Full Answer
How to prevent infection after dental work?
- It’s very easy to make a salt water rinse. All you have to do is add a half teaspoon of salt to one cup of warm water.
- After oral surgery like wisdom tooth extraction, start to rinse your mouth with salt water the next day. ...
- Some dentists may ask you to irrigate after a tooth extraction, too. ...
Who needs endocarditis prophylaxis?
- Prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts.
- Prosthetic material used for heart valve repair, such as annuloplasty rings, chords or clips.
- Previous IE.
What can cause endocarditis?
The study titled, "Infective Endocarditis Caused by Staphylococcus aureus After Transcatheter Aortic Valve Replacement," was published in the Canadian Journal of Cardiology. Medha Baranwal joined Medical Dialogues as an Editor in 2018 for Speciality Medical Dialogues.
What is the most common cause of infective endocarditis?
What is the most common cause of endocarditis? Bacterial. Staphylococcus aureus followed by Streptococci of the viridans group and coagulase negative Staphylococci are the three most common organisms responsible for infective endocarditis. Other Streptococci and Enterococci are also a frequent cause of infective endocarditis.

How long does it take for endocarditis to develop after a dental procedure?
Studies suggest that the incubation period of IE is usually 7 to 14 days for viridans group streptococci or enterococci, with 78% of cases occurring within 7 days of bacteremia and 85% within 14 days.
How common is endocarditis after dental work?
As a result of dental treatment a small amount of patients contract bacterial endocarditis (EB). Developing bacterial endocarditis (EB) in valve diseases patients is statistically 1 every 3000 cases. Intravascular access might be often infected; however, there is no evidence of a dental origin for these infections.
Can you get endocarditis from going to the dentist?
7 Invasive dental procedures that disrupt gingival integrity allow oral bacteria to access the circulation, which can lead to infective endocarditis in at-risk patients.
What is the most common cause of infective endocarditis after dental procedure?
The most common causative agent was VGS followed by Staphylococcus aureus. Forty percent of patients had a medical/surgical or dental procedure performed 2 to 6 months prior to the diagnosis of IE. The majority of these patients were given antibiotic prophylaxis perioperatively for their respective procedures.
What is the incubation period for endocarditis?
Studies suggest that the incubation period of IE is usually 7 to 14 days for viridans group streptococci or enterococci, with 78% of cases occurring within 7 days of bacteremia and 85% within 14 days.
What are the warning signs of endocarditis?
Common signs and symptoms of endocarditis include:Aching joints and muscles.Chest pain when you breathe.Fatigue.Flu-like symptoms, such as fever and chills.Night sweats.Shortness of breath.Swelling in your feet, legs or abdomen.More items...•
Can tooth cleaning cause endocarditis?
According to the American Heart Association, the biggest causes of infective endocarditis include poor oral hygiene, minor gum injury caused by tooth brushing, and dental procedures.
Can teeth cleaning cause endocarditis?
We also did not find any association between invasive dental treatments and infective endocarditis among patients with a high risk for infective endocarditis, such as those with a history of rheumatic heart disease or valve replacement.
Can endocarditis go away by itself?
Endocarditis is treated with a course of antibiotics given via a drip. You'll need to be admitted to hospital for this. Some people also need surgery to repair or replace a damaged heart valve or drain away any abscesses that develop. Endocarditis is a serious illness, especially if complications develop.
What are the chances of surviving endocarditis?
Conclusions: Long term survival following infective endocarditis is 50% after 10 years and is predicted by early surgical treatment, age < 55 years, lack of congestive heart failure, and the initial presence of more symptoms of endocarditis.
How common is bacterial endocarditis?
Infective endocarditis has an incidence rate of 3-10 cases in every 100,000 people.
What oral bacteria causes endocarditis?
Various micro-organisms have been implicated as causative agents for bacterial endocarditis, including lactobacilli and in particular the viridans streptococci which are more commonly associated with dental caries. Of these, the most frequently isolated one has the descriptive name Streptococcus sanguis.
What is the infection of the heart?
Infective endocarditis is a serious infection occurring on the endothelial surfaces of the heart , especially at the valves. Oral commensal bacteria are the important etiologic agents in this disease.
Can dental procedures cause bacteremia?
Common dental procedures, even non-surgical dental procedures, can often cause bacteremia of oral co …. Infective endocarditis is a serious infection occurring on the endothelial surfaces of the heart, especially at the valves. Oral commensal bacteria are the important etiologic agents in this disease.
Is dental invasive treatment a risk factor?
Invasive dental treatments (IDTs) have been considered a potential risk factor of IE; however, the association between IDTs and IE remains controversial. Dental treatments were considered IDTs when the treatments might cause bleeding and introduce oral bacteria into the bloodstream, such as dental cleaning, scaling and root planing, extraction, ...
Can dental treatments cause bacteremia?
Invasive dental treatments (IDTs) can yield temporary bacteremia and have therefore been considered a potential risk factor of infective endocarditis (IE). It is hypothesized that, through the trauma caused by IDTs, bacteria gain entry to the bloodstream and may attach to abnormal heart valves or damaged heart tissue, giving rise to IE.
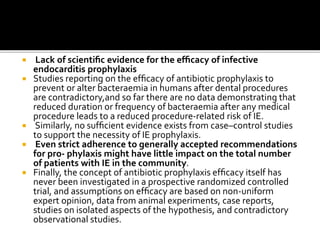
Is antibiotic prophylaxis effective for endocarditis?
Antibiotic prophylaxis has been recommended for the prevention of infective endocarditis in patients with a high risk for infective endocarditis. However, the effectiveness of antibiotic prophylaxis has remained a controversial issue for decades. Our large population-based study did not observe any clinically significant association between ...
When did the endocarditis guidelines change?
If your risk is high, you can take steps to lower it. How Have Endocarditis Prevention Guidelines Changed? In 2007, the American Heart Association Endocarditis Committee -- together with other experts -- issued guidelines to help prevent endocarditis. These replaced guidelines issued in 1997.
How long before dental treatment should you take antibiotics?
To prevent endocarditis, patients with certain heart conditions receive a single dose of an antibiotic. You receive it about one hour prior to certain dental treatments. The American Heart Association and American Dental Association now suggest that you receive antibiotics prior to dental treatment onlyif you have:
What happens when your gums bleed?
When gums bleed, the bacteria can enter the bloodstream and can infect other parts of the body. In the case of endocarditis, this affects the inner lining of the heart and the surfaces of its valves. The bacteria stick to these surfaces and create growths or pockets of bacteria. Because this is so rare, the new guidelines suggest antibiotics prior ...
What is endocarditis in the heart?
Endocarditis is a rare, life-threatening inflammation of the lining of the heart muscle and its valves. It is caused by a bacterial infection. Although it can occur in anyone, it is much more common in people with certain heart conditions and in those who've had it before. If your risk is high, you can take steps to lower it.
Can antibiotics cause endocarditis?
In patients with heart conditions associated with the highest risk of serious complications from endocarditis, it says that antibiotic treatment before dental procedures involving manipulation of the gums seems reasonable. In very rare cases, bacteria in the mouth may trigger endocarditis in people at higher risk.
Can dental procedures cause endocarditis?
Some dental procedures can trigger endocarditis, an inflammation in the heart. WebMD explains who's at risk and how it can be prevented. Skip to main content . Check Your Symptoms . Find A Doctor .
Can you take antibiotics before dental surgery?
Because this is so rare, the new guidelines suggest antibiotics prior to dental procedures only for patients who are at highest risk for serious complications from endocarditis. In fact, in most cases, the risk of problems from antibiotics exceeds the benefits from preventive antibiotics.
