
When a patient refuses initial life-sustaining treatment, respectfully explore the underlying reason for the refusal. This allows the healthcare team to identify alternative options that may be equally medically effective and also acceptable to the patient. In the end, the patient has the right to accept or refuse life-sustaining medical treatment.
Full Answer
Can a patient refuse life-sustaining medical treatment?
In the end, the patient has the right to accept or refuse life-sustaining medical treatment. After a competent patient chooses to forego a life-sustaining treatment or procedure, the healthcare team is faced with only one option: We must support the wishes of the patient that will ultimately result in his or her death.
What is the right to refuse life saving treatment?
Right To Refuse Lifesaving Treatment. Under such circumstances, the patient’s right to refuse or terminate life-sustaining treatment would override competing state interests in preserving life and the exercise of the right would not amount to suicide.
Can I refuse medical treatment based on my religious beliefs?
Where there is a compelling state interest, an individual’s right to refuse medical treatment based on his/her religious beliefs shall not be recognized and the court shall order the proceeding with such treatment. However, in People v.
How do you indicate the right to refuse treatment?
Advance Directives: The best way for a patient to indicate the right to refuse treatment is to have an advance directive, also known as a living will. Most patients who have had any treatments at a hospital have an advance directive or living will.
Can a patient refuse life saving medical treatment?
Every competent adult has the right to refuse unwanted medical treatment. This is part of the right of every individual to choose what will be done to their own body, and it applies even when refusing treatment means that the person may die.
Can a competent patient refuse life sustaining treatment?
Similarly, if the patient refusing the life-sustaining treatment is competent, one of the two necessary conditions for treatment discussed above is not fulfilled and hence the patient's health care providers are not ethically permitted to start the treatment.
How do you decline medical treatment?
Advance Directives The best way to indicate the right to refuse treatment is to have an advance directive.
What do you do when a patient refuses life saving treatment?
When a patient refuses initial life-sustaining treatment, respectfully explore the underlying reason for the refusal. This allows the healthcare team to identify alternative options that may be equally medically effective and also acceptable to the patient.
Can you be forced to have medical treatment?
You cannot legally be treated without your consent as a voluntary patient – you have the right to refuse treatment. This includes refusing medication that might be prescribed to you. (An exception to this is if you lack capacity to consent to treatment.)
What if the family disagrees with the DNR order?
What if the Family Disagrees with the DNR Order? If the family disagrees with the DNR order, then they have a right to speak with the attending physician. The physician should make a reasonable effort to explain the patient's prognosis and treatment options, along with the patient's wishes.
Is it a human right to refuse medical treatment?
The Human Rights Court has confirmed that Article 8 protects our physical, moral and psychological integrity, as well as our right to choose. Failing to respect someone's competent refusal of medical treatment, and providing treatment against their will, is therefore protected against by Article 8.
Is it a constitutional right to refuse medical treatment?
The Fourteenth Amendment provides that no State shall "deprive any person of life, liberty, or property, without due process of law." The principle that a competent person has a constitutionally protected liberty interest in refusing unwanted medical treatment may be inferred from our prior decisions.
Do patients have the ethical right to refuse treatment?
Competent patients have a right to refuse treatment. This concept is supported not only by the ethical principle of autonomy but also by U.S. statutes, regulations and case law. Competent adults can refuse care even if the care would likely save or prolong the patient's life.
What are the ethical issues when a patient refuses treatment?
In general, ethical tension exists when a physician's obligation to promote a patient's best interests competes with the physician's obligation to respect the patient's autonomy.
Can a nurse force a patient to take medication?
Because a client legally has the right to refuse medication, the nurse can only recommend, advise, suggest, or urge the patient to comply. Consequently, it is important to understand the nurse's response to patient refusal of medication.
When should a physician elicit patient goals of care?
Physicians should elicit patient goals of care and preferences regarding life-sustaining interventions early in the course of care, including the patient’s surrogate in that discussion whenever possible.
Is there an ethical difference between withholding and withdrawing treatment?
While there may be an emotional difference between not initiating an intervention at all and discontinuing it later in the course of care, there is no ethical difference between withholding and withdrawing treatment.
Can a surrogate make decisions on behalf of a patient?
