What are the dangers of monoclonal antibodies?
Feb 06, 2022 · Monoclonal antibody therapy for COVID-19 is well tolerated with minimal risks. Injection site reactions and infusion-related reactions are the most commonly reported adverse events. Infusion-related reactions are potential adverse reactions when administering monoclonal antibodies and are common with drugs such as rituximab.
How effective is the monoclonal treatment?
Monoclonal antibodies (mAbs) are now established as targeted therapies for malignancies, transplant rejection, autoimmune and infectious diseases, as well as a range of new indications. However, administration of mAbs carries the risk of immune reactions such as acute anaphylaxis, serum sickness and the generation of antibodies.
How long after monoclonal antibodies are you contagious?
Jan 06, 2022 · The FDA has authorized the emergency use of monoclonal antibody therapy for the treatment of COVID-19 under an Emergency Use Authorization (EUA) for people 12 years of age or older. “In multiple randomized controlled trials, high-risk outpatients with confirmed COVID-19 were 2-7% less likely to be hospitalized with severe COVID-19,” Spivak says.
When to give monoclonal antibody?
CAN MONOCLONAL ANTIBODY TREATMENT MAKE ME SICK? Antibody treatments do not contain any live virus, so there is no risk you will get COVID-19 from mAb treatment. However, the antibody treatment may have side effects: Allergic reactions can happen during and after an antibody infusion.

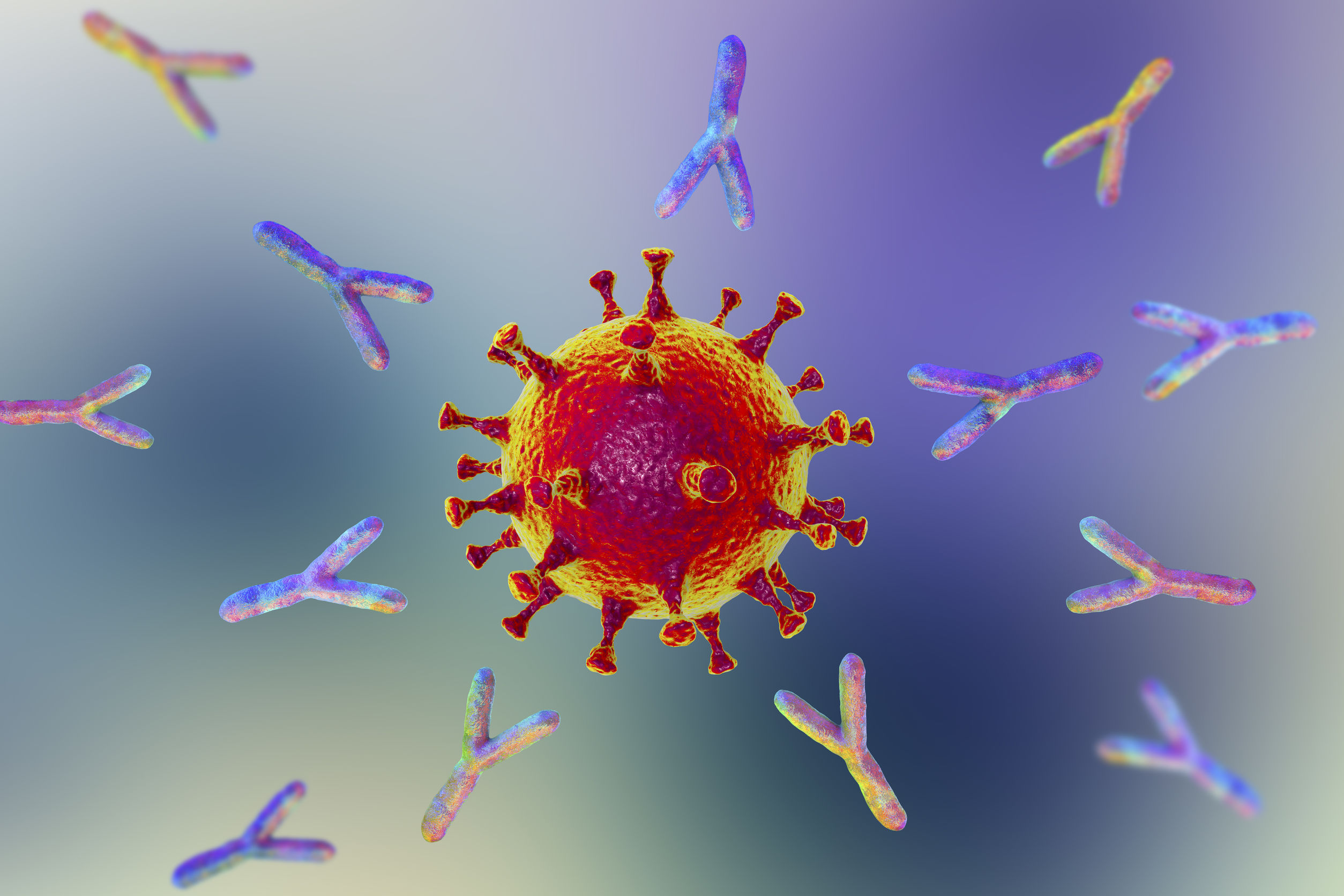
How do monoclonal antibodies work against COVID-19?
