
You can then download or print the PDFs out for your records, or automatically send a copy to the patient via email. Have patients fill out their information on a computer or tablet using an online Dental Health Record Form, then use PDF Editor to easily format the data into a polished PDF document for the patient’s file.
Full Answer
What information should be included in the dental record?
The information in the dental record should primarily be clinical in nature. The record includes a patient’s registration form with all the basic personal information. The dental team should be very meticulous and thorough in the dental office record keeping tasks.
What is the purpose of Dental Record Management?
Record Management. The recording of accurate patient information is essential to dentistry. The dental record, also referred to as the patient chart, is the official office document that records all diagnostic information, clinical notes, treatment given, and patient-related communications that occur in the dental office,...
Do dentists use computerized filing systems to maintain patient dental records?
However, many more dentists are making use of computerized filing systems to maintain patient dental records. Electronic records have great quality and patient-safety benefits, and will likely increase as more dental clinics and hospitals become computerized.
Why are complete and accurate dental records important?
Complete and accurate records allow providers who do not know the patient to become familiar with the individual’s dental history and experience while under your care. Consider these tips before making entries in the dental record:
How do you write dental records?
Information typically noted in the dental record includes:personal data, such as the patient's name, birth date, address and contact information including home, work and mobile telephone numbers.the patient's place of employment.medical and dental histories, notes and updates.progress and treatment notes.More items...
How do you present a dental treatment plan?
4:256:26How to present dental treatment plans and why this presentation is so ...YouTubeStart of suggested clipEnd of suggested clipUnderstanding the patient needs to understand. And then doing it in an environment where the patientMoreUnderstanding the patient needs to understand. And then doing it in an environment where the patient is most comfortable. So that we can help them. Make the best decision.
What information is recorded in a patient's dental history?
Dental records, also known as patient charts, are made up of the recorded information regarding your medical history, diagnostic information, clinical notes, patient-doctor communication, consent to treatment documents and treatment notes, as the American Dental Association (ADA) explains.
What is an example of an important record in a dental office?
Useful records include employment applications, expired insurance policies, petty cash vouchers, bank reconciliations, and general correspondence. This category is difficult to define, because one office may consider a document useful, whereas another might find it indispensable.
What is a treatment presentation?
The first step in a treatment presentation (in particular, an elective one) is to evaluate the patient's motivation level. Once the patient has demonstrated interest, you can then create excitement by offering an enthusiastic presentation that will help the patient recognize the benefits of treatment.
When is a treatment plan presented to the patient in dentistry?
It is during the sequencing stage that a dentist will flex their ability to handle complex issues and distill them into a comprehensive plan of action. To organize the stages into a proper sequence of treatments, a dentist should: Review the stages and the different treatments they plan to use.
What are the components of a medical dental record?
Dental records consist of documents related to the history of present illness, clinical examination, diagnosis, treatment done, and the prognosis.
What should not be included in a patient medical record?
The following is a list of items you should not include in the medical entry:Financial or health insurance information,Subjective opinions,Speculations,Blame of others or self-doubt,Legal information such as narratives provided to your professional liability carrier or correspondence with your defense attorney,More items...•
What should be written on dental notes?
Record all treatment provided, the taking of consent, treatment discussions, advice given about oral hygiene, advice about treatment options, aftercare and both positive and salient negative findings (remember that negative results may be as important as positive ones). Use only universally agreed dental abbreviations.
Why is record keeping so important in dentistry?
Accurate dental records can help practitioners to reach a diagnosis by providing detailed information about a patient's changing oral health. Detailed records can also help to prevent adverse incidents, for example, if the records are not clear the wrong tooth could be treated.
