Full Answer
What are outcome measurement tools in therapy?
Outcome measurement tools, in mental health therapy, empower you—and your clients—to set goals and determine the treatment’s effectiveness. “Our goals can only be reached through a vehicle of a plan, in which we must fervently believe, and upon which we must vigorously act. There is no other route to success.” —Pablo Picasso
How effective are care outcome measures?
Effectiveness of care outcome measures evaluate two things: Compliance with best practice care guidelines. Achieved outcomes (e.g., lower readmission rates for heart failure patients).
What are Patient-Reported Outcome measures?
Patient-reported outcome measures (PROMs) fall within the patient experience outcome measure category. According to the Agency for Clinical Innovation (ACI), PROMs “assess the patient’s experience and perception of their healthcare.
What do patients want from outcomes data?
Patients rely on outcomes data to make educated decisions about their healthcare. Quality reporting organizations, such as The LeapFrog Group, evaluate and report on U.S. hospital safety and quality performance. Patients want reassurance that they’re receiving the best care for the lowest cost.
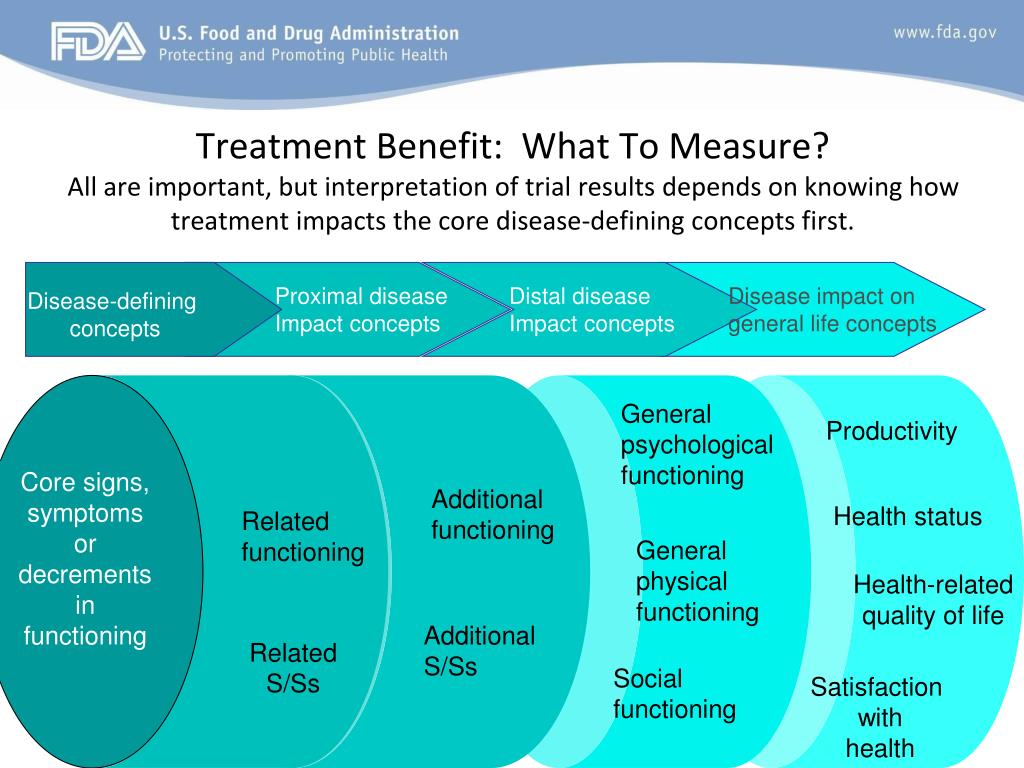
How do you measure treatment outcomes?
Treatment outcome is measured by scales developed or adapted from other instruments across the domains of dependence, blood borne virus exposure risk, drug use, health, psychological functioning and social functioning.
How do you measure therapeutic progress?
A great way to know you're making progress in therapy is getting a diagnosis that's improved. If you're in treatment for depression, and you and your therapist agree the symptoms have dissipated, you've made significant progress.
What is an outcome measure in healthcare?
Outcome measures reflect the impact of the health care service or intervention on the health status of patients. For example: The percentage of patients who died as a result of surgery (surgical mortality rates). The rate of surgical complications or hospital-acquired infections.
What is treatment outcome?
