
Can we measure outcomes from the patients’ perspectives in evaluating migraine?
… Migraine is characterized by headache with symptoms such as intense pain, nausea, vomiting, photophobia, and phonophobia that significantly impact individuals’ lives. The objective of this study was to develop a strategy to measure outcomes from the patients’ perspectives for use in evaluating preventive treatments for migraine.
How do you assess the severity of a migraine?
An assessment of severity related directly to migraine was obtained by asking the patient to respond to a single question with seven response categories: “Taking into account all aspects of your disease, how severe is your disease?”
What should be the next research step for migraine?
Suggested next research steps include development of a new PRO instrument for assessing the impact of migraine on functioning incorporating the concepts identified in this study, reflecting the experiences of patients with episodic and chronic migraine. 1. Headache Classification Committee of the International Headache S.
Do pro instruments measure the impact of migraine on physical functioning?
The item level review of PRO instruments revealed that none of the existing PRO instruments were suitable to collect data on impact of migraine on physical functioning, to evaluate treatment benefit. The impact of migraine includes impairments in functioning during and between migraine attacks that vary considerably on a daily basis.
How do you evaluate a migraine?
There's no specific test to diagnose migraines. For an accurate diagnosis to be made, a GP must identify a pattern of recurring headaches along with the associated symptoms. Migraines can be unpredictable, sometimes occurring without the other symptoms. Obtaining an accurate diagnosis can sometimes take time.
How effective is migraine treatment?
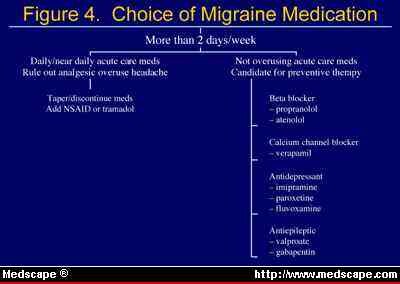
Beta‐blockers are the most widely used class of drugs in prophylactic migraine treatment and are about 50% effective in producing a greater than 50% reduction in attack frequency. Table 2-3 lists beta-blockers and dosages used for the prevention of migraine.
What is the most effective treatment for migraines?
Many people who have migraines find that over-the-counter painkillers, such as paracetamol, aspirin and ibuprofen, can help to reduce their symptoms. They tend to be most effective if taken at the first signs of a migraine attack, as this gives them time to absorb into your bloodstream and ease your symptoms.
How do I know if I have migraine results?
During a migraine, you might have:Pain usually on one side of your head, but often on both sides.Pain that throbs or pulses.Sensitivity to light, sound, and sometimes smell and touch.Nausea and vomiting.
What do you do when a migraine medication doesn't work?
Small tweaks in your daily routine can lower the number of headaches or migraines you have:Drink plenty of water.Don't skip meals.Watch your caffeine intake.Limit alcohol.Manage other health problems. ... Watch your use of medicines. ... Stick to a sleep schedule. ... Get to a healthy weight.More items...•
Do migraine preventatives work?
Anti-seizure Drugs They have been shown to work well in helping limit the number of migraines you get. Those used for treating migraines include gabapentin (Neurontin), topiramate (Qudexy XR, Topamax, Topamax Sprinkle, Trokendi XR) and valproate (Depakene).
How do you treat severe chronic migraines?
TreatmentAntidepressants. Tricyclic antidepressants — such as nortriptyline (Pamelor) — can be used to treat chronic headaches. ... Beta blockers. These drugs, commonly used to treat high blood pressure, are also a mainstay for preventing episodic migraines. ... Anti-seizure medications. ... NSAIDs. ... Botulinum toxin.
Which test is used to detect migraine?
MRI. This test produces very clear pictures, or images, of the brain without the use of X-rays. It uses a large magnet, radio waves, and a computer to produce these images. An MRI may be recommended if you are getting daily or almost daily headaches.
What food to avoid during migraine?
