
Treatment of infection by Yersinia pestis should be started soon after the first symptoms appear, as this bacterium can cause death in less than 24 hours.
Full Answer
When should treatment for Yersinia pestis be started?
Treatment of infection by Yersinia pestis should be started soon after the first symptoms appear, as this bacterium can cause death in less than 24 hours.
What are the treatment options for Yersinia infections?
If Yersinia infection is suspected, the clinical laboratory should be notified and instructed to culture on cefsulodin-irgasan-novobiocin (CIN) or other specific for growing it. Most infections are self-limited. Antibiotics should be given for severe cases.
Do symptoms of yersiniosis go away?
Most symptoms go away completely. However, some people may experience the following: Joint pain, called reactive arthritis, most commonly in the knees, ankles, or wrists. These joint pains usually develop about 1 month after yersiniosis illness begins and generally goes away after 1 to 6 months.
How is the diagnosis of Yersinia infections made?
Diagnosis is made by isolating the organism from stool, blood, bile, wound, throat swab, mesenteric lymph node, cerebrospinal fluid, or peritoneal fluid. If Yersinia infection is suspected, the clinical laboratory should be notified and instructed to culture on cefsulodin-irgasan-novobiocin (CIN) or other specific for growing it.
See more
Does Yersinia need to be treated?
Yersiniosis usually goes away on its own without antibiotic treatment. However, antibiotics may be used to treat more severe or complicated infections.
How long can you have Yersinia?
How long does it last? The symptoms usually last for 1 to 3 weeks. People with mild symptoms usually recover on their own without treatment.
What is the typical incubation time period for Yersinia?
Incubation period is typically 4–6 days (range, 1–14 days). Symptoms include fever, abdominal pain (may mimic appendicitis), and diarrhea (may be bloody and can persist for several weeks). Necrotizing enterocolitis has been described in infants.
How do I know if I have Yersinia?
Common symptoms in children are fever, abdominal pain, and diarrhea, which is often bloody. Symptoms typically develop 4 to 7 days after exposure and may last 1 to 3 weeks or longer. In older children and adults, right-sided abdominal pain and fever may be the predominant symptoms and may be confused with appendicitis.
Can Yersinia cause sepsis?
Yersinia enterocolitica is a gram-negative bacillus shaped bacterium that causes a zoonotic disease called yersiniosis. The infection is manifested as acute diarrhea, mesenteric adenitis, terminal ileitis, and pseudoappendicitis. In rare cases, it can even cause sepsis.
What is the treatment of Yersinia?
What is the best treatment? Fluoroquinolones are the drugs of choice for Y. enterocolitica infections, based on clinical observations and in vitro antimicrobial resistance studies. Third generation cephalosporins, trimethoprim-sulfamethoxazole and aminoglycosides also appear to be clinically effective.
Is Yersinia enterocolitica reportable?
In 38 states, Yersinia enterocolitica and/or Yersinia pseudotuberculosis infections are reportable, but no standard national definition exists for confirmed and probable cases.
How fast does plague spread?
A person usually becomes ill with bubonic plague 2 to 8 days after being infected. The incubation period of septicemic plague is poorly defined but likely occurs within days of exposure. A person exposed to Yersinia pestis through the air would usually become ill in just 1 to 3 days.
Can you survive bubonic plague without treatment?
Bubonic plague can be fatal if it's not treated. It can create infection throughout the body (septicemic plague) and / or infect your lungs (pneumonic plague.) Without treatment, septicemic plague and pneumonic plague are both fatal.
How common is yersiniosis?
Yersiniosis is an infection caused most often by eating raw or undercooked pork contaminated with Yersinia enterocolitica bacteria. CDC estimates Y. enterocolitica causes almost 117,000 illnesses, 640 hospitalizations, and 35 deaths in the United States every year.
Can Yersinia be chronic?
The correlations between acute and chronic symptoms indicate that yersiniosis is a chronic disease. Immunologically competent individuals may profit by fighting the infection in the right iliac fossa. The relationship between yersiniosis and inflammatory bowel diseases may still not be settled.
Can Yersinia come back?
Yersinia enterocolitica and Yersinia pseudotuberculosis are bacterial infections that are uncommon, but can cause problems when they occur. Y enterocolitica causes a condition called enterocolitis, which is an inflammation of the small intestine and colon that occurs, and often recurs, mostly in young children.
What Are Yersinia enterocolitica?
Y. enterolitica are the most common species causing human enteric (intestinal) yersiniosis.Pigs are the major animal reservoir for the few strains...
What Are The Symptoms of Yersiniosis?
The symptoms of yersiniosis depend on the age of the person infected. Infection occurs most often in young children. Common symptoms in children ar...
How Do People Get Yersiniosis?
Most people become infected by eating contaminated food, especially raw or undercooked pork, or through contact with a person who has prepared a po...
How Common Is Yersiniosis?
CDC estimates that infections with Yersinia enterocolitica cause almost 117,000 illnesses, 640 hospitalizations, and 35 deaths in the United States...
How Is Yersiniosis Diagnosed?
