- Record the treatment plan's components. The treatment plan will consist of the goals that the counselor and therapist has decided on.
- Record the goals. Your goals need to be as clear and concise as possible. Remember the SMART goals plan and make each goal specific, measurable, achievable, realistic, and time-limited.
- Express specific interventions you will use. The counselor will include treatment strategies the client has agreed to.
- Sign the treatment plan. Both the client and the counselor sign the treatment plan to show that there is an agreement on what to focus on in treatment.
- Review and improve as needed. You will be expected to complete goals and make new ones as the client progresses in treatment.
- The patient's personal information, psychological history and demographics.
- A diagnosis of the current mental health problem.
- High-priority treatment goals.
- Measurable objectives.
- A timeline for treatment progress.
How do you develop a comprehensive treatment plan?
Click here to see the meta data of this asset. Developing a comprehensive treatment plan follows a thorough assessment. The assessment will normally consist of a psychosocial assessment completed by the MMT counsellor, supplemented by a medical examination by the attending physician.
How do I write a treatment plan for my client?
Goals (or objectives) Every good treatment plan starts with a clear goal (or set of goals). Identify what your client would like to work on and write it down. Don't be scared of limiting your work, you can always adjust these as time goes on. However, it's helpful to write down and discuss what your client's purpose is for starting therapy.
What makes a good treatment plan?
Every good treatment plan starts with a clear goal (or set of goals). Identify what your client would like to work on and write it down. Don't be scared of limiting your work, you can always adjust these as time goes on.
How do you create a mental health treatment plan?
Create a Mental Health Treatment Plan With ICANotes Electronic health record (EHR) software allows medical professionals to store vital documents, such as treatment plans, evaluations and discharge summaries digitally in an organized, user-friendly format. ICANotes is EHR software designed specifically for the behavioral health field.
What are the four components of the treatment plan?
There are four necessary steps to creating an appropriate substance abuse treatment plan: identifying the problem statements, creating goals, defining objectives to reach those goals, and establishing interventions.
What does a counseling treatment plan look like?
A counseling treatment plan is a document that you create in collaboration with a client. It includes important details like the client's history, presenting problems, a list of treatment goals and objectives, and what interventions you'll use to help the client progress.
How many steps are there in the treatment planning process?
How To Write A Treatment Plan For Substance Use In 4 Steps. Treatment planning is an important part of the therapeutic process for individuals and the families that we serve. The treatment plans you write serve as roadmaps for the clients' recovery process while in your care.
What are goals in a treatment plan?
Treatment goals: Goals are the building blocks of the treatment plan. They are designed to be specific, realistic, and tailored to the needs of the person in therapy. The language should also meet the person on their level.
What is a comprehensive treatment plan?
Every patient needs individually tailored treatment. When a mental health professional creates a comprehensive treatment plan specially designed to meet their patient's needs, they give their patient directions towards growth and healing.
How do you write a treatment plan example?
Treatment plans usually follow a simple format and typically include the following information:The patient's personal information, psychological history, and demographics.A diagnosis of the current mental health problem.High-priority treatment goals.Measurable objectives.A timeline for treatment progress.More items...
What is a smart treatment plan?
S.M.A.R.T. Treatment Planning The treatment plan addresses problems identified in the client assessment, defines and measures interventions in their care and provides a measure for client's progress in treatment.
How do you write a treatment summary?
How To Write A Therapy Case Summary1 | Therapy Case History. ... 2 | Systemic Client Assessment. ... 3 | Treatment Focus and Progress. ... 4 | Client Strengths and Supports. ... 5 | Evaluation.
How long does it take to create a treatment plan?
Treatment plans are usually updated on a regular basis, often every six months or so, to allow for changes in your priorities and to reflect on the progress you have made.
What are the 5 smart goals?
The SMART in SMART goals stands for Specific, Measurable, Achievable, Relevant, and Time-Bound.
What are the steps needed to develop a systematic treatment plan for a client?
These domains include: (1) patient predisposing qualities, (2) treatment context, (3) relationship variables, and (4) intervention selection. These main principles provide the basis for which guidelines have been developed to systematically individualize treatment plans.
SHOW-NOTES (transcript)
Hi, Patrick Martin here, and in this post I will be sharing with you how to create a CBT treatment plan and this is the second part of the clinical loop.
Create A Treatment Plan Using The S.M.A.R.T. Model
Alright, another acronym that can help us out complements the smart model, and this is known as the P.O.W.E.R. model.
Final Thoughts On Creating A Treatment Plan
So, when it comes to making measurable goals right, those objectives we can use some tools and counseling to help us do that.
What is treatment planning?
Treatment planning is a team effort between the patient and health specialist. Both parties work together to create a shared vision and set attainable goals and objectives.
What is the third section of a treatment plan?
Problems and goals: The third section of the treatment plan will include issues, goals, and a few measurable objectives. Each issue area will also include a time frame for reaching goals and completing objectives. Counselors should strive to have at least three goals.