There is no surrogate available and willing to make decisions on behalf of a patient who does not have decision-making capacity or no surrogate can be identified. In the physician’s best professional judgment ...
Is it ethical to withhold life sustaining interventions?
Decisions to withhold or withdraw life-sustaining interventions can be ethically and emotionally challenging to all involved. However, a patient who has decision-making capacity appropriate to the decision at hand has the right to decline any medical intervention or ask that an intervention be stopped, even when that decision is expected to lead ...
What is the dilemma of emergency medicine?
One of the greatest dilemmas for emergency physicians occurs when a patient refuses medical treatment that is necessary to sustain life and health. When patients in need explicitly refuse life-sustaining emergency treatment, the physician must choose between the undesirable options of forgoing beneficial treatment and forcing treatment on a competent but unwilling patient [1], both of which have potential ethical and legal consequences. The “emergency privilege” does not permit physicians to treat competent patients with emergency conditions who refuse treatment; but how does one assess an injured patient’s decision-making capacity?
What are the limitations of determining DMC?
In the emergency setting, there are limitations on determining DMC. When faced with medical emergencies requiring urgent action and decision making, the emergency practitioner does not have the luxury of time to consult psychiatric professionals, an ethics committee, or hospital legal counsel.
Can a comatose patient be intubated?
Certainly, a comatose patient, a severely demented patient, or an intubated, head-injured patient lacks decisional capacity. Under the “emergency exception,” immediate intervention can proceed without informed consent in order to prevent death or serious disability.
What does the court consider when deciding an individual's right to refuse lifesaving treatment?
The courts, in deciding an individual’s right to refuse lifesaving treatment, even if there is a possibility of a cure, consider the competency of the individual as to whether an individual has knowingly and validly chosen such a right, and whether there is a compelling state interest that justifies overriding the individual’s decision.
What was the case in Columbian Presbyterian Medical Center?
Sup. Ct. 1965), it was found that the court authorized blood transfusions for a member of Jehovah’s Witnesses who was in a critical state and had refused pleas of her husband and family and hospital staff that she sign authorization for blood transfusions.
Is blood transfusion a risk?
Nevertheless, while considering the state’s interest in preserving life in blood transfusion cases that can cure the patient’s condition, the court should examine the facts that blood transfusions are not without risk and can result in adverse complications affecting the patient due to impure blood transfusion.
Is a minor child dependent on a patient?
Where there are minor children dependent upon the survival of the patient, the medical control of one’s body is relative. Therefore, the need of protection of innocent third parties arises and where there are such minor children dependent on the patient, the court will not recognize the patient’s right to refuse medical treatment even ...
Can a patient refuse life-sustaining treatment?
The competent adults irreversibly sustained by artificial life support and enduring physical and mental pain and suffering had the right to terminate treatment. Under such circumstances, the patient’s right to refuse or terminate life-sustaining treatment would override competing state interests in preserving life and the exercise of the right would not amount to suicide.
What is the best way for a patient to indicate the right to refuse treatment?
Advance Directives. The best way for a patient to indicate the right to refuse treatment is to have an advance directive, also known as a living will. Most patients who have had any treatments at a hospital have an advance directive or living will.
What are the rights of a patient who refuses treatment?
In addition, there are some patients who do not have the legal ability to say no to treatment. Most of these patients cannot refuse medical treatment, even if it is a non-life-threatening illness or injury: 1 Altered mental status: Patients may not have the right to refuse treatment if they have an altered mental status due to alcohol and drugs, brain injury, or psychiatric illness. 6 2 Children: A parent or guardian cannot refuse life-sustaining treatment or deny medical care from a child. This includes those with religious beliefs that discourage certain medical treatments. Parents cannot invoke their right to religious freedom to refuse treatment for a child. 7 3 A threat to the community: A patient's refusal of medical treatment cannot pose a threat to the community. Communicable diseases, for instance, would require treatment or isolation to prevent the spread to the general public. A mentally ill patient who poses a physical threat to himself or others is another example.
What is the end of life refusal?
End-of-Life-Care Refusal. Choosing to refuse treatment at the end of life addresses life-extending or life-saving treatment. The 1991 passage of the federal Patient Self-Determination Act (PSDA) guaranteed that Americans could choose to refuse life-sustaining treatment at the end of life. 9 .