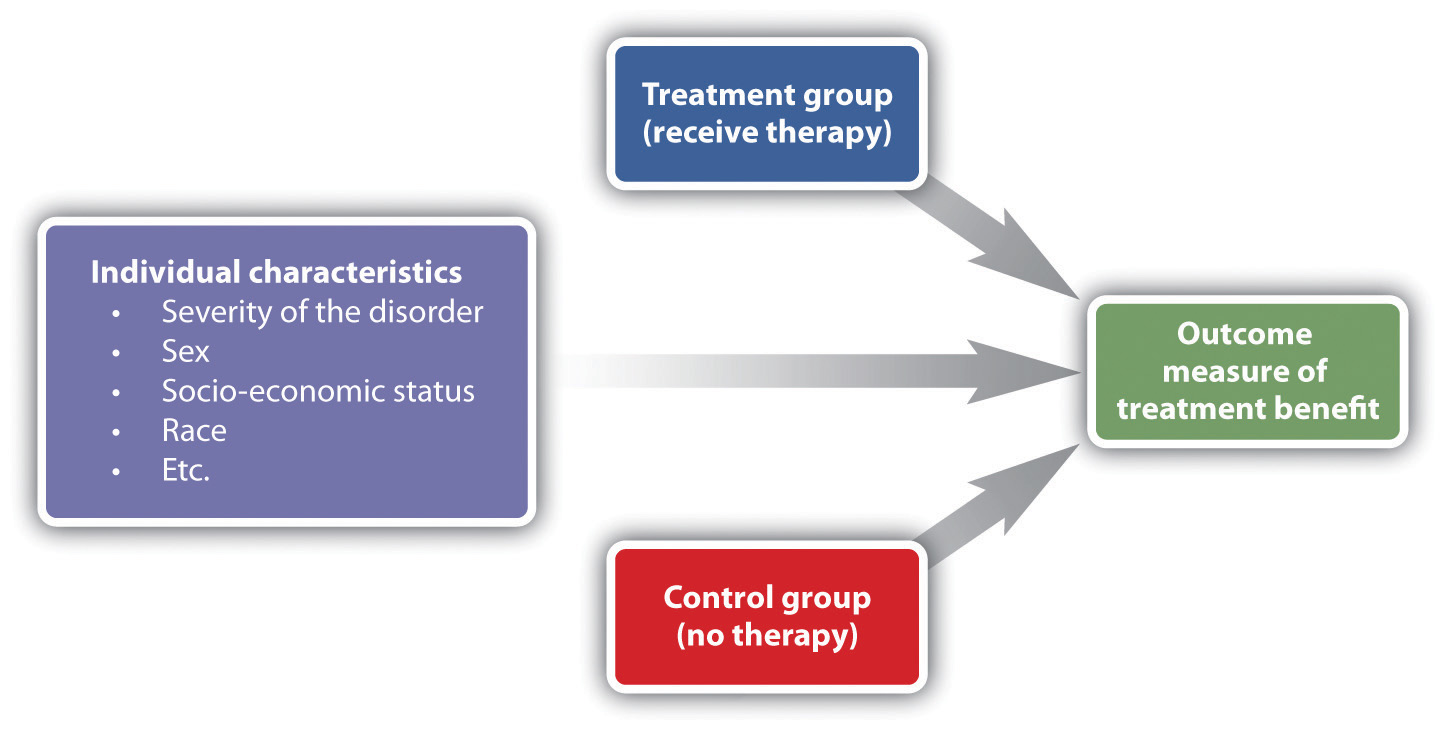
Treatment outcome research was defined by Mowrer (1953) as a situation whereby the “emphasis is upon measuring significant aspects of personality before and after treatment and noting the nature and extent of the resulting changes” (p. 4).
What is Outcome Rating Scale?
The Outcome Rating Scale (ORS) is used by the client to rate three domains: individual (personal well-being), interpersonal (family/close relationships), and social (work/school/friendships) as well as an overall rating. Once the scale is completed by the client, results are shared and discussed openly.
How do you monitor the progress of a client?
How to Track Client ProgressProgress reports. Structured progress reports are a simple and effective means of helping clients evaluate progress and focus on their goals. ... 'Before and after' photos. Sometimes a simple visual reminder can speak volumes. ... Workout or nutrition records. ... Communication.
How do you measure clinical effectiveness?
Evaluating clinical effectiveness and improving future care involves examining a number of indicators alongside each other. These include patient safety indicators, patient satisfaction, productivity measurement tools, and how effective clinicians are in supporting people to achieve their best clinical outcomes.
How do you evaluate nursing outcomes?
Five Steps of the Evidence-based ProcessAsk a clinical question.Obtain the best research literature.Critically appraise the evidence.Integrate the evidence with clinical expertise, patient preferences.Evaluate the outcomes of the decision.
Why do we measure outcomes?