Monoclonal antibodies for COVID-19 may block the virus that causes COVID-19 from attaching to human cells, making it more difficult for the virus to reproduce and cause harm. Monoclonal antibodies may also neutralize a virus.Mar 31, 2022
Can I get the COVID-19 vaccine if I was treated with monoclonal antibodies or convalescent plasma?
If you were treated for COVID-19 symptoms with monoclonal antibodies or convalescent plasma, you should wait 90 days before getting a COVID-19 vaccine.
What does monoclonal antibody treatment mean for COVID-19?
Monoclonal antibodies are manmade versions of the antibodies that our bodies naturally make to fight invaders, such as the SARS-CoV-2 virus.Apr 1, 2022
What is the difference between monoclonal antibodies and the COVID-19 vaccine?
COVID-19 vaccines help stimulate and prepare a person's immune system to respond if they are exposed to the virus. However, monoclonal antibodies boost the immune system only after a person is already sick, speeding up their immune response to prevent COVID-19 from getting worse.Nov 8, 2021
Should you still get the COVID-19 vaccine if you were treated with monoclonal antibodies?
If you were treated for COVID-19 with monoclonal antibodies or convalescent plasma, there is no need to delay getting a COVID-19 vaccine.Feb 17, 2022
Do I need the COVID-19 vaccine if I still have antibodies?
Yes, the COVID-19 vaccines are recommended, even if you had COVID-19.Nov 23, 2021
How long do COVID-19 antibodies last?
At this time, it is unknown for how long antibodies persist following infection and if the presence of antibodies confers protective immunity.Jan 31, 2022
How many types of monoclonal antibody COVID-19 treatments are there in the US?
In the United States, there are three anti-SARS-CoV-2 monoclonal antibody treatments with FDA Emergency Use Authorization (EUA) for the treatment of COVID-19: bamlanivimab plus etesevimab, casirivimab plus imdevimab,, and sotrovimab.
How long could it take to develop antibodies against COVID-19?
It takes 5-10 days after you get infected to develop antibodies against the SARS-CoV-2 virus. Antibody tests could give people a false sense of security. They might go back to work and start to travel again when they could still catch or spread the virus.Jan 21, 2022
Can I get COVID-19 again after having the vaccine?
Getting COVID-19 after you've been vaccinated or recovered is still possible. But having some immunity -- whether from infection or vaccination -- really drops the odds of this happening to you.Nov 9, 2021
Who should not take the Pfizer-BioNTech COVID-19 vaccine?
If you have had a severe allergic reaction to any ingredient in the Pfizer-BioNTech COVID-19 vaccine (such as polyethylene glycol), you should not get this vaccine. If you had a severe allergic reaction after getting a dose of the Pfizer-BioNTech COVID-19 vaccine, you should not get another dose of an mRNA vaccine.
What is the main ingredient in an mRNA coronavirus vaccine?
mRNA – Also known as messenger ribonucleic acid, mRNA is the only active ingredient in the vaccine. The mRNA molecules contain the genetic material that provide instructions for our body on how to make a viral protein that triggers an immune response within our bodies.Jan 11, 2021
What is a monoclonal antibody?
Monoclonal antibodies (mAbs) are now established as targeted therapies for malignancies, transplant rejection, autoimmune and infectious diseases, as well as a range of new indications . However, administration of mAbs carries the risk of immune reactions such as acute anaphylaxis, serum sickness and ….
What are the adverse effects of mAbs?
In addition, there are numerous adverse effects of mAbs that are related to their specific targets, including infections and cancer, autoimmune disease, and organ-specific adverse events such as cardiotoxicity.
What is mAb therapy?
Monoclonal antibodies (mAbs) are now established as targeted therapies for malignancies, transplant rejection, autoimmune and infectious diseases, as well as a range of new indications. However, administration of mAbs carries the risk of immune reactions such as acute anaphylaxis, serum sickness and the generation of antibodies.
When did TGN1412 occur?
In March 2006, a life-threatening cytokine release syndrome occurred during a first-in-human study with TGN1412 (a CD28-specific superagonist mAb), resulting in a range of recommendations to improve the safety of initial human clinical studies with mAbs.
What are monoclonal antibodies?
Our bodies naturally make antibodies to fight infections. However, if you haven’t received the COVID-19 vaccine or had a previous COVID-19 infection, your body will not have antibodies designed to recognize a new virus like SARS-CoV-2.
How does monoclonal antibody therapy help?
Monoclonal antibody therapy is a way of treating COVID-19 for people who have tested positive, have had mild symptoms for seven days or less, and are at high risk for developing more serious symptoms.
Who is eligible for monoclonal antibody therapy?
Given that COVID-19 vaccination provides strong protection against severe disease and need for hospitalization, monoclonal antibody therapy is an option for certain high-risk patients with COVID-19.
WHAT IS A MONOCLONAL ANTIBODY?
Your body naturally makes antibodies to fight infection. However, your body may not have antibodies designed to recognize a novel (or new) virus like SARS-CoV-2, the virus that causes COVID-19.