What foods can trigger migraines?aged cheeses.alcohol, particularly beer and red wine.chocolate.cured meats.food preservatives, such as nitrates, nitrites, MSG, and artificial sweeteners.smoked fish.yeast extract.
How long do migraines last with medication?
How long will this last? A migraine can last anywhere from 4 to 72 hours. It can be difficult to predict how long an individual migraine will last, but charting its progress may help. Migraines can usually be divided into four or five distinct stages.
What happens in the brain during a migraine?
One aspect of migraine pain theory explains that migraine pain happens due to waves of activity by groups of excitable brain cells. These trigger chemicals, such as serotonin, to narrow blood vessels. Serotonin is a chemical necessary for communication between nerve cells.
Is it normal to have a migraine for 5 days?
Most migraine headaches last about 4 hours, but severe ones can go for more than 3 days. It's common to get two to four headaches per month. Some people may get migraine headaches every few days, while others get them once or twice a year. This stage can last up to a day after a headache.
What is the best treatment for migraine?
The aim of prophylactic treatments for migraine, such as antiepileptics, antidepressants, and antihypertensives, is not only to reduce migraine frequency, but also reduce disability and restore the ability to function [ 22, 23 ].
How long does migraine last?
Migraine is a common and often debilitating neurologic condition characterized by primary recurrent headaches lasting 4 to 72 h with at least two of the following pain characteristics: unilateral, pulsating, moderate or severe intensity, or aggravated by routine physical activity. In addition, migraine attacks are often accompanied by nausea, ...
What are the dimensions of MSQ?
The MSQ was designed to measure three dimensions: (i) Role Function-Restrictive; (ii) Role Function-Preventive; and (iii) Emotional Function in the past four weeks or in the past week. It was not developed based on concept elicitation interviews with patients with migraine [ 42 ]; therefore, the conceptual fit of the items within each domain subscale has not been explicitly substantiated. The HIT-6 was designed to measure impact of headaches; it is not migraine-specific and also did not involve patient input during its development [ 41] it aims to collect data on the impact of headaches have on the ability to function on the job, at school, at home and in social situations in the past 4 weeks. The MIDAS had similar limitations [ 39] as it was designed to measure the impact of migraine headaches to determine the level of pain and disability caused by migraine in the past 3 months. None of these three instruments were designed to capture the impact of migraine on physical functioning and the day-to-day variability of the experience as reported by patients in the concept elicitation research.
How does migraine affect people?
This study provides a comprehensive assessment of the functional impact of migraine, specifically those of relevance from the individuals’ perspective. Migraine impacts physical functioning, social and leisure activities, and also has emotional impacts. These impacts are experienced during and between migraine attacks and vary considerably day-to-day. This study utilized an iterative and multi-faceted approach to understand patients’ experiences of the impact of migraine. The result of concept identification research and concept elicitation interviews with migraine patients have been used to develop a CDM that can be used as a visual guide to select the COI for developing strategies for measuring outcomes of interventions for migraine, depending on the context of evaluation.
What is concept identification research?
Concept identification research was conducted to understand the impact of migraine in adults. This stage included identifying a list of concepts describing the experience of the impact of migraine symptoms in order to develop a CDM and identify the COI.
How many people with migraines receive preventive care?
However, only approximately 12 % of people with migraine receive any preventive therapy due in part to limited efficacy and significant tolerability and safety issues with available preventive therapies, indicating a large unmet medical need for migraine prophylaxis [ 21 ].
How common is migraine in women?
Migraine is about three times more common in women than men, affecting roughly 18 % of women and 6 % of men in the United States [ 2 – 8 ]. Migraine prevalence estimates are fairly comparable across the world, with 11.5 % of adults meeting criteria for a migraine on average [ 9 ].
Table of Contents
Chronic migraine refers to migraine headaches occurring at least 15 days per month, frequently associated with significant functional impairment and depression.