What information do counselors fill out?
Patient information: At the top of the treatment plan, the counselor will fill in information such as the patient’s name, social security number, insurance details, and the date of the plan. Diagnostic summary: Next, the counselor will fill out a summary of the patient’s diagnosis and the duration of the diagnosis.
What is a goal in a patient's life?
Both parties work together to create a shared vision and set attainable goals and objectives. A goal is a general statement of what the patient wishes to accomplish. Examples of goals include: The patient will learn to cope with negative feelings without using substances.
What is objective in a patient?
An objective, on the other hand, is a specific skill a patient must learn to reach a goal. Objectives are measurable and give the patient clear directions on how to act.
What is the role of model and technique in a treatment plan?
Treatment plans provide structure patients need to change. Model and technique factors account for 15 percent of a change in therapy. Research shows that focus and structure are critical parts of positive therapy outcomes. Goal-setting as part of a treatment plan is beneficial in itself. Setting goals helps patients:
Do mental health professionals have to make treatment plans?
Although not all mental health professionals are required to produce treatment plans, it’s a beneficial practice for the patient. In this article, we’ll show you why treatment plans are essential and how to create treatment plans that will make a difference in your and your patient’s lives.
What is a comprehensive treatment plan?
When a mental health professional creates a comprehensive treatment plan specially designed to meet their patient’s needs, they give their patient directions towards growth and healing.
What is a treatment plan?
A treatment plan is a detailed plan tailored to the individual patient and is a powerful tool for engaging the patient in their treatment. Treatment plans usually follow a simple format and typically include the following information: The patient’s personal information, psychological history and demographics.
What is the role of a counselor in a treatment plan?
A counselor must use their skills to help a client establish the best goals and objectives for their unique condition. Counselors can ask themselves these questions to help uncover the best goals for their patients:
What is the goal of a mental health treatment plan?
Both parties work together to create a shared vision and set attainable goals and objectives. A goal is a general statement of what the patient wishes to accomplish .
How to evaluate the effectiveness of a treatment plan?
To evaluate the effectiveness of the treatment plan, you need to keep score of how the patient is doing. Ask the patient to count and keep track of their thoughts, feelings and behaviors in a log so you can monitor their progress.
When is a discharge summary needed?
When patients are ready to leave a treatment program, a discharge summary is needed to document how the patient completed treatment and what their plan for continuing care is. A treatment plan can guide the writing process when it’s time to produce an accurate, detailed discharge summary.
Why do treatment plans go hand in hand with progress notes?
2. Progress Notes. Treatment plans and progress notes tend to go hand in hand because progress notes need to incorporate one or more treatment objectives.
How to start a treatment plan?
Every good treatment plan starts with a clear goal (or set of goals). Identify what your client would like to work on and write it down. Don't be scared of limiting your work, you can always adjust these as time goes on. However, it's helpful to write down and discuss what your client's purpose is for starting therapy.
Is treatment plan more meaningful than term paper?
Without their feedback, your treatment plan is no more meaningful than a term paper with a bunch of words on it. Remember, your documentation serves you and the client, not the other way around! This is an ongoing conversation to have throughout treatment.
Is therapy hard work?
Therapy is often hard work but can have amazing results. However, success is 100% dependent on the client's motivation and willingness to engage in the process. 3. Support. Another aspect of treatment planning that is so often forgotten in private practice settings is the client's support system.
Why do we need treatment plans?
Treatment plans can reduce the risk of fraud, waste, abuse, and the potential to cause unintentional harm to clients. Treatment plans facilitate easy and effective billing since all services rendered are documented.
What is a mental health treatment plan?
At the most basic level, a mental health treatment plan is simply a set of written instructions and records relating to the treatment of an ailment or illness. A treatment plan will include the patient or client’s personal information, the diagnosis (or diagnoses, as is often the case with mental illness), a general outline ...
What is the treatment contract?
Treatment Contract – the contract between the therapist and client that summarizes the goals of treatment. Responsibility – a section on who is responsible for which components of treatment (client will be responsible for many, the therapist for others)
What is the part of effective mental health?
Part of effective mental health treatment is the development of a treatment plan. A good mental health professional will work collaboratively with the client to construct a treatment plan that has achievable goals that provide the best chances of treatment success. Read on to learn more about mental health treatment plans, how they are constructed, ...
What is intervention in therapy?
Interventions – the techniques, exercises, interventions, etc., that will be applied in order to work toward each goal. Progress/Outcomes – a good treatment plan must include space for tracking progress towards objectives and goals (Hansen, 1996)
What is blended care in therapy?
Blended care involves the provision of psychological services using telecommunication technologies.
What is a goal in counseling?
Goals are the broadest category of achievement that clients in mental health counseling work towards. For instance, a common goal for those struggling with substance abuse may be to quit using their drug of choice or alcohol, while a patient struggling with depression may set a goal to reduce their suicidal thoughts.