How Can I Get Monoclonal Antibodies?
To receive a mAb you should be referred for treatment by your healthcare professional and directed to available infusion locations. If you do not have a healthcare provider, call the Combat COVID Monoclonal Antibodies Call Center at 1-877-332-6585 to find out who to talk with about your symptoms and treatment.
WHAT IF I DO NOT QUALIFY FOR MONOCLONAL ANTIBODY TREATMENT?
Your healthcare professional may decide you do not qualify for mAb treatment. There could be several reasons for this. You may not meet all eligibility criteria or you may have an underlying health condition that disqualifies you for mAb treatment.
WHAT CAN I EXPECT FROM TREATMENT (INFUSION)?
The mAb treatment is usually offered at an infusion center because the treatment is given through an intravenous (IV) infusion or shots. Depending on the mAb treatment you receive, the whole process takes about 1-3 hours, depending on the treatment..
CAN MONOCLONAL ANTIBODY TREATMENT MAKE ME SICK?
Antibody treatments do not contain any live SARS-CoV-2, so there is no risk you will get COVID-19 from mAb treatment. However, the antibody treatment may have side effects:
What antibody is used to block the virus?
Monoclonal antibodies against COVID-19 attach to the virus to block it from entering human cells. The monoclonal antibody protein also “marks” the virus to be broken down by the immune system and cleared from the body.
What is the function of antibodies?
Antibodies are proteins that exist in our bodies as part of our immune system to recognize and defend against harmful viruses and bacteria. Monoclonal antibodies are made in a laboratory and designed to target a specific virus or bacteria.
Can monoclonal antibodies cause nausea?
Most people tolerate monoclonal antibody infusions very well. Some people may experience infusion-related side effects, such as nausea and dizziness, that are short-lived and go away on their own. As with any medication, there is the potential for mild or more severe allergic reactions, which are uncommon.
Why is monoclonal antibody therapy important?
"Monoclonal antibody therapy is really important for the transplant population because they are less likely to develop their own immunity.
What is the purpose of monoclonal antibodies?
Monoclonal antibodies help prevent the virusthat causes COVID-19 from attaching to human cells, which helps block the spread of infection. In fall 2020, the Food and Drug Administration authorized the emergency use of bamlanivimab and casirivimab-imdevimab to treat mild to moderate COVID-19 in patients with a high risk of becoming seriously ill.
Is Mayo Clinic a nonprofit?
Mayo Clinic is a nonprofit organization committed to innovation in clinical practice, education and research, and providing compassion, expertise and answers to everyone who needs healing. Visit the Mayo Clinic News Network for additional Mayo Clinic news.
Is it safe to have monoclonal antibodies in 2021?
June 10, 2021. ROCHESTER, Minn. — Treating transplant patients with mild to moderate cases of COVID-19 with monoclonal antibodies is safe and helps prevent serious illness, according to a Mayo Clinic study recently published in Open Forum Infectious Diseases.
What is a monoclonal antibody?
Monoclonal antibodies are copies of human antibodies, created in a lab, that bolster your immune system to fight off an illness. With COVID-19, monoclonal antibodies bind to COVID-19’s spike protein to neutralize the virus and fight off the infection.
When was monoclonal antibody first discovered?
It was discovered in the mid-1970s and brought to market in the mid-1990s. “Now, there are more than 60 FDA-approved monoclonal antibody treatments for various diseases, including autoimmune diseases, cancer, and other infections,” says Dr. Muma. “This type of treatment has been a huge breakthrough in healthcare.
What are the requirements for a syringe?
The Food and Drug Administration (FDA) outlined specific guidelines of who qualifies for the treatment: 1 All adults ages 65 and older. 2 Anyone who is pregnant. 3 Children ages 12 to 17 with a body mass index (BMI) equal to or higher than 85% of children who are the same age and gender. 4 Adults ages 18 and older with a BMI of 25 or greater. 5 Anyone ages 12 and older with: diabetes, chronic kidney disease, a disease that weakens the immune system or a weakened immune system due to medication, cardiovascular disease (including congenital heart disease) or hypertension, chronic lung diseases, moderate to severe asthma, sickle cell disease, neurodevelopmental disorders (for example, cerebral palsy), genetic or metabolic syndromes and severe congenital anomalies, or regular use of medical technology (such as a feeding tube or a device that assists with breathing).
Can you get monoclonal antibody therapy?
You cannot receive monoclonal antibody therapy if you have already progressed to severe illness—once you’re in the hospital or on oxygen, the treatment is not approved for use, so it’s incredibly important to talk to your doctor as soon as possible to see if you’d be a candidate. All adults ages 65 and older.
Who is Bruce Muma?
Bruce Muma, M.D., is an internal medicine physician with Henry Ford Health System. He is the CEO of Henry Ford Physician Network and is leading the expansion of the monoclonal antibody clinics at Henry Ford. Categories: FeelWell. Tags: Coronavirus.
Is monoclonal antibody effective?
“This treatment is 70% effective in reducing rates of hospitalization and death, yet not many people know about it,” says Bruce Muma, M.D ., CEO of Henry Ford Physician Network.