
Training physicians to be more empathetic, particularly toward people of other races, may be an effective tool at closing the racial gap in pain relief. An empathetic physician can have a real impact on their patients’ well-being.
Full Answer
Does racial bias in pain perception affect treatment recommendations?
In contrast, endorsing more false beliefs was associated with perceptions that blacks feel less pain and a “commensurate” insufficient treatment recommendation for black patients. It thus seems that racial bias in pain perception has pernicious consequences for accuracy in treatment recommendations for black patients and not for white patients.
Why don’t doctors treat black patients’ pain?
The second possibility is that physicians do not recognize black patients’ pain in the first place, and thus cannot treat it. In fact, recent work suggests that racial bias in pain treatment may stem, in part, from racial bias in perceptions of others’ pain.
What are some examples of racial disparities in pain management?
For example, a study examining pain management among patients with metastatic or recurrent cancer found that only 35% of racial minority patients received the appropriate prescriptions—as established by the World Health Organization guidelines—compared with 50% of nonminority patients (4).
Can physician training help close The racial gap in pain relief?
Training physicians to be more empathetic, particularly toward people of other races, may be an effective tool at closing the racial gap in pain relief. An empathetic physician can have a real impact on their patients’ well-being.
How do you get rid of racial bias in healthcare?
Actions that health care providers can take to combat implicit bias, include:Having a basic understanding of the cultures from which your patients come.Avoiding stereotyping your patients; individuate them.Understanding and respecting the magnitude of unconscious bias.More items...
How do African Americans respond to pain?
African Americans were found to have lower pain thresholds than whites for cold, heat, pressure, and ischemia [4]. Most studies showed no racial differences in pain intensity ratings, although African Americans described comparable pain intensity as a more unpleasant sensation than did whites [4].
What race has higher pain tolerance?
It was found that African Americans had a significantly lower pain tolerance (M = 63.2) than both Caucasians (M= 148.92, p=. 003) and Asians (M= 132.57, p= . 03). Asians had higher pain intensity (M=8.99) than Hispanics (M= 7.74, p=.
Why is race important in medicine?
Race continues to permeate medical teaching and clinical decision making and treatment in multiple ways, including: (1) through providers' attitudes and implicit biases, (2) disease stereotyping and nomenclature, and (3) clinical algorithms and treatment guidelines.
What is the problem with race based medicine?
However, Roberts traces race-based medicine to false assumptions about innate biological differences and to ugly justifications for slavery and medical exploitation. Today, race-based medicine diverts attention and resources from the social determinants that cause appalling racial gaps in health.
How culture affects pain perception?
Evidence supports the idea that culture can influence many pain-related factors, including but not limited to, how an individual communicates pain, an individual's emotional responses to someone else's pain (empathy), pain intensity and tolerance, beliefs about and coping with pain, and pain catastrophizing.
Do different cultures have different pain tolerances?
Ethnic differences in experimental pain have been shown in other countries as well. For example, in a Canadian study, Chinese participants reported greater pain catastrophizing, displayed lower pain tolerance and reported higher affective responses than European Canadians to a cold pressor task [30].
What determines your pain tolerance?
Pain tolerance is influenced by people's emotions, bodies, and lifestyles. Here are several factors that Grabois says can affect pain tolerance: Depression and anxiety can make a person more sensitive to pain. Athletes can withstand more pain than people who don't exercise.
Do Asians have a lower pain tolerance?
Perceived stress, anxiety, perfectionism, parental criticism, parental expectations and depressive symptoms were also measured. The results indicated that for the cold pain test, Asians demonstrated significantly lower pain threshold and tolerance levels than Whites.
What is race correction in medicine?
Race correction is the use of a patient's race in a scientific equation that can influence how they are treated. In other words, some diagnostic algorithms and risk predictor tools adjust or "correct" their results based on a person's race.
What is race based healthcare?
For centuries, race-based medicine in the United States has aimed to identify biological differences between racial groups that could then be used to tailor health care to members of those groups.
When is race used in medicine?
The role of patient race in medical decision-making is heavily debated. While some evidence suggests that patient race can be used by physicians to predict disease risk and determine drug therapy, other studies document bias and stereotyping by physicians based on patient race.
Is high pain tolerance genetic?
Sometimes physicians, friends, and family members quickly dismiss pain as being all in a patient's head, but this research shows that pain tolerance is controlled to some extent by genes.
How do you know if you have a high pain tolerance?
