:quality(70)/https://d1l9wtg77iuzz5.cloudfront.net/assets/2696/307311/original_instagram.png?1593641995)
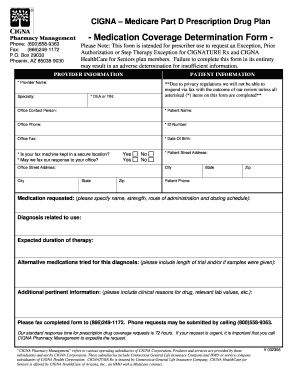
How do I get a prior authorization from CIGNA?
The prior authorization process gives your health insurance company a chance to review how necessary a medical treatment or medication may be in treating your condition. For example, some brand-name medications are very costly. During their review, your health insurance company may decide a generic or another lower-cost alternative may work ...
Does Cigna pre-approve procedures?
Prior Authorization may include, for example, a Step Therapy determination. Step Therapy determines the specific usage progression of therapeutically equivalent drug products or …
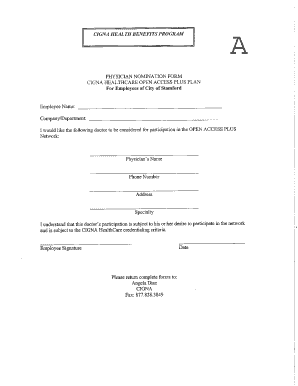
How do I request a referral from CIGNA for health care professionals?
Cigna claims: PO Box XXXX, Anytown, USA 12345-6789 TPV name, PO Box XXXX, Anytown, USA 12345-6789 CSN name, PO Box XXXX, Anytown, USA 12345-6789 Customer service: …
What does precertification mean for Cigna services?
Enrollee‘s Name Date of Birth Enrollee‘s Address City State Zip Code Phone Enrollee‘s Member ID #. Complete the following section ONLY if the person making this request is not the enrollee or …
How long does Cigna preauthorization take?
For health insurance providers like Cigna, the prior authorization process takes an average of 5.7 hours, down from 18.7 hours.Feb 24, 2022
What is the difference between precertification and prior authorization?
Sometimes called prior authorization, prior approval or precertification. Your health insurance or plan may require preauthorization for certain services before you receive them, except in an emergency. Preauthorization isn't a promise your health insurance or plan will cover the cost.
What is a preauthorization request?
A prior authorization (PA), sometimes referred to as a “pre-authorization,” is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine, medical device or procedure.
How do I submit a prior authorization to Cigna?
If you are unable to use electronic prior authorization, you can call us at 1 (800) 882-4462 to submit a prior authorization request.
How can I speed up my insurance authorization?
16 Tips That Speed Up The Prior Authorization ProcessCreate a master list of procedures that require authorizations.Document denial reasons.Sign up for payor newsletters.Stay informed of changing industry standards.Designate prior authorization responsibilities to the same staff member(s).More items...
How do pre authorizations work?
A pre-authorization is a restriction placed on certain medications, tests, or health services by your insurance company that requires your doctor to first check and be granted permission before your plan will cover the item.Feb 1, 2022
What is preauthorization charge?
Authorization hold (also card authorization, preauthorization, or preauth) is a service offered by credit and debit card providers whereby the provider puts a hold of the amount approved by the cardholder, reducing the balance of available funds until the merchant clears the transaction (also called settlement), after ...
What is pre-authorization payment?
A credit card pre-auth is when a merchant reserves a transaction amount temporarily on a credit card, but only debits the amount after a few hours or days. This way, merchants can guarantee the availability of a payment amount for a specific transaction before it is finally confirmed.May 14, 2020
How long does a pre-authorization take to cancel itself?
The pre-authorization is voided on our end immediately. However, the time release depends on your individual credit / debit card bank. Once posted, it typically takes 2-3 days for the pre-authorization charge to be removed by your bank.
How do I check my Cigna authorization status?
You can see the status of your claims on the myCigna® website. When a claim is approved, we either pay the health care provider directly or you do, depending on who submitted the claim. In most cases for in-network care, providers will file claims for you and you'll receive an explanation of benefits, or EOB.
What should you do with the authorization number once you have prior approval?
What should you do with the authorization number once you have prior approval? Document it in the financial record and on all forms associated with the procedure.
How long does prior authorization for medication take?
How Long Does a Prior Authorization Take to Get? Once your physician submits a request for prior authorization, a decision is usually returned in several days. In some instances, the initial request may take as long as a week, and appeals may take even longer.Jun 1, 2021
What happens when a claim is approved?
When a claim is approved, we pay the health care provider or you, depending on who submitted the claim. In most cases for in-network care, providers will file claims for you and you’ll receive an explanation of benefits, or EOB. Your EOB is not a bill but an explanation of how your claim was paid. The provider will bill you directly ...
Does an HMO cover urgent care?
Most HMO, Network and EPO plans only include out-of-network coverage for emergency care. Some plans may also cover urgent care services, as defined in plan documents. In this instance, you will usually need to file a claim since out-of-network providers are not required to submit a claim on your behalf.
What to do if you are unhappy with prior authorization?
If you are unhappy with the results of your prior authorization, you or your health care provider can ask for another review of the decision. Or, your health care provider may prescribe a different treatment or medication. In some instances, your health plan will recommend an alternative treatment or medication before coverage is available ...
Is health care confusing?
Health care can be confusing . The good news is we’re here to help. Below are a few important terms that will help you to better understand your medical bills and health plan coverage.
What is retroactive denial?