Chronic Migraine
Chronic migraine refers to migraine headaches occurring at least 15 days per month, frequently associated with significant functional impairment and depression.
What is migraine headache?
Background Migraine is characterized by headache with symptoms such as intense pain, nausea, vomiting, photophobia, and phonophobia that significantly impact individuals’ lives. The objective of this study was to develop a strategy to measure outcomes from the patients’ perspectives for use in evaluating preventive treatments for migraine. Methods This study used a multi-stage process. The first stage included concept identification research through literature review, patient-reported outcome (PRO) instrument content review, and clinician interviews, and resulted in a list of concepts relevant to understand the migraine experience. These results informed the design of the subsequent concept elicitation stage that involved qualitative interviews of adults with migraine to understand their experiences. Information from these two stages was used to develop a conceptual disease model (CDM) of the migraine experience. This CDM was used to identify concepts of interest (COI) to evaluate patient-relevant outcomes for assessing treatment benefit of migraine prophylactics. In the final stage, existing PRO instruments were reviewed to assess coverage of concepts related to the selected COI. Results Nine articles from 563 screened abstracts underwent full review to identify migraine-relevant concepts. This concept identification and subsequent concept elicitation interviews (N = 32; 21 episodic migraine; 11 chronic migraine) indicated that people with migraine experience difficulties during and between migraine attacks with considerable day-to-day variability in the impact on movement, ability to perform every day and social activities, and emotion. The CDM organized concepts as proximal to and more distal from disease-defining migraine symptoms, and was used to identify impact on physical function as the key COI. The item level review of PRO instruments revealed that none of the existing PRO instruments were suitable to collect data on impact of migraine on physical functioning, to evaluate treatment benefit. Conclusions The impact of migraine includes impairments in functioning during and between migraine attacks that vary considerably on a daily basis. There is a need for novel PRO instruments that reflect patients’ migraine experience to assess treatment benefit of migraine prophylactics. These instruments must evaluate the concepts identified and be able to capture the variability of patients’ experience.
What is clinical trial?
Clinical trials are a key component of the evidence base for the treatment of headache disorders. In 1991, the International Headache Society Clinical Trials Standing Committee developed and published the first edition of the Guidelines for Controlled Trials of Drugs in Migraine. Advances in drugs, devices, and biologicals, as well as novel trial designs, have prompted several updates over the nearly 30 years since, including most recently the Guidelines for controlled trials of preventive treatment of chronic migraine (2018), the Guidelines for controlled trials of acute treatment of migraine attacks in adults (2019), and Guidelines for controlled trials of preventive treatment of migraine in children and adolescents (2019). The present update incorporates findings from new research and is intended to optimize the design of controlled trials of preventive pharmacological treatment of episodic migraine in adults. A guideline for clinical trials with devices will be published separately.
Is onabotulinumtoxina effective for migraine?
Background OnabotulinumtoxinA is an effective preventive treatment for chronic migraine. In chronic migraine, besides a reduction in headache frequency, a decreased reliance on oral prophylactics is also indicative of treatment effectiveness. This study aimed to quantify the change in the use of oral prophylactics after treatment with onabotulinumtoxinA in patients with chronic migraine. Methods This was a retrospective, multicentric, cross‐sectional study. Patients with chronic migraine (ICHD‐3b) that had been treated with onabotulinumtoxinA were enrolled consecutively. We collected parameters related to each patient’s pre‐treatment situation, as well as their current one, focusing on frequency and intensity of migraine, number of oral prophylactics and the respective cycle of onabotulinumtoxinA. Univariate and logistic regression analyses were performed. Results We included 542 patients. 90.0% were taking oral preventive treatments. During treatment with onabotulinumtoxinA, 47.8% withdrew at least one prophylactic and 41.6% stopped using oral prophylactics altogether. Factors associated with a reduction or cessations of oral prophylactics were: having>50% improvement in frequency and intensity, remission to episodic migraine, the use of topiramate as an initial treatment, an increased number of infiltrations and a shorter chronification period (p<0.05). The multivariate analysis showed that a chronification period<20 months, >five cycles of onabotulinumtoxinA, >50% improvement in pain intensity and topiramate as an initial treatment were predictors of a reduction in oral prophylactics (AUC of 70.3%; p<0.001). Conclusions Our study demonstrates the efficacy and safety of onabotulinumtoxinA. This treatment reduces the use of oral prophylactics. Withdrawal of oral prophylactics is most likely to occur after five cycles of treatment.
