw. This can be easier said than done. If you hold tension in your jaw when you feel stress, it can make TMJ/TMD worse.
- Take a pain reliever. Over-the-counter pain relievers can help with the pain. ...
Does physical therapy help TMJ?
What Temporomandibular Joint (TMJ) Exercises Relieve Pain?
- Exercises for TMJ pain relief. It’s unclear exactly how TMJ exercises may relieve pain. ...
- Tips for relieving pain during dental care. If you have TMJ, it may be painful to practice basic oral hygiene. ...
- The bottom line. In some cases, TMJ disorders go away on their own. If your symptoms persist, TMJ exercises may help bring pain relief.
How to perform a TMJ massage to relieve jaw pain?
Your physical therapist will teach you exercises that don’t exert a lot of pressure on your TMJ but can strengthen the jaw muscles and restore more natural, pain-free motion. If your pain is severe, your physical therapist may use treatments such as electrical stimulation or ultrasound in addition to manual therapy to reduce your pain.
What causes TMJ degeneration?
There is no single cause for the development of TMJ osteoarthritis and several risk factors tend to contribute to the disease. A main risk factor for TMJ osteoarthritis is repetitive movement of the jaw, such as teeth grinding, jaw clenching or gum chewing over a long period of time.
What is degenerative changes in the temporomandibular joint?
Degenerative changes in the TMJ bone components include erosion, flattening, sclerosis, subchondral cysts, and osteophytes. The joint space also decreases as a result of the loss of the joint cartilage tissue [3]. Knowledge of these bone changes is fundamental for the diagnosis of dysfunctions associated with TMD [12].
Can temporomandibular joint dysfunction be cured?
Unfortunately, there is no cure for arthritis. This means that for anyone suffering from TMJ due to arthritis, there's also no cure for the TMJ disorder. An eroded disk or a connective tissue disease may similarly have no cure.
Can the TMJ joint be repaired?
Surgery can be used to treat a TMJ disorder if more conservative treatments, such as oral splints or mouthguards, don't help to reduce the severity of your symptoms. For some people, surgery may be necessary to restore full use of their TMJ.
Can TMJ cause degenerative disc disease?
Dysfunction of the TMJ is a common cause of pain and disability and can have multiple underlying causes (including injury and arthritis). Changes in the TMJ disc (such as disc thinning) are an early sign of TMJ degeneration and dysfunction.
Can Botox help TMJ pain?
Botox can help relax the muscles in your jaw Botox for TMJ can be highly effective. One 2012 study found that Botox treatments significantly decreased pain and increased mouth movements for three months following the treatment. Another study found that symptoms improved in 90 percent of participants.
What is the best medication for TMJ?
The best medicines for TMJ pain are over-the-counter painkillers and anti-inflammatories, such as Tylenol and ibuprofen. In some extreme circumstances, a dentist may prescribe something stronger, but even then it's likely to be a prescription ibuprofen, not opioid painkiller.
How can I fix my TMJ myself?
Here are eight ways you can help relieve pain in your TMJ and manage symptoms without surgery:Maintain the resting position of your jaw. ... Correct your posture. ... Get a good night's sleep. ... Use a hot or cold compress. ... Reduce stress. ... Exercise your jaw. ... Take notice of bad habits. ... Avoid certain activities and foods.
What is the best doctor to see for TMJ?
Most often, a dentist who specializes in TMJ disorders is actually your best choice. There are multiple forms of TMJ disorder treatment. Fortunately, dental specialists like Dr. Phillips have specialized knowledge of the jaw and the temporomandibular joint and can prescribe the correct treatment.
Is surgery necessary for TMJ?
TMJ surgery, including TMJ reconstruction surgery, may be recommended to correct your TMJ disorder if you experience: TMJ locking—the inability to fully open or close your mouth. Continuous facial pain and/or TMJ dysfunction—despite having trialled non-surgical therapies for at least six months.
What happens if TMJ doesn't go away?
Decreased Quality of Life. With untreated TMJ, you will experience all types of painful symptoms that can have a huge impact on your quality of life. Your frequent headaches and constant pain can cause you to call out of work more often, turn down social obligations, and spend most of your time feeling miserable in bed ...