A retroactive denial is a claim paid by Cigna and then later denied, requiring you to pay for the services. A retroactive denial could be due to: Eligibility issues. Service (s) determined to be not covered by your plan. Rescission (or cancellation) of coverage. Ways to avoid denied claims:
Is EOB a bill?
An EOB is not a bill. It is a document to help you understand how much each service costs, how much your plan will cover, and how much you will have to pay when you receive a bill from your doctor or hospital. It includes:
What to do if Cigna denied my claim?
Get prior authorization, if required by the plan. What to do if your claim is retroactively denied: Cigna will notify you in writing about your appeal rights. For additional assistance, call Customer Service at 1 (800) Cigna24 (1 (800) 244-6224). Learn more about appeals and grievances.
Why do insurance companies require prior authorization?
The prior authorization process gives your health insurance company a chance to review how necessary a certain medication may be in treating your medical condition.
What is prior authorization?
Prior authorization may also apply to certain health care treatments, services and/or supplies. If you use a health care provider in your plan’s network, then the provider is responsible for obtaining approval from your health insurance company. If you don’t use a health care provider in your plan’s network, then you are responsible ...
What is a shared administration repricing plan?
It’s designed for Taft-Hartley and federal plan employers that want to continue processing and paying their claims, retain customer and provider service, or use a third-party administrator to perform these functions.
Does Cigna offer dental insurance?
Cigna offers Individual & Family Plans with medical, pharmacy, and (when applicable) pediatric dental benefits in Arizona, California, Colorado, Connecticut, Florida, Georgia, Maryland, Missouri, North Carolina, South Carolina, Tennessee, and Texas. Depending on the plan, customers will have access to health care professionals who participate in one of four networks: Connect Network, Focus Network, LocalPlus Network, or Open Access Plus Network. The network name will appear on the top right of the ID card.
Does Cigna have an alliance with health insurance companies?
Cigna has entered into strategic alliances with several nationally recognized health care companies. These plans give our customers access to an alliance’s network of health care professionals and discounts in specific geographic areas. They also provide the alliance’s customers with access to Cigna’s national health care professional network and discounts outside their specific geographic area.
Is the Apple logo a trademark?
The Apple logo is a trademark of Apple Inc., registered in the U.S. and other countries. App Store is a service mark of Apple Inc. Android and Google Play are trademarks of Google Inc. Amazon, Kindle, Fire and all related logos are trademarks of Amazon.com, Inc. or its aliates. Blackberry and Blackberry World are trademarks or registered trademarks of BlackBerry Limited, the exclusive rights to which are expressly reserved. Cigna is not aliated with, endorsed, sponsored, or otherwise authorized by BlackBerry Limited. The downloading and use of the myCigna Mobile App is subject to the terms and conditions of the app, and the online store from which it is downloaded. Standard mobile phone carrier and data usage charges apply.
How long does it take for Cigna to make a decision?
Decisions are made within two business days of receiving all necessary information. You and your doctor will be notified by phone, email and by U.S. Mail. Cigna receives a request while you are receiving care or in a hospital, skilled nursing facility or rehabilitation facility (concurrent review).
Does Cigna require precertification?
Your plan may require precertification for hospital admissions and some outpatient services. When precertification is required, a Cigna nurse reviews the request using nationally recognized guidelines. These guidelines help the nurse decide what services are covered based on your plan coverage.
What does PCP stand for?
PCP stands for Primary Care Physician. Your PCP will be your source for basic care, advice and direction. Your PCP will also coordinate your total care - from preventive checkups and routine medical care to specialized care and hospitalizations.
How long can you wait to make an appointment?
There are standards, required by law, to make sure your appointment happens in a timely manner. The following legal standards set the number of days or weeks you can wait for an appointment based on your medical needs: Emergency: Immediately. Emergencies are medical problems that are life-threatening.
PRECERTIFICATION GUIDELINES
Precertification can be complicated. Knowing the right place to start can make a big difference.
New process to order home health services for Cigna Commercial customers
Contact participating home health, durable medical equipment, and home infusion therapy providers directly. CareCentrix no longer manages these services for Cigna. eviCore healthcare now administers these programs; however, approval or contact with eviCore is not needed.#N#To find a participating home health/DME provider:
Determine if precertification is required
View the complete list of services that require precertification of coverage:
Follow the service specific precertification process
To better serve our providers, business partners, and patients, the Cigna Coverage Review Department is transitioning from PromptPA™, fax, and phone coverage reviews, also called prior authorizations, to Electronic Prior Authorizations. ePAs save time and help patients receive their medications faster.
Medical
There are three ways to request precertification for medical procedures. Upon submission of a precertification request, please provide all required information. Failure to provide all necessary information required for the review may result in the denial of certification for an admission, procedure or service.
For many services, we manage the precertification process directly
Use your practice management system or vendor: Health Care Request and Response (ANSI 278) - Contact your Electronic Data Interchange (EDI) or Practice Management System vendor.
For the following services, we collaborate with national ancillaries to support the precertification process and administration of the services
To request precertification, use the contact information below or visit the website for next steps.
What Is A Claim?
HMO, Network, Or EPO Plans
Point of Service (POS) Plans
Indemnity Plans
Claims Process
Prior Authorizations
EOB
- What is an EOB?
An EOB (Explanation of Benefits) is a claim statement that Cigna sends to you after a health care visit or procedure to show you how your claim was paid. An EOB is not a bill. It is a document to help you understand how much each service costs, how much your plan will cover, and how muc…