Which meds have the highest efficacy?
Medications with the highest quality of evidence of efficacy are aspirin, ibuprofen, butorphanol nasal spray, oral opiate combinations, dihydroergotamine nasal spray, and triptans (injectable, oral, and nasal spray). Migraine-specific agents such as the triptans are recommended for patients with moderate to severe migraines or milder headaches ...
How many mental health conditions were there in 2001?
The World Health Report 2001—MentalHealth: New Understanding, New Hopecited 135 health conditions, particularly mental and neurologic disorders, that accounted for nearly 40% of all years lived with disability worldwide.
Does migraine affect daily functioning?
FUNCTIONAL IMPAIRMENT AND INDIRECT COSTS. Numerous studies have shown that migraine adversely affects daily functioning . In a 5-nation study by Brandes,15more than half (52.3%) of the 516 adults with migraine interviewed required bed rest to manage their headache attacks.
Is migraine a neurologic disorder?
Migraine headache remains an underrecognized and undertreated neurologic disorder despite the availability of effective treatment and management options. Care improves when health care professionals and patients communicate effectively about the burden of migraine, as recommended in treatment guidelines.
What is MIDAS test?
The MIDAS test is designed to assess the impact of migraines on your daily life. 1 But it does not diagnose migraines or rule out other serious medical conditions.
Can you use MIDAS for health insurance?
Keep in mind that your MIDAS disability score can be used for treatment planning, not for health insurance authorization, worker's compensation, or any other monetary, employment, or school-related purposes.
Is the Midas test helpful?
While the MIDAS test is useful, people with migraines report that the questions miss some of the subtle aspects of migraines, 2 and most want to discuss other details and symptoms with their doctor. It is certainly a helpful tool, but it should not be used as the only means of communication between you and your doctor.
What is migraine headache?
Migraine is a neurological condition characterized by recurrent headaches and other neurological symptoms. Migraine represents one-third of all neurological disease burden [ 1] and is one of the top 15 conditions with the most substantially increased disease burden ranking in the past decade; it is among the top 25 causes of years lived with disability (YLDs) 2. Migraine leads the list of neurological disorders, representing more than 50% of neurological YLDs or 22.9% of global YLDs [ 2 ], imposing considerable burden on the migraineurs and on society. Approximately 90% of persons with migraine have moderate or severe pain, three-quarters have reduced ability to function during headache attacks, and one-third require bed rest during their attacks [ 3, 4, 5, 6 ].
Is migraine a determinant of health outcomes?
In persons with migraine, severity of migraine is an important determinant of several health outcomes (e. g., patient quality of life and health care resource utilization). This study investigated how migraine patients rate the severity of their disease and how these ratings correlate with their socio-demographic, clinical, and psycho-social characteristics.
Is GAMS valid for migraine?
In summary, we demonstrat e the validity of GAMS as a brief measure of patient-reported migraine severity and identified clinic al and psycho social correlates and/or mediators of patient-reported severity of migraine in a cohort of migraine patients seen in an outpatient Headache clinic. The identified determinants can help health researchers design and implement targeted interventions, appropriate support services and adequate measures to improve disability in persons with migraine. In addition, a single-item global rating scale of migraine severity may be a rapid and efficient way for clinicians to obtain information about disease severity, but requires validation in future prospective studies.