Measuring health outcomes allows us to make decisions about how to best care for our patients and outcome measures help us predict the patients who might benefit most from a particular intervention. It helps us identify any improvement after an intervention is provided.
What is treatment outcome research?
research designed to evaluate the efficacy of interventions and to investigate the mechanism by which effective interventions produce change.
What is therapy outcome study?
research that investigates the end results of therapy or other interventions to which patients are exposed. The focus is primarily on the “cure” (or not) of patients, but the research also evaluates their experiences, preferences, and values, as well as the wider influence on society.
What is the purpose of a treatment outcome study?
Treatment outcome studies are designed to answer commonsense questions. To determine whether a treatment accomplishes anything, we have to know how patients who have not received the treatment fare. Perhaps untreated patients do just as well, implying that the treatment does not influence outcome at all.
What is outcome measurement in therapy?
Outcome measurement tools in mental health therapy also allow counselors to measure the impact of treatment over the course of time. If little-to-no progression occurs, the client and clinician can tweak the course of therapy to see better results.
How to use outcome methods in private practice?
The first step to using outcome methods in your private practice is to determine which specific standardized assessments suit your demands. Individual therapists will prefer different evaluation methods, so find the one you are most comfortable using. Then, create the goals—working with your new clients—to measure treatment effectiveness.
Why are standardized instruments important?
Standardized instruments were developed to monitor whether or not treatment is effective, and measuring results aids both the client and clinician through the treatment process, regardless of whether you use self-reporting or performance-based measures. By setting goals with new clients, they can track their own progress over time, giving them the motivation to continue treatment and celebrate successes along the way.
How to assess effectiveness of therapy for OCD?
For example, one way to assess the effectiveness of therapy for a client with OCD is to monitor the frequency and/or amount of times she washes her hands. If her baseline for hand-washing at the start was 1-2 minutes at a time, or over 25 times a day, and through the course of treatment it decreased to twenty seconds at a time , or only ten times throughout the day, the process is proving successful.
What is modern counseling?
Modern counseling has evolved to be a diverse practice with clinicians who embrace various methods, theories, and populations. In your private practice, while you may subscribe to a particular model, such as cognitive behavioral therapy, holistic health, strength-based, or others, you still temper treatments based on an individual client needs. ...
Is client-therapist alliance a predictor of positive clinical outcome?
A 2001 study published in Frontiers in Psychology found that “the quality of the client–therapist alliance is a reliable predictor of positive clinical outcome independent of the variety of psychotherapy approaches and outcome measure.”.
Can you use the same outcome measurement tools in mental health?
Regardless of the method chosen, stick with the same outcome measurement tools in mental health treatment, instead of using one to start, and changing to a different one later. That would be comparing apples to oranges, and no significant value could be determined.
What is the FICS scale?
measure that we rely upon for this feedback is the Family Interaction and Communication Scale (FICS). The FICS assesses the perspective of both the Parent and the Adolescent in measuring problematic Family Relational Dynamics. Higher scores on the FICS indicate greater levels of Familial discord and dysfunction. Lower scores indicate familial harmony. In reviewing the 2012-2013 Annual Outcomes Studies conducted at New Haven, a majority of families experienced significant healing in their family relationships.
What does a higher YOQ score mean?
Higher scores on the YOQ represent greater levels of distress/dysfunction. Lower scores on the YOQ indicate healthier functioning. In analyzing the 2012-2013 Annual Outcomes Studies that involved an overwhelming majority of our client families; New Haven was successful in significantly reducing the severity of scores during treatment, producing an average discharge score well below the clinical cut-off for the measure.
Why is collecting outcomes important?
Collecting outcomes is a best-practice for any treatment program or institution. Measuring treatment outcomes is vital in determining the level of effectiveness, and improving quality of care. At New Haven, practice-based research is a top priority.
What is the Youth Outcome Questionnaire?
The YOQ is a reliable and valid assessment measure yielding statistically significant differences between Clinical and
How much is readmission after hospitalization?
Readmission is costly (and often preventable). In fact, researchers estimate that in one year, $ 25 to $45 billion is spent on avoidable complications and unnecessary hospital readmissions. After increasing efforts to reduce their hospital readmission rate, the University of Texas Medical Branch (UTMB) saw a 14.5 percent relative reduction in their 30-day all-cause readmission rate, resulting in $1.9 million in cost avoidance. UTMB reduced their hospital readmission rate by implementing several care coordination programs and leveraging their analytics platform and advanced analytics applications to improve the accuracy and timeliness of data for informing decision making and monitoring performance.
Why should outcomes measurement always tie back to the quadruple aim?