Why do people need treatment plans?
Treatment plans can also be applied to help individuals work through addictions, relationship problems, or other emotional concerns. While treatment plans can prove beneficial for a variety of individuals, they may be most likely to be used when the person in therapy is using insurance to cover their therapy fee.
Why are treatment plans important?
Treatment plans are important for mental health care for a number of reasons: Treatment plans can provide a guide to how services may best be delivered. Professionals who do not rely on treatment plans may be at risk for fraud, waste, and abuse, and they could potentially cause harm to people in therapy.
What is HIPAA treatment plan?
Treatment Plans and HIPAA. The Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule grants consumers and people in treatment various privacy rights as they relate to consumer health information, including mental health information.
What is a mental health treatment plan?
Mental health treatment plans are versatile, multi-faceted documents that allow mental health care practitioners and those they are treating to design and monitor therapeutic treatment. These plans are typically used by psychiatrists, psychologists, professional counselors, therapists, and social workers in most levels of care.
What does a therapist do for Chris?
Therapist will provide psychoeducation on positive parenting and will support Chris in developing a concrete parenting plan. Therapist will provide materials for Chris to document the new house rules, rewards, and consequences system.
What is progress and outcomes?
Progress and outcomes of the work are typically documented under each goal. When the treatment plan is reviewed, the progress sections summarize how things are going within and outside of sessions. This portion of the treatment plan will often intersect with clinical progress notes.
Do you need a treatment plan for a 3rd party?
Treatment plans are required if you accept 3rd party reimbursement and are just good practice. They are a road map to treatment. They are fluid and are developed with the client/patient. Pretty much necessary if you are doing your job as a therapist.
How to share a treatment plan?
To share a Treatment Plan: Click Patients > Patient Name > Documents tab. Click on the name of the Treatment Plan. Click the Share on Portal button. Under Documents Included in Request , Request signature is selected by default for the Treatment Plan. If you do not need your client's signature, deselect this option.
What happens if an intake note is completed prior to the creation of the treatment plan?
If an Intake Note was completed prior to the creation of the Treatment Plan, the Presenting Problem will automatically pull forward into the Treatment Plan. Otherwise, enter the reason for treatment.
Do you need an intake note for a treatment plan?
Note: An Intake is not needed if you complete a Treatment Plan. TherapyNotes will prompt you to create a Treatment Plan after you create an Intake Note for a client and will generate a To-Do list item as a reminder to create a Treatment Plan for the client.
Do you need a treatment plan before a therapy session?
Because of this, a Treatment Plan must be completed prior to completing a Progress Note for a client's first scheduled Therapy Session. If you do not want to write a Treatment Plan before the first appointment with a client, you can schedule a Consultation or Psychotherapy Intake and subsequently write either a Consultation or Psychotherapy Intake ...
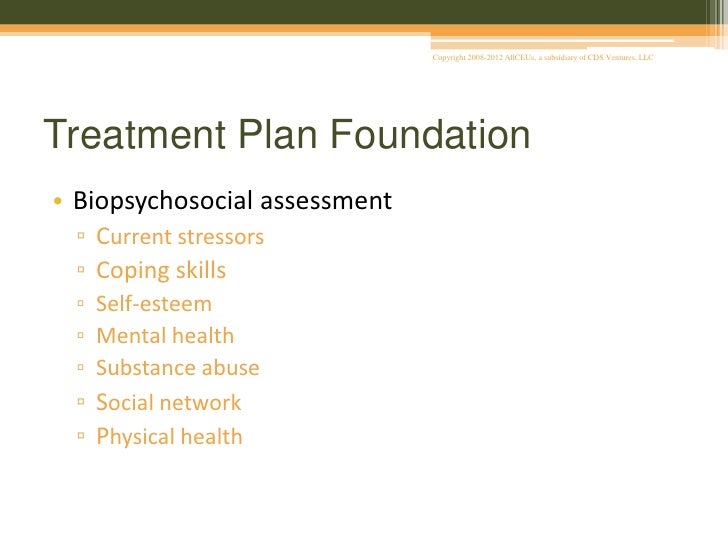
Psychosocial Assessment
- It is advisable for clients to complete a psychosocial assessment as soon as possible upon entry to methadone treatment and not later than four weeks after admission. In preparation, clients should be fully informed about the nature and purpose of the assessment process and should be clear about how the information gleaned from the assessment will ...
Problem Identification
- The problem areas listed below in the assessment checklist should be covered in the comprehensive psychosocial assessment, as well as any other areas that appear relevant.
Assessment Instruments
- A comprehensive psychosocial assessment can include the application of structured assessment tools. The assessment instruments identified for use in Ontario substance abuse treatment services are suitable for use in MMT programs. These include tools to assess drug use history, adverse consequences of drug use, problem behaviours and symptoms, perceived social suppor…