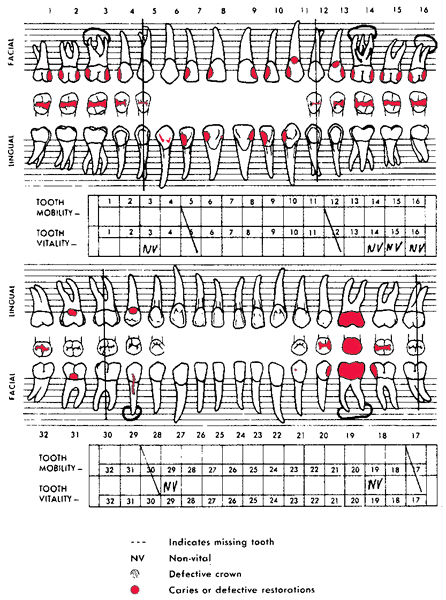
Why is charting important in dental?
The chart gives both you and your dentist a point of reference to see if you're making progress in your dental health. With better home care, for example, gum pockets could improve. They are able to keep an organized and easy-to-read record of the condition of your mouth.
Why is dental recording system important in dental practice?
Beyond providing patient care, the dental record is important because it may be used in a court of law to establish the diagnostic information that was obtained and the treatment that was rendered to the patient. It can be used in defense of allegations of malpractice.
How long do you have to keep dental records?
How long do we have to keep dental records? In general, clinical and financial records, as well as radiographs, consultation reports, and drug and lab prescriptions must be maintained for at least ten years after the date of the last entry in the patient’s record.
Why is a dental record important?
Beyond patient care, the dental record is important because it may be used as evidence in court or in a regulatory action to establish the diagnostic analysis that was performed and what treatment was rendered to the patient.
Why is it important to record patient information?
The dental record (aka patient chart) is the official source of all diagnostic information, clinical notes, treatment and patient-related communications that occur in the dental office, including instructions for home care, consent to treatment and finances. It provides invaluable data, which can be used to assess the quality of care that has been provided and to properly plan for treatment going forward.
What happens if a chart doesn't justify the claim submitted?
by insurance companies). If the chart doesn’t justify the claim submitted, an insurance company might refuse payment or demand reimbursement. This will certainly lead to an upset patient, and if there is a serious discrepancy between the progress notes and the bill submitted, fraud might be suspected. In these situations, insurance companies could audit your records or even report you to the College. Keeping good records helps avoid this unnecessary stress. For example:
Do electronic records leave an audit trail?
Electronic records must leave an audit trail that accomplishes the same result. Late entries should be clearly marked as such. In no circumstances should a clinician add to or correct a patient’s chart after receiving a demand for compensation or notice of legal proceedings.
When should progress notes be completed?
Because they are essential for treatment continuity, progress notes should be completed during or immediately after each visit and must be reviewed and approved by the treating clinician.
Can Zirconoia crown be retroactively altered?
If you provide a Zirconoia crown and accidentally submit the code for a PFM, you might be accused of insurance fraud or overbilling. Never, never retroactively alter the patient chart. To avoid allegations of tampering, errors or incorrect information should never be erased or eliminated from the chart.
What is a dental health record template?
The Dental Health Record Template is easy for patients to fill out and designed to get the doctor the most important information. Patients can fill out their information on a computer or tablet using our Dental Health Record Template.
Why use a medical history record PDF?
Medical History Record PDF template is mostly used in order to provide significant information about the health history, care requirements, and risk factors of the patient to doctors. It is for collecting data from the patients.
What is an occupational first aid assessment?
An Occupational First Aid Patient Assessment is a document that puts into record the injuries or signs or symptoms of diseases provided by the patient or his or her companion. This is recorded by an attendant and the records of such must be kept for historical purposes.This Occupational First Aid Patient Assessment PDF template is your easy to use document for your company. It contains the necessary questions required for a first aid assessment in order to help medical practitioners immediately see the information of their patients or for them to immediately get a lead of the patient's illness or injury.
What is a first aid incident report?
The First-Aid Incident Report template contains injured person's personal details and contact details, the details and visible symptoms of injury, the Glasgow Coma Scale which is a neurological scale that expects to give a dependable and target method for chronicle the condition of an individual's awareness and brief information of treatment. Also, it contains the profile of the first-aider and signature of the person who prepares the report. Plus, JotForm is HIPAA-compliant and that is gigantic in addition to for anybody in the medicinal services industry.