Your pain threshold is determined by the amount of time between the start of the test and your first report of pain. Once the pain becomes unbearable, you can remove your hand. The time between the test start and when your remove your hand is considered your pain tolerance.
What is the human pain tolerance?
Pain tolerance, is the maximum amount, or level, of pain a person can tolerate or bear. For example, when listening to a sound, the level of loudness, or pressure, at which the sound becomes painful is described as the pain threshold for that person at that time.
Which of the following is the most reliable indicator for chronic pain?
Abstract. Self-report of pain is the single most reliable indicator of pain intensity.
What is racism in medicine?
“Racism” is generally used to refer to active, willful acts of discrimination and harm. It would be a mistake to conclude that racial disparities in medicine are purposefully propagated.
How much was the disparity between the experimental group’s pain treatment of African Americans and whites?
The disparity between the experimental group’s pain treatment of African Americans and whites was approximately 50 percent lower than that of nurses in the control group. Racial bias can clearly be reduced in medical decision making as well.
Is racial health disparities a reality?
Racial health care disparities are a reality, and it is this author’s opinion that the racial biases of health care professionals are driving numerous health care disparities. Some of the research presented in the previous sections supports this claim; however, I also acknowledge that more definitive evidence is needed to support it. Nonetheless, the infrastructure does not currently exist to examine this question, let alone develop interventions capable of eliminating the racial biases that we know exist. In the paragraphs that follow, I argue that medical education is in a prime position to develop this infrastructure, which will require collaboration, data, and time.
Is racial bias a function of institutional bias?
Clearly, racial bias in health care is not simply a function of uncontrollable, institutional biases—individuals’ decision-making processes are also at play.
Is racial discrimination real?
Racial disparities in health care and pain treatment are real. Patients are suffering, and research indicates that racial bias permeates American society. Prejudice of the nonconscious sort is the rule, not the exception. Although people have a tendency to avoid confronting their own biases and do not know how to ameliorate them, evidence from the social sciences suggests that racial biases can be reduced.
Why do people fail to get along in health care?
Racism and discrimination in health care: Providers and patients. “People fail to get along because they fear each other; they fear each other because they don’t know each other ; they don’t know each other because they have not communicated with each other.”. A patient of mine recently shared a story with me about her visit to an area emergency ...
Is the CDC relaxed?
The CDC has relaxed some prevention measures, particularly for people who are fully vaccinated, and especially outdoors. Meanwhile, scientists continue to explore treatments and to keep an eye on viral variants. Doctors take an oath to treat all patients equally, and yet not all patients are treated equally well.
What is the Medical Definition of Pain?
The American Academy of Pain Medicine classifies pain in two categories, acute and chronic. When a patient is experiencing acute pain, the source is related with an injury. The pain is considered “short-lived and self-limiting” because, ideally, the need for pain management is temporary and will alleviate on it’s own as the injury heals.
Why are Some Not Treated for Their Pain?
Evidence indicating that physicians and nurses do not treat pain adequately began to appear in medical literature nearly 30 years ago. It exists alongside current news chronicling the opioid crisis sweeping the nation.
The Relationship Between Racism & Pain Treatment
Drilling down through the healthcare system from birthing suite to hospice care, reveals that at every point along the journey, Black patients are less likely than white patients to receive any pain medication at all. And when pain medication is administered, lower doses are prescribed, regardless of pain score.
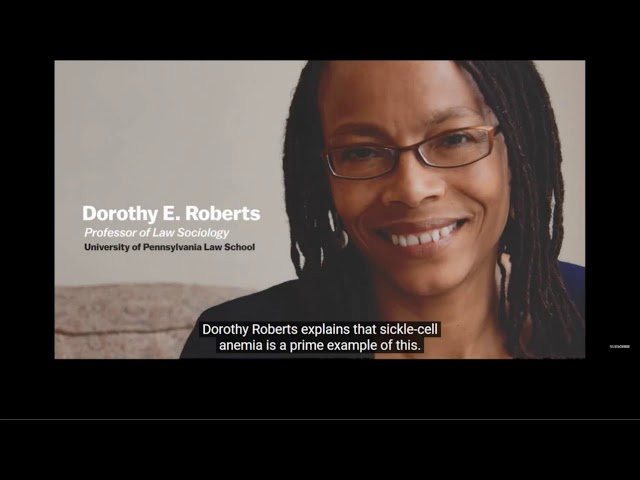
Sickle Cell Anemia and Pain Treatment?