Yersiniosis usually is diagnosed by detecting the bacteria in the stool of an infected person. Many laboratories do not routinely test for Yersinia...
How Is Yersiniosis Treated?
Yersiniosis usually goes away on its own without antibiotic treatment. However, antibiotics may be used to treat more severe or complicated infecti...
Are There Long-Term Consequences of Yersiniosis?
Most symptoms go away completely. However, some people may experience the following: 1. Joint pain, called reactive arthritis, most commonly in the...
How Can I Help Protect Myself and My Family from Infection?
1. Avoid eating raw or undercooked pork. Learn more about the safe minimum cooking temperature for pork. 2. Consume only pasteurized milk and milk...
What Are Public Health Agencies Doing to Prevent and Control Yersiniosis?
Many agencies work together to prevent and control yersiniosis: 1. Public health departments investigate outbreaks of yersiniosis to stop them, and...
How long does it take for yersiniosis to go away?
These joint pains usually develop about 1 month after yersiniosis illness begins and generally go away after 1 to 6 months. A skin rash, called “erythema nodosum,” on the legs and torso.
How to diagnose yersiniosis?
Yersiniosis usually is diagnosed by detecting the bacteria in the stool of an infected person. Many laboratories do not routinely test for Yersinia, so it is important that the clinician notifies the laboratory when yersiniosis is suspected so that special tests can be done.
How many people die from yersiniosis every year?
How common is yersiniosis? CDC estimates that infections with Yersinia enterocolitica cause almost 117,000 illnesses, 640 hospitalizations, and 35 deaths in the United States every year. Children are infected more often than adults, and the infection is more common in the winter.
What is Y. enterocolitica?
What are Yersinia enterocolitica? Y. enterolitica are the most common species causing human enteric (intestinal) yersiniosis. Pigs are the major animal reservoir for the few strains of Y. enterocolitica that cause human illness, but rodents, rabbits, sheep, cattle, horses, dogs, and cats also can carry strains that cause human illness.
How long does it take for a child to get a fever?
Symptoms typically develop 4 to 7 days after exposure and may last 1 to 3 weeks or longer.
Does the CDC monitor yersinia enterocolitica?
CDC monitors Yersinia enterocolitica infections through the Foodborne Disease Active Surveillance Network ( FoodNet).
How can Yersinia be transmitted?
Yersinia bacteria can be transmitted by consuming or handling contaminated food, most commonly raw or undercooked por k products ; milk or milk products that were not pasteurized, inadequately pasteurized, or contaminated after pasteurization; or untreated water. They can also be transmitted by direct or indirect contact with animals.
What is the etiologic agent of Yersiniosis?
Etiologic agent. Yersiniosis is caused by a facultative anaerobic gram-negative coccobacilli in the genus Yersinia (most commonly Yersinia enterocolitica serogroups O:3; O:5,27; O:8; and O:9).
Does antimicrobial therapy affect postinfectious sequelae?
They are typically resistant to first-generation cephalosporins and most penicillins. Antimicrobial therapy has no effect on postinfectious sequelae. See the 2017 Infectious Diseases Society of America Clinical Practice Guidelines for the Diagnosis and Management of Infectious Diarrhea >. External.
Is Y. enterocolitica resistant to cephalosporins?
Most infections are self-limited. Antibiotics should be given for severe cases. Y. enterocolitica isolates are usually susceptible to trimethoprim-sulfamethoxazole, aminoglycosides, third-generation cephalosporins, fluoroquinolones, and tetracyclines; they are typically resistant to first-generation cephalosporins and most penicillins. They are typically resistant to first-generation cephalosporins and most penicillins. Antimicrobial therapy has no effect on postinfectious sequelae.
What doctor can treat erythema nodosum?
However, consultation with an infectious diseases specialist or gastroenterologist may be useful. Consultation with a rheumatologist may be helpful in cases of erythema nodosum or reactive arthritis. Next: Antibiotic Therapy. Antibiotic Therapy.
Can antibiotics cause bacteremia?
Avoid antimotility medications, which could lead to bacteremia. In cases of severe enterocolitis, antibiotics have shown some benefit in terms of shortening the duration of illness. Patient populations who should be considered for empiric antibiotic therapy include the following: Elderly patients.
Should blood banks be asked about gastroenteritis?
In blood banks, donors should be asked about any recent symptoms of gastroenteritis. Unwashed raw vegetables, uncooked meats (especially pork), and unpasteurized milk should be avoided [ 14, 15] Reservoirs should be eliminated. The contamination of food products should be minimized.
Etiologic Agent
- Yersiniosis is caused by a facultative anaerobic gram-negative coccobacilli in the genus Yersinia (most commonly Yersinia enterocoliticaserogroups O:3; O:5,27; O:8; and O:9).