What is a medical history document?
A comprehensive document providing the patients’ past medical history, personal and contact details, health information, habits, living standards and family medical history with their consent to the terms and conditions.
Can you record medical history as a PDF?
Once you have collected these medical data, you can record them as a pdf by using this medical history PDF template. In addition, you don't need to be worried about the safety of data, because our forms are HIPAA compliant.
Is jotform HIPAA compliant?
JotForm is HIPAA-compliant and that ’s a huge plus for anyone in the healthcare industry. So, aside from these PDF templates that were pre-built and designed for you, you also enjoy the advantages of using a platform that’s HIPAA-compliant. Read More….
What are the requirements for a medical history?
Medical and dental history ( P resenting conditions)#N#Current thinking on a proper patient medical history says the following should be included: 1 Comprehensive information collection, including systemic diseases, allergies, and medications. 2 Name and phone number of patient’s medical doctor. 3 Appropriate medical alert that makes medical concerns obvious (red sticker, red circle, highlighted area, etc.). 4 Baseline blood pressure and pulse documentation section. 5 Dentist review section with the dentist’s comments and signature (or personalized electronic code) in addition to the patient’s signature. 6 Updated at least once a year, or more if there is a significant change in the patient’s health.
How many carpules of anesthetic are used for each restoration?
For example, some digitized “macros” include one to two carpules of anesthetic for each restoration. This could result in a patient’s digitized record showing six carpules of anesthetic for restorations on tooth Nos. 2, 3, and 4, when only two carpules may have actually been used.
Where should a written fee estimate be kept?
This way everyone knows what is expected financially. A copy should be kept in the patient’s paper record or in the digitized file, and the patient should have a copy to take home.
Can a patient's information be merged with a chart?
Digital files, such as radiographs, may or may not be possible to be merged with a Web-based chart.
Is consent a form?
Consent is a process, not just a form. However, even though consent can simply be acknowledged in the patient’s progress notes, a detailed, treatment-specific, patient-signed-and-dated form focuses on the fact that a treatment has been explained and agreed to.
Is a dental appointment a legal document?
While correct documentation of a patient’s dental appointment is essential, it is not the only reason for a visit. It is true that we must be concerned about accuracy and completeness, as well as the importance of the dental record as a legal document. Also, most issues with insurance carriers hinge on accurate records.
Purpose
To establish uniform procedures detailing the responsibilities of dental providers (including Employee, Faculty, Affiliate Faculty, Pre-doctoral and Graduate Students) who administer treatment to patients of record within the School of Dentistry (herein referred to as “SOD”) to compile and maintain patient treatment records.
General Policy
The SOD employs a patient Electronic Health Record (herein referred to as “EHR”) system called axiUm and a patient radiograph record system called “MiPACS.” [1] Dental providers engaged in all levels of patient related clinical activity must adhere to strict policy guidelines and regulatory requirements when entering patient treatment notes and records in axiUm and MiPACS..
Implementation
Washington state law governing the “Maintenance and Retention of Records” requires that dentists compile and maintain comprehensive and dated patient treatment records.
How long do dental records need to be kept?
There is usually a different requirement for the retention of records of children; these records must be kept for a certain period after the child reaches the age of majority. HIPAA also affects recordkeeping requirements for offices that are covered by generally requiring that such offices maintain patient records for six (6) years and two (2) years after a patient’s death. The dental office should have a records retention policy and all staff should understand it. The office’s professional liability insurance company will likely have recommendations about retention.
What is the obligation of destroying dental records?
Confidential information is included in the dental record. You have an obligation to protect the patient’s privacy and personal health and financial information.
What happens if a patient refuses a dental treatment?