How can a patient's wishes be honored?
Another way for a patient's wishes to be honored is for the patient to have a medical power of attorney. This designates a person to make decisions on behalf of the patient in the event they are mentally incompetent or incapable of making the decision for themselves.
What must a physician do before a course of treatment?
Before a physician can begin any course of treatment, the physician must make the patient aware of what he plans to do . For any course of treatment that is above routine medical procedures, the physician must disclose as much information as possible so you may make an informed decision about your care.
What are the four goals of medical treatment?
There are four goals of medical treatment —preventive, curative, management, and palliative. 2 When you are asked to decide whether to be treated or to choose from among several treatment options, you are choosing what you consider to be the best outcome from among those choices. Unfortunately, sometimes the choices you have won't yield ...
Why do patients make this decision?
Patients make this decision when they believe treatment is beyond their means. They decide to forgo treatment instead of draining their bank accounts. Those who live in a country with a for-profit healthcare system may be forced to choose between their financial health and their physical health.
What is mature minor doctrine?
Despite its novelty, the mature minor doctrine is a prevailing pattern found in many state jurisdictions. [lix] In considering a minor’s capacity to make autonomy medical decisions, courts consider a constellation of cognitive and social factors.
Can a minor refuse LSMT?
Prior to 1986, no court examined the question of whether a minor has the right to refuse LSMT. In the case of In re D.P., the California Superior Court of Santa Clara County held that a 14-year-old cancer patient could not be held in a hospital against her will, and thus was not required to receive blood transfusions. [xxviii] The following year, in Cardwell v. Bechtol, the Tennessee Supreme Court addressed the issue of whether a minor can consent to medical treatment. [xxix] In Cardwell, a minor and her parents brought suit against an osteopath for medical malpractice on the grounds that the osteopath failed to obtain informed consent for a medical procedure. [xxx] The Court in Cardwell “recognize [d] the varying degrees of responsibility and maturity of minors” [xxxi] and ruled that if a minor has the capacity to consent to and appreciate the nature, risk, and consequences of medical treatment, that the minor functions as an adult when making decisions on medical treatment. [xxxii] The Court, however, warned that the “ [a]doption of the mature minor exception to the common law rule [was] by no means a general license to treat minors without parental consent and [the exception’s] application [was] dependent on the facts of each case.” [xxxiii]
Can a terminally ill minor refuse LSMT?
Recent judicial rulings, [i] legislative developments, [ii] and public policy polls [iii] suggest that the United States is prepared to hold a serious conversation surrounding a patient’s right to refuse LSMT. State legislatures have made significant progress in the Death with Dignity movement; however, minimal progress, if any, has been made on whether competent, terminally ill minors should also have the right to refuse LSMT.
Can minors consent to medical treatment?
Minors are generally presumed legally incompetent, and thus lack the authority to consent to medical treatment. [xliv] Under U.S. common law, parents enjoy a substantive constitutional right to make health care decisions on behalf of their children. [xlv] This is particularly true in the realm of end-of-life care. [xlvi] The notion that minors lack the capacity to make independent decisions concerning medical treatment rests on the presumption that minors lack the maturity and wisdom to make such decisions. [xlvii] In Prince v. Massachusetts, the Supreme Court articulated that “ [p]arents may be free to become martyrs themselves. But it does not follow they are free, in identical circumstances, to make martyrs of their children before they have reached the age of full and legal discretion when they can make that choice for themselves.” [xlviii] This parental right, however, is generally assumes that parents will act in the best interest of the minor. [xlix]
Why did Daniel refuse chemotherapy?
The refusal was based on their religious practice of Nemenhah, a Native American healing practice in which Daniel was a medicine man and which forbade chemotherapy because of a prohibition against doing harm [10]. Daniel was unable to articulate why he opposed the chemotherapy beyond the notion of “do no harm,” and experts placed his reading below ...
What is the right to make decisions?
