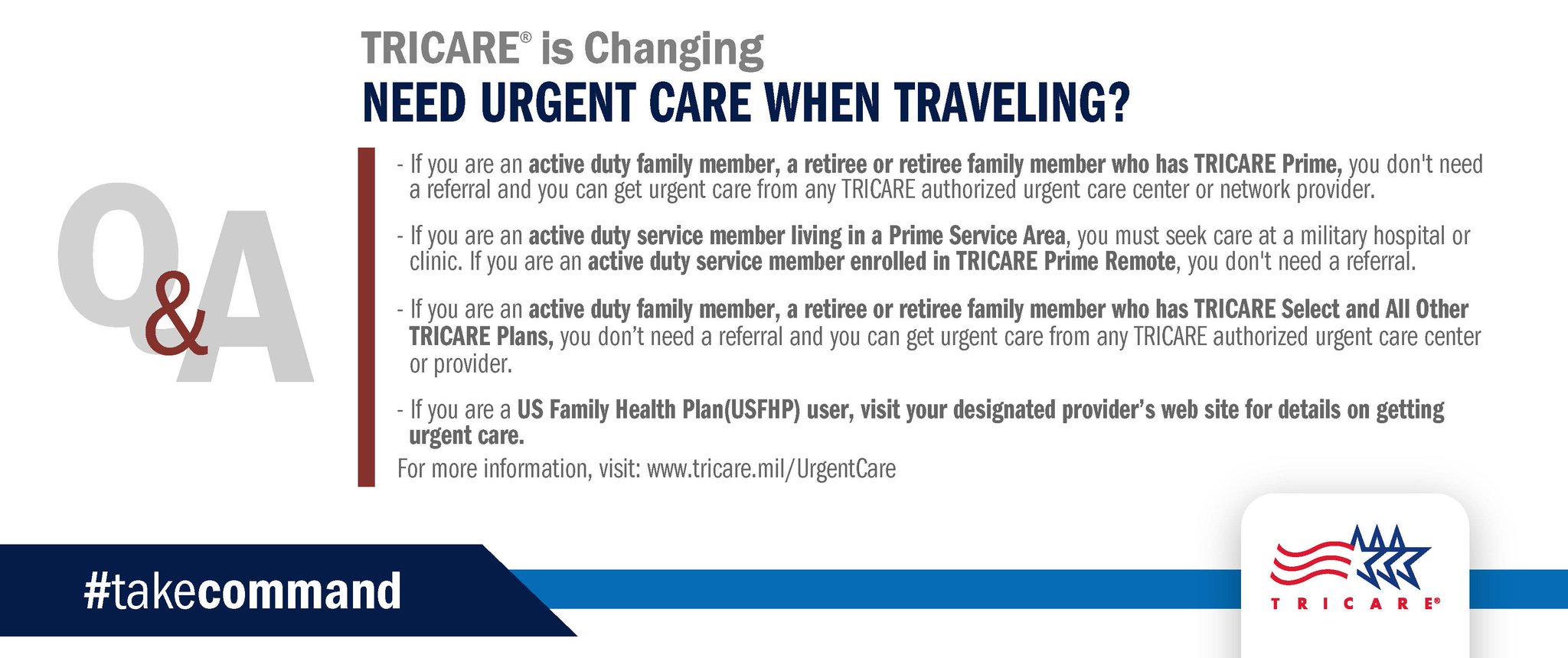
TRICARE requires a provider, typically your primary care manager or family doctor, to submit prior authorization and referral requests. Please contact your provider and have him or her submit your request. Why was I referred to a military hospital or clinic for care?
Full Answer
Does Tricare cover inpatient hospital services?
Emergency Services TRICARE covers emergency inpatient hospital services when: You have a medical or psychiatric emergency You need immediate hospital admission You will get treatment at the closest hospital that can provide your care. If you have a mental health or substance use disorder, we will cover emergency inpatient hospital services for:
What medications does Tricare cover?
TRICARE covers medications that are approved by the U.S. Food and Drug Administration. Injection/infusion medications may be self- or caregiver-administered, or administered by a home health agency, in a hospital, or in a provider’s office.
Do you need a referral for Tricare mental health?
Note: If you are an active duty service member (ADSM) seeking care in the TRICARE network, you must get a referral and pre-authorization. You don’t need a referral or pre-authorization if you seek outpatient mental health services at a military hospital or clinic.
Does Tricare cover intensive outpatient programs (IOP)?
TRICARE covers Intensive Outpatient Programs (IOPs). You may qualify for an IOP if you: Have a psychiatric or substance use disorder Don’t need to be in a hospital full-time
How do I get a TRICARE eligibility letter?
Family members can access only their own Eligibility Letters....Online RequestLog in to milConnect.Click on the “Obtain proof of health coverage” button.Or click on Correspondence/Documentation and choose "Proof of Coverage."Your coverage letter will be generated and available for download.
Does TRICARE require prior authorization for mental health?
You need to get a referral and pre-authorization for all mental health care in the TRICARE network. You don't need it if you seek outpatient mental health services at a military hospital or clinic.
Does TRICARE require a referral for psychiatrist?
Schedule an appointment with a network psychiatrist or psychologist in your region. You don't need a referral or pre-authorization for outpatient visits except for psychoanalysis and outpatient therapy for substance use disorder.
Can TRICARE be used for therapy?