If the patient refuses the proposed treatment, the dentist must inform the patient about the consequences of not accepting the treatment and get a signed informed refusal. However, obtaining an informed refusal does not release the dentist from the responsibility of providing a standard of care. If, for example, the patient refuses to have radiographs taken, the dentist should refer the patient to another dentist when the original dentist believes that radiographs are a necessary prerequisite to proper care in that case.
What is informed consent?
What exactly is informed consent? In general, it is required that dentists provide information to patients about the dental health problems that the dentist observes, the nature of any proposed treatment, the potential benefits and risks associated with that treatment, any alternatives to the treatment proposed, and the potential risks and benefits of alternative treatments, including no treatment. Some procedures call for a separate consent form to be signed, but there are many times when procedures and options are discussed and a consent form may not be utilized. In some offices, notes of the discussion with the patient are entered in the record at the time the discussion is held and the patient is asked to initial the entry.
What is a dental chart?
The dental record, also referred to as the patient's chart, is the official office document that records all of the treatment done and all patient-related communications that occur in the dental office. State and federal laws or regulations determine how it is handled, how long it is kept and who may have access to the information. The dental record provides for continuity of care for the patient and is critical in the event of a malpractice insurance claim. This publication will provide some helpful information but the first step should be to review your state dental practice act.
What is ADA dental records?
This ADA publication is designed especially for dentists and the dental team to provide helpful information about the dental record. This publication is not intended or offered as legal or other professional advice. Laws vary from state to state and thus, readers should consult with their personal legal counsel and malpractice insurer to access the applicable laws in their state. Dental Records is based in part on questions frequently asked by our members. It is our hope that dentists and their team members will find this publication, helpful but in no way a substitute for actual legal advice given by an attorney in your state.
Why is communication important in dentistry?
Patients should receive clear, consistent information about their dental problems and treatment from all dental professionals. Mixed messages can confuse and frustrate patients. The following steps can facilitate the communication process:
What is dental chart?
A dental chart is a permanent record of a patient’s dental care, and completion of a dental chart is the minimum standard of care for documenting any pro- fessional dental procedure.
What does BUC/LIP/X 105/205 mean?
Practitioners who perform infiltration nerve blocks be- fore extracting wolf teeth can abbreviate the procedure as BUC/LIP/X 105/205 to indicate that a buccal local infiltration anesthesia, local infiltration anesthesia of the palate, and simple extraction of.
Why is electronic dental records important?
Electronic dental records, computerized systems, and paper charts must all include certain key elements to make them thorough, accurate, and defensible. One of the most important aspects of a patient record is an updateable medical history. Here we strive for simplicity and accuracy. It is also imperative that a chart as a whole lends itself ...
Why should a label be placed on a penicillin record?
For example, instead of writing "allergy to penicillin" on the outside of a record, a label should be placed that indicates providers need to check the patient's medical history prior to treatment. Patient safety is as important as privacy.
What is an acknowledgement of receipt of notice of privacy practices?
A dental office needs to make a good faith effort to obtain a signature on an "Acknowledgement of Receipt of Notice of Privacy Practices.". Detailed record keeping and an updateable medical history are important to every dental practice, regardless of whether the office is using paper or computerized charts.
What is an update in medical history?
An update can be part of a medical history form, or simply noted in the progress notes. It should reflect any changes or that there are no changes. • The format should be proactive. In other words, the patient should be able to indicate with yes or no what conditions apply to him/her.
What is the job of a dental assistant?
It is typically the dental assistant's task to make sure that all sections of the history have been addressed. Conditions that should be brought to the dentist's attention can be highlighted in yellow on a paper form, or otherwise computer-identified.
What is the privacy policy for dental offices?
2. A dental office needs to provide a copy of the privacy policy to all staff and document that it has been distributed. 3. A dental office needs to select a privacy officer who will make many of the decisions involved in implementing the office's privacy policy.
Is a medical history format out of date?
Medical history formats that are even six months old can be out of date. Personalized entries are important. Computer systems that do not allow for individual remarks and explanations limit the types of conditions that can be noted. Prewritten templates or cut-and-paste functions are usually not patient specific.