Is jaw surgery for TMJ worth it?
Corrective jaw surgery can improve regular functions such as breathing, speaking and chewing. With your jaw in proper alignment, pains associated with TMJ disorders may be believed. Chronic jaw joint pain, headaches, a locking jaw, and an open bite are just a few maladies that can be remedied with jaw surgery.
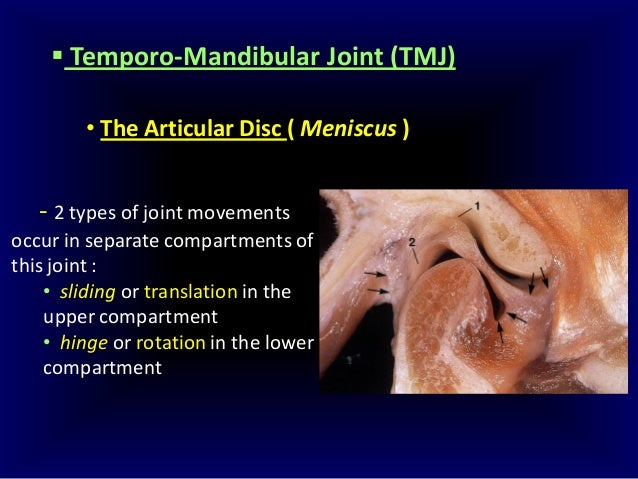
What bone will touch the temporal bone?
In simpler terms, the top of the lower jawbone —the mandibular condyle—will touch the temporal bone. Put those two bones in contact long enough and they will appear to be wearing away. X-ray of normal. X-ray of total disc displacement. X-ray of degenerative arthritis, no disc.
What happens when the articular disc is displaced long enough?
When the articular disc is displaced long enough, it will eventually perforate or more likely fragment. When this occurs, the mandibular condyle will contact the inferior surface of the glenoid fossa. In simpler terms, the top of the lower jawbone—the mandibular condyle—will touch the temporal bone.
Can bone degeneration reverse?
The degeneration that has occurred will not reverse; in other words, the lost bone cannot be expected to grow back*. But you should be able to stop the degeneration from worsening.
What is TMJ degenerative disorder?
Degenerative disorders of the temporomandibular joint: etiology, diagnosis, and treatment. Temporomandibular joint (TMJ) disorders have complex and sometimes controversial etiologies. Also, under similar circumstances, one person's TMJ may appear to deteriorate, while another's does not.
Can TMJ deteriorate?
Also, under similar circumstances, one person's TMJ may appear to deteriorate, while another's does not. However, once degenerative changes start in the TMJ, this pathology can be crippling, leading to a variety of morphological and functional deformities.
What is the therapy for TMJ?
For the TMJ this means eating softer foods, taking smaller bites, and chewing more slowly during periods of increased symptoms.
Why is education important for TMJ?
The goals of therapy are reduction of stress on the TMJ, maintenance of function, and reduction of pain.
What is the joint closest to the face?
Degenerative arthritis or as it is referred to now, Osteoarthritis (OA) can effect any joint in the body and the joint closest to the face is the temporomandibular joint (TMJ), so I will assume that you are referring to arthritis in the TMJ.
What do dentists use to combat bites?
Since these are activities that people are not normally conscious of, it can be difficult to develop direct ways to combat them. Dentists commonly use orthotics (i.e. splints, bite planes, or bite guards) which reduce these habits to some extent.
Is biting your fingers bad for your jaw?
But parafunctional activities of the jaw — that is clenching and grinding the teeth, biting your fingernails or lips, and biting pencils or pens — are considered to be much more detrimental than functional activities such as chewing.
Can OA cause TMJ pain?
You should also be aware that OA might be used by doctors in a general sense to suggest any condition that affects the bony integrity of a joint. Therefore, it is prudent to rule out other conditions, which might be causing pain in the TMJ.
Does PT help with TMJ?
They have also been shown to have a relaxing effect on the muscles of the jaw thus reducing strain on the TMJ. Physical therapy ( PT) is quite useful in improving any limited range of motion of the mandible, improving function and reducing pain.
Which joints are most affected by osteoarthritis?
Osteoarthritis can also affect other joints in the body such as wrist, shoulder, ankle and Temporomandibular joint (TMJ).