Clinical Features
- Incubation period is typically 4–6 days (range, 1–14 days). Symptoms include fever, abdominal pain (may mimic appendicitis), and diarrhea (may be bloody and can persist for several weeks). Necrotizing enterocolitis has been described in infants. Reactive arthritis affecting the wrists, knees, and ankles can occur, usually 1 month after the initial diarrhea episode, resolving after 1–…
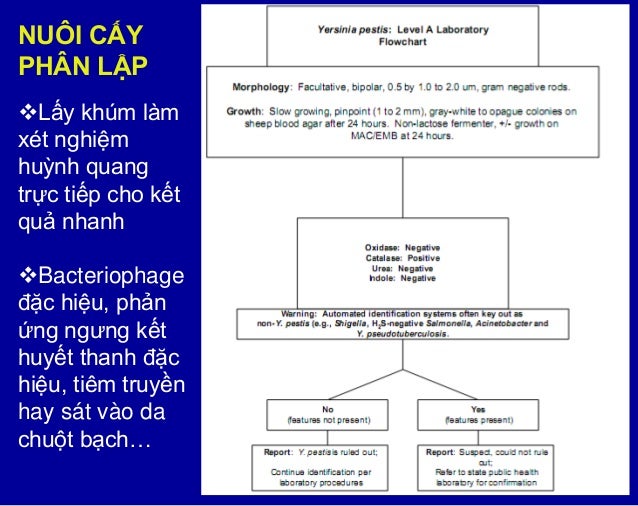
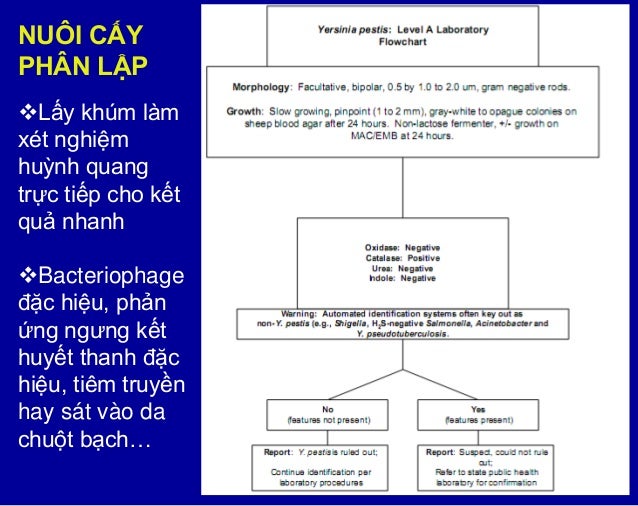
Diagnosis
- Diagnosis is made by isolating the organism from stool, blood, bile, wound, throat swab, mesenteric lymph node, cerebrospinal fluid, or peritoneal fluid. If Yersiniainfection is suspected, the clinical laboratory should be notified and instructed to culture on cefsulodin-irgasan-novobiocin (CIN) or other specific for growing it.
Treatment
- Most infections are self-limited. Antibiotics should be given for severe cases. Y. enterocoliticaisolates are usually susceptible to trimethoprim-sulfamethoxazole, aminoglycosides, third-generation cephalosporins, fluoroquinolones, and tetracyclines; they are typically resistant to first-generation cephalosporins and most penicillins. They are typically resi…
Surveillance
- The Centers for Disease Control and Prevention (CDC) monitors the frequency of Y. enterocolitica infections through the Foodborne Diseases Active Surveillance Network (FoodNet).
Incidence
- Y. enterocoliticais a relatively infrequent cause of diarrhea and abdominal pain. Infection is more common in winter. The incidence of yersiniosis in FoodNet sites in 2014 was 0.28 cases per 100,000 population. This met the U.S. Healthy People 2020 target for yersiniosisExternalfile_external of 0.30 or fewer cases per 100,000. Take a look at recent trends …
Transmission
- Yersiniabacteria can be transmitted by consuming or handling contaminated food, most commonly raw or undercooked pork products; milk or milk products that were not pasteurized, inadequately pasteurized, or contaminated after pasteurization; or untreated water. They can also be transmitted by direct or indirect contact with animals.
What Disease Is Caused byYersinia pestis
- The bacteriumYersiniapestilenceit causes bubonic plague, also popularly known as black plague and can be found in fleas, which are present mainly in infected rodents. This disease is serious and often fatal if it is not treated immediately, being the main responsible for the death of more than 30% of Europe's population in the 14th century.
Bacteria Life Cycle
- Fleas feed on blood, especially rodents. If the rodents are infected withYersinia pestis, when parasiting the animal, the flea also acquires this bacterium. When the rodent dies, the infected flea looks for other bodies to continue feeding on blood. Thus, it can infect other rodents and other animals, such as cats or humans through bites. Each flea can remain infected for months and th…
How The Transmission Happens
- The transmission of this bacterium to humans can occur in several ways, such as: 1. Infected flea bite; 2. Manipulation of blood, secretion or tissues of infected animals; 3. Bites and scratches from contaminated cats. The least common way of transmission is through vomiting, sneezing and coughing, in which the droplets are dispersed in the air and can spread this bacteria among …
How to Prevent
- Prevention for this infection can be done based on rodent and pest control and the use of repellents to prevent flea bites, since the plague-causing bacteria mainly infect rats, mice and squirrels, which are the main hosts of fleas . It is also important to wear protective equipment when handling blood, secretion and tissues from potentially infected animals. People who travel …