The outreaching effects of racism on the healthcare system means that when dealing with diseases that predominantly affect the Black community, the treatments, research, and medications are inefficient at the core.
Chronic Pain Exacerbated by Lack of Access to Care
SCA patients are frequently seen in emergency rooms or require admission for treatment of pain, infection, or other complications. Readmissions to hospitals are receiving enormous attention from Medicare and other payers, such as health insurance companies, with hospitals being penalized for readmissions for specific diagnoses.
Can a Physician be Held Liable for Failing to Treat Pain?
There is an established standard of care when it comes to pain management and physicians who fail to treat pain according to those standards are committing medical malpractice, and gross negligence. And, even if professional medical or hospital boards don’t hold physician licensees to that standard, juries will.
Is Access to Pain Medication a Human Right?
The ethical responsibility of clinicians to manage pain is well understood and stands as a basic element of ethical medical codes. Many organizations around the world recognize this right.
What is the greatest racial disparity in pain treatment?
In fact, in the meta-analysis, the greatest racial disparity in pain treatment was for conditions like backache, migraine, and abdominal pain. Racial and ethnic disparities in pain treatment are not intentional. …. Instead, inequities are the product of complex influences, including implicit biases that providers don’t even know they have.
Do white people have unconscious bias?
Although providers might like to believe that they do not har bor unconscious biases, research shows that they are just as likely as others to do so.
Is pain assessment subjective?
In addition, assessment of pain is inherently subjective.
Why do doctors treat black people differently?
Experts say doctors diagnose and treat Black Americans differently for pain management. They say this is partly because of the mistaken belief of some medical professionals that Black people feel pain differently than white people. Experts are encouraging the medical profession to make changes to avoid this and other systemic discriminatory ...
Why was the goal of the study Black bodies inferior to white bodies?
The goal was to show that Black bodies were inferior to white bodies, that they were less sensitive to pain, which justified inflicting pain,” said Janice A. Sabin, PhD, MSW, a research associate professor at the University of Washington who studies the role of implicit bias in racial disparities in healthcare.
Is racism a public health threat?
The American Medical Association has set out a series of goals and policies to recognize racism as an urgent public health threat and to mitigate its effects. “There are ways to test your own bias. We often use the implicit association test in research and as an educational tool,” Sabin told Healthline.
Is there racial bias in healthcare?
Systemic bias in healthcare. Experts say it’s not a surprise that there’s racial bias in the medical field, as healthcare mirrors the larger society. “The root is white supremacy ideology, a false belief in a hierarchy that puts white people at the top, and it results in a dehumanization of people of color,” Jones said.

What Was Their Proposed Solution?
- The authors do, at least, propose something to change the status quo. However, there are problems with their proposed solution. Here is what they propose: 1. Provide more opportunities for BIPOC individuals to enter health and medical professions, in particular Black, Indigenous and Latinx individuals focusing on pain management practices. 2. Add a...
What’s Wrong with This Proposal
- All a person has to do to see what is wrong with bringing more BIPOC practitioners into pain management is reflected in the list of practitioners attacked. The majority of those attacked are BIPOC. So asking more to join the specialty would just insure that they would become targets of the DOJ. Then it doesn’t matter how much incentivization there is, the government would take it …
So What Is needed?
- We need for the systemic racism to be addressed by recognizing that attacks on drugs was a government racist ploy to start with, and needs to end NOW!! POC need to join us in this fight. In fact, since chronic pain patients can’t seem to get the right message in their heads, POC need to steal the ball and run with it, straight to the goal line. That can be done quickly and easily with w…
Health Care Disparities Persist
Default Strategies For Addressing Bias May Be Ineffective
Racial Bias Is Common
Are Health Care Professionals Racist?
Racial Bias Can Be Reduced and Eliminated
- What actions can be taken to reduce the effects of racial bias in health care professions? Social psychology research provides evidence that reducing racially biased behaviors, emotions, and thoughts is possible. For example, one of the most effective methods for reducing prejudice is equal-status contact, which involves members from different raci...
Conclusion
Why Are Certain Groups of Patients Getting Different Care?
Why Are Doctors Sometimes The Targets of Bias and Racism?
and Can We Fix this?
- Articles addressing racism in medicine suggest many of the same things. To fight racism and discrimination, we all need to recognize, name, and understand these attitudes and actions. We need to be open to identifying and controlling our own implicit biases. We need to be able to manage overt bigotry safely, learn from it, and educate others. These...
Sources