If you qualify for mAb treatment, there are three steps to get it:
- Test positive for COVID-19 sometime in the last 10 days.
- Get a referral for mAb treatment from your healthcare provider. If you do not have a healthcare provider, call the Combat COVID Monoclonal Antibodies Call Center at 1-877-332-6585 to find ...
- Locate an infusion center that’s available near you.
How effective is the monoclonal treatment?
Apr 07, 2022 · Follow All monoclonal antibody (mAb) therapies are in limited supply, and not everyone will be eligible for treatment. A prescription from a healthcare provider is required to receive any mAb therapy. Variants, like Omicron, may have an impact on the effectiveness of mAb therapies.
Can monoclonal antibodies kill you?
Jan 06, 2022 · Individuals qualify for monoclonal antibody treatment if: they have tested positive for COVID-19, and; it has been 10 days or less since symptoms first started, and; they have other health conditions that put them at higher risk. Monoclonal antibody treatment is most effective when given early—and the sooner it is given, the better.
How often can you get monoclonal antibodies?
Get the most current list of billing codes, payment allowances, and effective dates for currently authorized monoclonal antibody products. Payment for Infusion at Home Beginning on May 6, 2021, Medicare established separate coding and payment for administering COVID-19 monoclonal antibody products through infusion in a patient’s home or residence.
What are the dangers of monoclonal antibodies?
Treatment with COVID-19 monoclonal antibodies is done through a one-time intravenous (IV) infusion. Another option for COVID-19 therapy is an antiviral called Remdesivir. Remdesivir is approved by the FDA and helps reduce the effects of COVID-19. Remdesivir is given by an intravenous (IV) infusion over three (3) consecutive days.
How many types of monoclonal antibody COVID-19 treatments are there in the US?
In the United States, there are three anti-SARS-CoV-2 monoclonal antibody treatments with FDA Emergency Use Authorization (EUA) for the treatment of COVID-19: bamlanivimab plus etesevimab, casirivimab plus imdevimab,, and sotrovimab.
What is a monoclonal antibody for COVID-19?
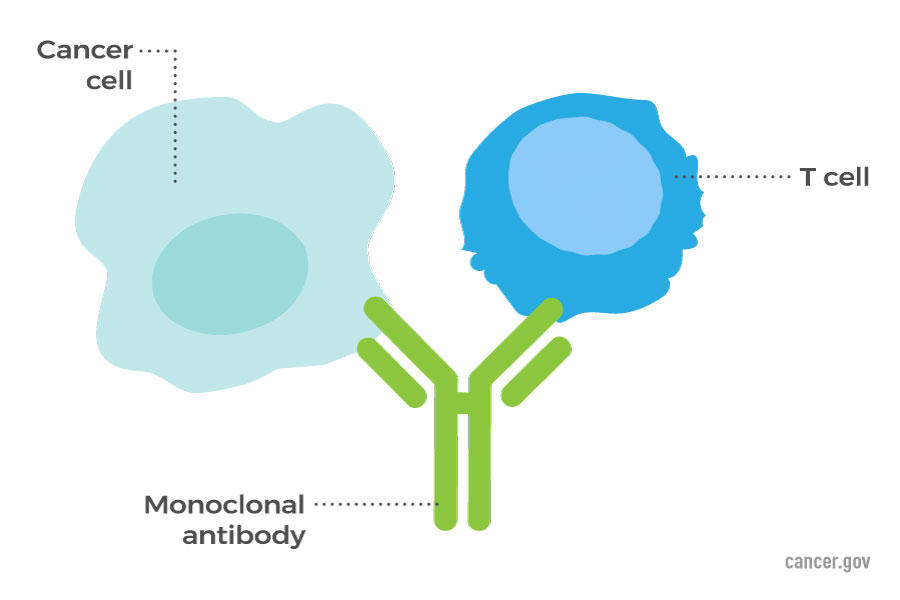
Monoclonal antibodies are laboratory-produced molecules that act as substitute antibodies that can restore, enhance or mimic the immune system's attack on cells. Monoclonal antibodies for COVID-19 may block the virus that causes COVID-19 from attaching to human cells, making it more difficult for the virus to reproduce and cause harm. Monoclonal antibodies may also neutralize a virus.Mar 31, 2022
Can I get the COVID-19 vaccine if I was treated with monoclonal antibodies or convalescent plasma?
If you were treated for COVID-19 symptoms with monoclonal antibodies or convalescent plasma, you should wait 90 days before getting a COVID-19 vaccine.
Will monoclonal antibodies provide immunity against COVID-19?
COVID-19 vaccines help stimulate and prepare a person's immune system to respond if they are exposed to the virus. However, monoclonal antibodies boost the immune system only after a person is already sick, speeding up their immune response to prevent COVID-19 from getting worse.Nov 8, 2021
What is a monoclonal antibody?
Monoclonal antibodies are laboratory-produced molecules that act as substitute antibodies that can restore, enhance or mimic the immune system's attack on cells.Mar 31, 2022
What is the difference between monoclonal antibodies and the COVID-19 vaccine?
COVID-19 vaccines help stimulate and prepare a person's immune system to respond if they are exposed to the virus. However, monoclonal antibodies boost the immune system only after a person is already sick, speeding up their immune response to prevent COVID-19 from getting worse.Nov 8, 2021
Should you still get the COVID-19 vaccine if you were treated with monoclonal antibodies?
If you were treated for COVID-19 with monoclonal antibodies or convalescent plasma, there is no need to delay getting a COVID-19 vaccine.Feb 17, 2022
Do I need the COVID-19 vaccine if I still have antibodies?
Yes, the COVID-19 vaccines are recommended, even if you had COVID-19.Nov 23, 2021
What medication is not recommended before vaccinations for COVID-19?
It is not recommended you take over-the-counter medicine – such as ibuprofen, aspirin, or acetaminophen – before vaccination for the purpose of trying to prevent vaccine-related side effects. It is not known how these medications might affect how well the vaccine works.
How do you build an immunity against COVID-19?
Vaccinations are the best option to developing immunity against the new coronavirus. In addition, the hope is that people who've been exposed to COVID-19 also develop an immunity to it. When you have immunity, your body can recognize and fight off the virus.Jan 21, 2022
Are antibiotics effective in preventing or treating COVID-19?
Antibiotics do not work against viruses; they only work on bacterial infections. Antibiotics do not prevent or treat COVID-19, because COVID-19 is caused by a virus, not bacteria. Some patients with COVID-19 may also develop a bacterial infection, such as pneumonia.Mar 31, 2022
What are some ways to strengthen your immune system helping to prevent COVID-19?
Vaccines are the single best way to strengthen your immune system and help prevent the flu and COVID-19 and the potentially life-threatening complications these viruses can cause. Good nutrition—including adequate hydration—is also a great way to give your immune system a boost and help you stay well.Feb 2, 2022
What is the function of antibodies?
Antibodies are proteins that exist in our bodies as part of our immune system to recognize and defend against harmful viruses and bacteria. Monoclonal antibodies are made in a laboratory and designed to target a specific virus or bacteria.
Does infusion cause nausea?
Some people may experience infusion-related side effects, such as nausea and dizziness, that are short-lived and go away on their own. As with any medication, there is the potential for mild or more severe allergic reactions, which are uncommon.