Outcomes measurement should always tie back to the Quadruple Aim, so healthcare organizations aren’t just reporting numbers . Health systems shouldn’t become so obsessed with numbers that they forget their Quadruple Aim goal. Instead, they should focus on quality and improving the care experience at the most efficient cost.
How does healthcare manage complexities?
Health systems can manage these complexities by taking a closer look at outcome measures —understanding their definitions and nuances, reviewing real-world examples, and integrating three essentials for successful outcomes measurement.
Why is it important to track clinician compliance with care guidelines?
It’s important to track clinician compliance with care guidelines; It’s equally important to monitor treatment outcomes and alert clinicians when care guidelines need to be reviewed.
Why do patients rely on outcomes data?
Patients rely on outcomes data to make educated decisions about their healthcare. Quality reporting organizations, such as The LeapFrog Group, evaluate and report on U.S. hospital safety and quality performance. Patients want reassurance that they’re receiving the best care for the lowest cost.
What is the LeapFrog Group?
Outcome measures are frequently reported to the government, commercial payers, and organizations that report on quality, such as The LeapFrog Group —a national nonprofit that evaluates and reports U.S. hospital safety and quality performance. LeapFrog’s work centers on “increasing transparency among health care providers in order to reduce the estimated 440,000 annual deaths from hospital errors, accidents, and injuries .” While initial measures focused on inpatient care, they have since expanded to include most aspects of care delivery.
What is outcome measure?
The World Health Organization defines an outcome measure as a “change in the health of an individual, group of people, or population that is attributable to an intervention or series of interventions.”. Outcome measures (mortality, readmission, patient experience, etc.) are the quality and cost targets healthcare ...
Why is VBVC important?
Society's relationship with animals is changing, likely influencing the medical care that owners desire for their pets and contributing to the increase in veterinary patients for which care includes referral to a specialist. 15As veterinary care becomes more complex and costly, VBVC can be a way to provide high value care to patients and clients, while helping us understand the outcomes and costs involved with care.
Why is infection prevention important in veterinary care?
This figure highlights the importance of patient‐centered infection prevention in increasing the quality of care. In the tibial plateau leveling osteotomy example, the improved asepsis protocol will lead to less infections hence improve antibiotic stewardship. Furthermore, the lower complications (surgical site infections) post‐surgery will lead to faster rehabilitation and recovery, overall leading to improved outcomes (improved quality of life) and decrease costs. This is the basis at enhancing the value provided to our patients and clients through the value‐based veterinary care framework
How is value based care created?
Value is created by improving the outcomes of patients with a particular clinical condition over the full cycle of care, which normally involves multiple specialties and care sites. To be successful, a key aspect of value based care is working as teams (integrated practice units) centered around the patient's clinical condition. As veterinary medicine has become more specialized and more complex, multidisciplinary communication and trust among the care team are paramount in providing value to patients (and clients).
What is value based care?
In value‐based care, the only true measures of quality are the outcomes that matter to patients. When outcomes are measured and reported, it fosters improvement and adoption of best practices, thus further improving outcomes. Understanding outcomes is central in providing value and represents an opportunity for redefining veterinary patient care.
What are the challenges of outcome measurement?
Aside from survival, outcome measurement remains limited.24Two main challenges for outcome measurement are organizational structure and information technology systems. The tendency is to measure only what the care team directly controls in a particular intervention, what can be measured easily, or the intervention and treatment that can be billed. Furthermore, rather than determining outcomes for the full care cycle over which value is determined, outcomes are assessed for department or billing units. In health care, outcome work often is driven by medical specialty experts or consensus panels, and not multidisciplinary groups for medical conditions. Organizational structure could explain why doctors fail to accept responsibility for outcomes, defending this position by citing their lack of control over “outside” players involved with patient care (even if they belong to the same hospital) or patient compliance.20An additional barrier is the cost implied in obtaining longitudinal patient data because of organizational fragmentation. Lack of an electronic medical record system that could effortlessly capture outcome data and compile it remains a challenge for many health care systems.20Many of these hurdles in outcome data measurement can be easily extrapolated to veterinary medical care, and thus we have a great opportunity for learning about and improving the way care is provided to our patients.
Why is patient-reported outcome important?
Use of patient‐reported outcomes is an essential aspect for improving clinical care, because it enhances the connections among doctors and with patients. Designing and implementing owner‐reported outcomes in veterinary clinical practice will lead to an understanding of the effects of treatments on outcomes and quality of life (QOL) of our patients from the owner's perspective, a key way to assess a veterinary patient's QOL.
What is value maximization?