How many people have osteoarthritis at 40?
Osteoarthritis can occur at any age, although, it occurs with greater frequency as age increases. At 40 years of age, only 20 % of the population may have osteoarthritis; however, by 65 years the rates drastically increase and a majority will exhibit radiographic evidence of the disease [10].
Is viscosupplementation effective for osteoarthritis?
Viscosupplementation is effective in primary and secondary osteoarthritis [60]. Viscosupplementation has analgesic, anti inflammatory, anabolic, and chondroprotective effects [61]. It is a disease modifying agent as well as provides pain relief [62].
What causes TMD pain?
But trauma to the jaw, the head, or the neck may cause TMD. Arthritis and displacement of the jaw joint disks can also cause TMD pain. In other cases, another painful medical condition such as fibromyalgia or irritable bowel syndrome may overlap with or worsen the pain of TMD.
What is TMD in dentistry?
Temporomandibular disorders (TMD) are disorders of the jaw muscles, temporomandibular joints, and the nerves associated with chronic facial pain. Any problem that prevents the complex system of muscles, bones, and joints from working together in harmony may result in temporomandibular disorder. The National Institute of Dental ...
What are the symptoms of TMD?
The National Institute of Dental and Craniofacial Research classifies TMD by the following: 1 Myofascial pain. This is the most common form of TMD. It results in discomfort or pain in the fascia (connective tissue covering the muscles) and muscles that control jaw, neck and shoulder function. 2 Internal derangement of the joint. This means a dislocated jaw or displaced disk, (cushion of cartilage between the head of the jaw bone and the skull), or injury to the condyle (the rounded end of the jaw bone that articulates with the temporal skull bone). 3 Degenerative joint disease. This includes osteoarthritis or rheumatoid arthritis in the jaw joint.
What is the most common form of TMD?
The National Institute of Dental and Craniofacial Research classifies TMD by the following: Myofascial pain. This is the most common form of TMD. It results in discomfort or pain in the fascia (connective tissue covering the muscles) and muscles that control jaw, neck and shoulder function.
What does TMD feel like?
Sensitivity of the teeth without the presence of an oral health disease. Numbness or tingling sensation in the fingers. A change in the way the upper and lower teeth fit together. The symptoms of TMD may look like other conditions or medical problems. See a dentist or your doctor for a diagnosis.
How do you know if you have TMD?
The following are the most common signs and symptoms of TMD: Jaw discomfort or soreness ( often most prevalent in the morning or late afternoon) Headaches. Pain spreading behind the eyes, in the face, shoulder, neck, and/or back. Earaches or ringing in the ears (not caused by an infection of the inner ear canal)
What is internal derangement of the joint?
Internal derangement of the joint. This means a dislocated jaw or displaced disk, (cushion of cartilage between the head of the jaw bone and the skull), or injury to the condyle (the rounded end of the jaw bone that articulates with the temporal skull bone). Degenerative joint disease.
What is the term for the breakdown of the TMJ?
Osteoarthritis. Breakdown of the bony surface of the TMJ condyle has been termed osteoarthritis and degenerative joint disease. All three terms refer to the same underlying changes.
Can TMJ degeneration cause pain?
It may also be associated with long-term advanced internal derangement in the TMJ. When degeneration does occur, it can lead to pain and joint dysfunction. This is generally managed by a medical professional, as it is when it occurs in other joints in the body (e.g., hip, knee, etc.).

Diagnosis
Treatment
- In some cases, the symptoms of TMJ disorders may go away without treatment. If your symptoms persist, your doctor may recommend a variety of treatment options, often more than one to be done at the same time.
Alternative Medicine
- Complementary and alternative medicine techniques may help manage the chronic pain often associated with TMJ disorders. Examples include: 1. Acupuncture.A specialist trained in acupuncture treats chronic pain by inserting hair-thin needles at specific locations on your body. 2. Relaxation techniques.Consciously slowing your breathing and taking deep, regular breaths c…
Preparing For Your Appointment
- You'll probably first talk about your TMJ symptoms with your family doctor or dentist. If suggested treatments don't provide enough relief, you may be referred to a doctor who specializes in TMJ disorders.