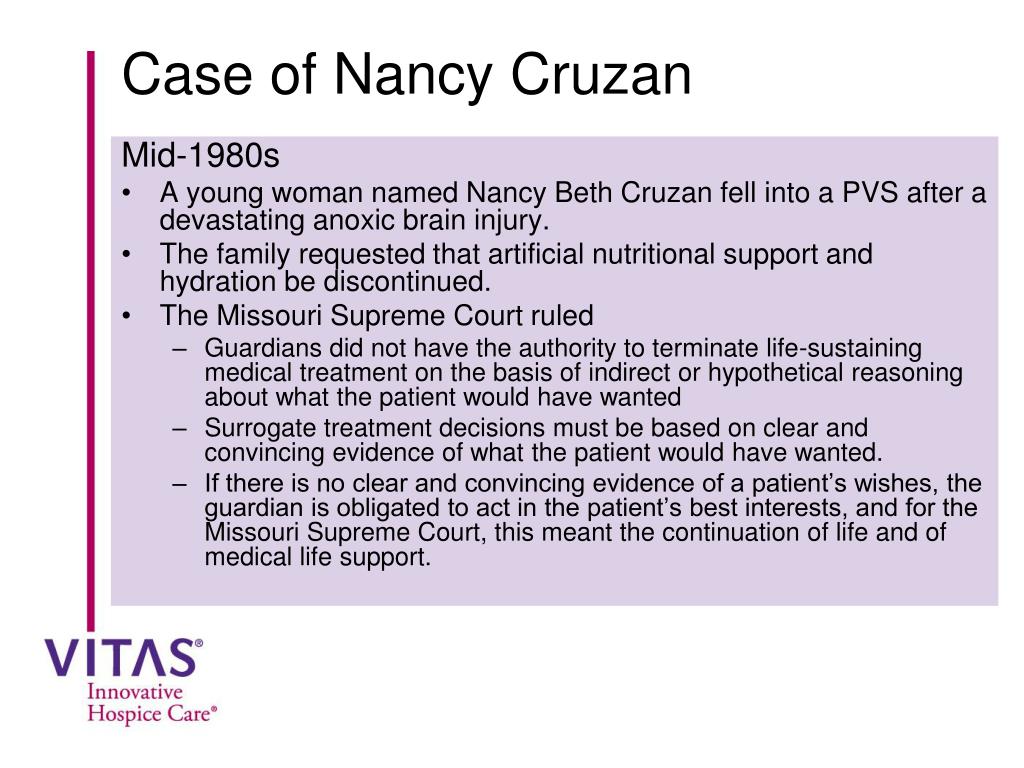
Adults with decision-making capacity have a long-recognized and legally protected right to make decisions about their bodies and health, stemming from interest in their autonomy and bodily integrity. This is emphasized by famous cases like Cruzan v. Director Missouri Department of Health, in which the U.S. Supreme Court recognized a competent person’s “constitutionally protected liberty interest in refusing unwanted medical treatment” and set the evidentiary standard for proving an unconscious adult would want life-sustaining support removed [1], and Bouvia v. Superior Court, in which a California court allowed a 28-year-old woman with cerebral palsy to order withdrawal of the nasogastric tube that fed her [2]. The right to refuse life-saving therapies on religious grounds is also strongly defined, most notably the refusal of blood transfusions by Jehovah’s Witnesses [3].
Is parental consent required for mental health?
Some states have statutes that specify types of care for which parental consent is not required, such as treatment for sexually transmitted infections, treatment for substance abuse or mental health, or requests for contraceptives [8].
Do teenagers have the right to make their own medical decisions?
Unlike their adult counterparts, teenager s generally do not have the right to make their own medical decisions, and physicians, families, and sometimes the courts are left to make difficult choices that have implications for religious freedom, parental rights, and a child’s well-being alike. Three stories help illustrate ...
Does every refusal involve religion?
While not every refusal involves religion, many do, whether the belief is on the part of the child, the parent, or both. The freedom to practice religion is strongly undergirded by the First Amendment of the Constitution, which prohibits Congress from making any law that interferes with it [12].
Can Jehovah's Witnesses refuse blood transfusions?
The right to refuse life-saving therapies on religious grounds is also strongly defined, most notably the refusal of blood transfusions by Jehovah’s Witnesses [3]. Whether the same rights apply to minors (typically defined as younger than 18, though the definition varies by state) is more complex.