Value is defined as health outcomes achieved that matter to patients relative to the cost of achieving those outcomes. Improving value requires either improving 1 or more outcomes without increasing costs or lowering costs without negatively affecting outcomes, or both.7Important considerations regarding this concept are: value is not synonymous with cost savings; outcomes should be multidimensional and be defined by the context of the patient; cost determinations should include all costs and, as a result, some costs may increase for others to decrease; and, value is best considered on a long‐term basis.13
What is the effect of low adherence in chronic conditions?
A low rate of adherence in chronic conditions is associated with poor outcome and decreased quality of life , which constitutes an additional burden for the healthcare systems.
What is adherence measured as?
Adherence is usually measured over a period of time and reported as a percentage, offering information about dose taking behavior in relation to what was prescribed. In some cases adherence is reported as dichotomous variable (adherent/ non-adherent) or classifying levels of adherence (low/high adherers) and even as a mean value.
Why are different tools and measurements developed and validated?
Different tools and measurements have been developed and validated in order to effectively and accurately assess adherence and persistence in a wide range of diseases. Each has advantages and disadvantages that should be thoroughly taken into consideration when designing and choosing a suitable method.
Why is adherence to treatment important?
Optimal treatment adherence is essential for the management of chronic conditions and the effectiveness of prescribed therapies. A World Health Organisation (WHO) report underlines the fact that adherence to chronic treatments is as low as 50% [1].
Why is it important to increase adherence?
Being able to correctly identify and estimate treatment adherence has become a research focus in many chronic conditions, and the importance of increasing the effectiveness of adherence interventions is considered to “have a far greater impact on the health of the population than any improvement in specific medical treatments” [1,8]. However, effective interventions to improve treatment adherence can only be developed if research can also provide additional information about predictors and factors related to adherence, for a better understanding of the individual causes.
What is direct method?
Direct methods. Direct methods include measurements of the drug(or a metabolite) concentration in body fluids. Although it may be considered as being an adequate and precise method, which can offer strong evidence of the ingestion of the drug, there are some variables that should be considered.
What is non-invasive monitoring?
Non-invasive, patients not aware that they are being monitored
Why are children referred for ADHD treatment?
Patients with ADHD are most often referred for treatment because of dysfunction in familial, social, emotional, academic, and occupational roles rather than because of ADHD symptoms.13Children are often referred for diagnosis and treatment because of poor academic performance, difficulty making friends, or low self-esteem (functional impairments) rather than because they cannot remain seated or they lose things or interrupt others (ADH D symptoms). Because functional impairments are a primary impetus for seeking treatment, they may be the most appropriate targets for assessing treatment response.14Although behavioral symptoms show moderate correlation with functional impairments, assessment of symptom improvement alone may not adequately reflect changes in functional status.15There is a strong need to broaden outcome assessments to encompass a multidimensional array of outcomes in patients with ADHD.12,14
How many items are needed to identify ADHD?
A subscale of 25 items can be used to identify whether the adult had ADHD as a child
What are the core concepts of ADHD?
We recognize 5 core conceptual areas that are integral to assessing treatment outcomes in ADHD: (1) DSM-IV-TRADHD behavioral symptoms; (2) functional impairment in familial, social, emotional, academic, and occupational areas; (3) quality of life (QOL) or the burden of illness on the daily lives of patients and their families; (4) adaptive life skills (the development of strategies and skills to cope with problem behaviors); and (5) executive function (working memory, goal-directed activity, planning, organization, prioritizing, self-monitoring, and self-regulation). 16,17These overlapping but distinct concepts each contribute to the real-life outcome of the patient. Although some of these concepts are poorly differentiated in the literature and current measurement approaches, we believe that each should be considered when assessing ADHD outcomes. The objective of this review is to discuss approaches for measuring ADHD treatment outcomes in these 5 core conceptual areas.
How many children have ADHD?
An estimated 9.5% of children aged 4 to 17 years1and 4.4% of adults2in the United States meet diagnostic criteria for attention-deficit/hyperactivity disorder (ADHD). Pharmacologic and behavioral therapy can be effective treatments for ADHD,3–6as reflected in ADHD treatment guidelines.7–10However, assessment of treatment response in patients with ADHD has generally been limited to narrowly focused measures of ADHD symptoms as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR),11with relatively little attention to other relevant outcome domains.4,5,12
What is the objective of the adhd review?
Objective:To review measures used to assess treatment response in patients with attention-deficit/hyperactivity disorder (ADHD) across the life span.
How many points are on the Likert scale?
Each item scored on a 5-point Likert scale
What are the four areas of function?
Assesses 4 areas of function: interpersonal relations, psychopathology, function at work or school, use of leisure time