Individual therapy: TRICARE covers psychotherapy sessions lasting up to 60 minutes, and up to 120 minutes for crises. Family therapy: TRICARE covers sessions lasting up to 90 minutes, and 180 minutes for crises. Group therapy: TRICARE covers sessions lasting up to 90 minutes.
Does TRICARE have a copay for mental health?
Mental health copays are now $30 per visit for TRICARE Prime Retirees, $31 for TRICARE Select ADFM, and $41 for TRICARE Select Retirees. These amounts are higher than those in high quality commercial plans.
Does TRICARE Prime require a prior authorization?
TRICARE Prime Overseas and TRICARE Prime Remote Overseas Active Duty Service Members (ADSMs) require prior authorization for all inpatient and outpatient specialty care services. An additional fitness-for-duty review is required for maternity care, physical therapy, mental health care services, and family counseling.
How do I get a TRICARE referral Online?
Beneficiaries must log in at www.tricare-west.com to view authorizations, referrals and individual Explanation of Benefits statements. HNFS posts these documents electronically to the Secure Inbox where they can viewed online and/or printed.
Does TRICARE cover anxiety?
TRICARE mental health and substance use disorder (SUD) services are available for you and your family during times of stress, depression, grief, anxiety, mental health crisis, or misuse or abuse of alcohol or drugs.
What doesn't TRICARE cover?
In general, TRICARE excludes services and supplies that are not medically or psychologically necessary for the diagnosis or treatment of a covered illness (including mental disorder), injury, or for the diagnosis and treatment of pregnancy or well-child care.
Does TRICARE cover virtual therapy?
YES! Tricare Select, Tricare Prime, or Tricare Prime-Remote all cover therapy services. Your benefits cover mental health services for active duty service members and their dependents.
What does TRICARE for Life pay for?
A: TFL is Medicare-wraparound coverage for TRICARE beneficiaries who have Medicare Part A and Part B. It's available worldwide and offers comprehensive health coverage, including prescription drug coverage under the TRICARE Pharmacy Program.
What does TRICARE pay therapists?
Tricare is a common health insurance in California, and individuals who have Tricare may wish to find therapists who are in-network with their health insurance. When you see a therapist who is in-network with Tricare, each session you'll pay only a copay, which typically ranges from $0-$75/session.
Do you need prior authorization for tricare?
You don’t need to get prior authorization for emergency services. But you do need approval for ongoing treatment. You do need prior authorization for non-emergency inpatient hospital services. Emergency Services. TRICARE covers emergency inpatient hospital services when:
Does Tricare cover hospital admission?
TRICARE covers emergency inpatient hospital services when: You have a medical or psychiatric emergency. You need immediate hospital admission. You will get treatment at the closest hospital that can provide your care.
What does "medically necessary" mean in tricare?
TRICARE covers services that are medically necessaryTo be medically necessary means it is appropriate, reasonable, and adequate for your condition. and considered proven. There are special rules or limits on certain services, and some services are excluded. Last Updated 9/22/2020.
Does Tricare cover self-injection?
TRICARE covers medications that are approved by the U.S. Food and Drug Administration. Injection/infusion medications may be self- or caregiver-administered, or administered by a home health agency, in a hospital, or in a provider’s office. See Home Infusion Therapy for information on medication coverage for self-injection/infusion in ...
How long does it take to report a hospital admission?
You don't need prior authorization. If admitted, call your regional contractor within 24 hours or the next business day. Admissions must be reported within 72 hours.
What is the primary payer for mental health care?
Use TRICARE For Life. Medicare is the primary payer for mental health care.
What is tricare.mil?
www.tricare.mil is an official website of the Defense Health Agency (DHA), a component of the Military Health System . TRICARE is a registered trademark of the Department of Defense (DoD), DHA. All rights reserved.
Does Tricare cover outpatient programs?
TRICARE covers Intensive Outpatient Programs (IOPs). You may qualify for an IOP if you: Have a psychiatric or substance use disorder . Don’t need to be in a hospital full-time. Need stabilization, symptom reduction, or prevention of relapse.
Who is a tricare authorized provider?
Getting Vaccines from a TRICARE-Authorized ProviderAn authorized provider is any individual, institution/organization, or supplier that is licensed by a state, accredited by national organization, or meets other standards of the medical community, and is certified to provide benefits under TRICARE.
Does Tricare cover travel?
TRICARE only covers these vaccines for active duty family members traveling with their sponsor on permanent change of duty station orders or other official travel. Claims must include a copy of the travel orders or other official documentation to verify the official travel requirement.
Does Tricare cover new shots?
TRICARE regularly adds coverage for new vaccines based on CDC recommendations. You can also talk to your provider or regional contractor to see if the vaccine you need is covered. Getting Vaccines at a Military Hospital or Clinic. Contact your local military hospital or clinic for vaccine instructions and availability.
Managed Care Support Contractors
Each TRICARE region Opens in TRICARE.mil website has its own managed care support contractor (MCSC) who is responsible for administering the TRICARE program in each region. The MCSCs establish the provider networks and conduct provider education.
TRICARE Provider Types
TRICARE defines a provider as a person, business, or institution that provides health care. Understanding the different TRICARE provider types will help you decide what type of TRICARE provider you want to be.
Network Providers
If you decide to become a network provider, you will sign a contractual agreement with the MCSC in your region Opens in TRICARE.mil website . You will: