
If you qualify for mAb treatment, there are three steps to get it:
- Test positive for COVID-19 sometime in the last 10 days.
- Get a referral for mAb treatment from your healthcare provider. If you do not have a healthcare provider, call the Combat COVID Monoclonal Antibodies Call Center at 1-877-332-6585 to find ...
- Locate an infusion center that’s available near you.
How effective is the monoclonal treatment?
Follow All monoclonal antibody (mAb) therapies are in limited supply, and not everyone will be eligible for treatment. A prescription from a healthcare provider is required to receive any mAb therapy. Variants, like Omicron, may have an impact on the effectiveness of mAb therapies.
Can monoclonal antibodies kill you?
Jan 06, 2022 · Individuals qualify for monoclonal antibody treatment if: they have tested positive for COVID-19, and; it has been 10 days or less since symptoms first started, and; they have other health conditions that put them at higher risk. Monoclonal antibody treatment is most effective when given early—and the sooner it is given, the better.
What are the dangers of monoclonal antibodies?
Get the most current list of billing codes, payment allowances, and effective dates for currently authorized monoclonal antibody products. Payment for Infusion at Home Beginning on May 6, 2021, Medicare established separate coding and payment for administering COVID-19 monoclonal antibody products through infusion in a patient’s home or residence.
Can you still get monoclonal antibodies?
Treatment with COVID-19 monoclonal antibodies is done through a one-time intravenous (IV) infusion. Another option for COVID-19 therapy is an antiviral called Remdesivir. Remdesivir is approved by the FDA and helps reduce the effects of COVID-19. Remdesivir is given by an intravenous (IV) infusion over three (3) consecutive days.
What is a monoclonal antibody for COVID-19?
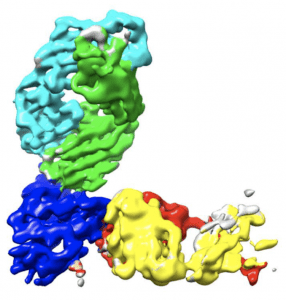
Monoclonal antibodies are laboratory-produced molecules that act as substitute antibodies that can restore, enhance or mimic the immune system's attack on cells. Monoclonal antibodies for COVID-19 may block the virus that causes COVID-19 from attaching to human cells, making it more difficult for the virus to reproduce and cause harm. Monoclonal antibodies may also neutralize a virus.Mar 31, 2022
How many types of monoclonal antibody COVID-19 treatments are there in the US?
In the United States, there are three anti-SARS-CoV-2 monoclonal antibody treatments with FDA Emergency Use Authorization (EUA) for the treatment of COVID-19: bamlanivimab plus etesevimab, casirivimab plus imdevimab,, and sotrovimab.
Can I get the COVID-19 vaccine if I was treated with monoclonal antibodies or convalescent plasma?
If you were treated for COVID-19 symptoms with monoclonal antibodies or convalescent plasma, you should wait 90 days before getting a COVID-19 vaccine.
What is the difference between monoclonal antibodies and the COVID-19 vaccine?
COVID-19 vaccines help stimulate and prepare a person's immune system to respond if they are exposed to the virus. However, monoclonal antibodies boost the immune system only after a person is already sick, speeding up their immune response to prevent COVID-19 from getting worse.Nov 8, 2021
What is the first drug that was approved by the FDA to treat COVID-19?
Remdesivir is the first drug approved by the FDA for treatment of hospitalized COVID patients over the age of 12.Jan 25, 2022
Which drug is approved by FDA to treat COVID-19?
Veklury (Remdesivir) is an antiviral drug approved for use in adults and pediatric patients [12 years of age and older and weighing at least 40 kilograms (about 88 pounds)] for the treatment of COVID-19 requiring hospitalization.Mar 31, 2022
Should you still get the COVID-19 vaccine if you were treated with monoclonal antibodies?
If you were treated for COVID-19 with monoclonal antibodies or convalescent plasma, there is no need to delay getting a COVID-19 vaccine.Feb 17, 2022
Do I need the COVID-19 vaccine if I still have antibodies?
Yes, the COVID-19 vaccines are recommended, even if you had COVID-19.Nov 23, 2021
What medication is not recommended before vaccinations for COVID-19?
It is not recommended you take over-the-counter medicine – such as ibuprofen, aspirin, or acetaminophen – before vaccination for the purpose of trying to prevent vaccine-related side effects. It is not known how these medications might affect how well the vaccine works.
What is a monoclonal antibody?
Monoclonal antibodies are laboratory-produced molecules that act as substitute antibodies that can restore, enhance or mimic the immune system's attack on cells.Mar 31, 2022
Can I get COVID-19 again after having the vaccine?
Getting COVID-19 after you've been vaccinated or recovered is still possible. But having some immunity -- whether from infection or vaccination -- really drops the odds of this happening to you.Nov 9, 2021
Who should not take the Pfizer-BioNTech COVID-19 vaccine?
If you have had a severe allergic reaction to any ingredient in the Pfizer-BioNTech COVID-19 vaccine (such as polyethylene glycol), you should not get this vaccine. If you had a severe allergic reaction after getting a dose of the Pfizer-BioNTech COVID-19 vaccine, you should not get another dose of an mRNA vaccine.
COVID-19 VEKLURYTM (remdesivir)
Following the recent statement from the National Institutes of Health (NIH) COVID-19 Treatment Guidelines Panel about therapies for the COVID-19 Omicron variant, CMS created HCPCS code J0248 for VEKLURY™ (remdesivir) antiviral medication when administered in an outpatient setting.
COVID-19 Monoclonal Antibody Products
The FDA authorized the following investigational monoclonal antibody product under EUA for pre-exposure prophylaxis of COVID-19:
Important Update about Viral Variants
On April 16, 2021, the FDA revoked the EUA for bamlanivimab, when administered alone , due to a sustained increase in COVID-19 viral variants in the U.S. that are resistant to the solo product.
Medicare Coverage for COVID-19 Monoclonal Antibody Products
During the COVID-19 public health emergency (PHE), Medicare will cover and pay for these infusions (when furnished consistent with their respective EUAs) the same way it covers and pays for COVID-19 vaccines.
Coding for the Administration of COVID-19 Monoclonal Antibody Products
CMS identified specific code (s) for each COVID-19 monoclonal antibody product and specific administration code (s) for Medicare payment:
Medicare Payment for Administering COVID-19 Monoclonal Antibody Products
To ensure immediate access during the COVID-19 PHE, Medicare covers and pays for these infusions and injections in accordance with Section 3713 of the Coronavirus Aid, Relief, and Economic Security Act (CARES Act) .
Billing for Administering COVID-19 Monoclonal Antibody Products
Health care providers can bill on a single claim for administering COVID-19 monoclonal antibody products, or submit claims on a roster bill.
What antibody is used to block the virus?
Monoclonal antibodies against COVID-19 attach to the virus to block it from entering human cells. The monoclonal antibody protein also “marks” the virus to be broken down by the immune system and cleared from the body.
What is the function of antibodies?
Antibodies are proteins that exist in our bodies as part of our immune system to recognize and defend against harmful viruses and bacteria. Monoclonal antibodies are made in a laboratory and designed to target a specific virus or bacteria.
Can monoclonal antibodies cause nausea?
Most people tolerate monoclonal antibody infusions very well. Some people may experience infusion-related side effects, such as nausea and dizziness, that are short-lived and go away on their own. As with any medication, there is the potential for mild or more severe allergic reactions, which are uncommon.
What is the FDA approved monoclonal antibody?
Department of Health and Human Services (HHS), two different monoclonal antibody treatments have been authorized for emergency use by the FDA. One is bamlanivimab, and the other is a mixture of casirivimab and imdevimab. Over 600,000 such treatments have been shipped to U.S. health care facilities.
Who is the chief science officer for the Biden administration?
Dr. David Kessler , chief science officer for the Biden administration's COVID response, has now said "it is very important" that Americans enquire about monoclonal antibodies if they test positive for coronavirus and fall into high-risk categories.
Is monoclonal antibody free?
The federal government is currently distributing monoclonal antibodies for free, but some health care providers may be charging patients for administering the treatment. These costs may be covered if the patient has insurance. If not, it is advised to ask the treatment facility if there will be any charges.
Monoclonal Antibody Therapy
Glaxo Smith Kline’s monoclonal antibody Sotrovimab is authorized for the treatment of mild-to-moderate coronavirus disease 2019 (COVID-19) in:
Preventative Monoclonal Antibody Therapy: EvuSheld
Preventative monoclonal antibody therapy locations are marked with a blue pin on the locator map.
