Buprenorphine
This medication is used to help relieve severe ongoing pain.
Naloxone
This medication is used for the emergency treatment of known or suspected opioid overdose.
Full Answer
How much does opioid treatment cost?
Feb 28, 2018 · Medicaid spending on prescription drug treatment for opioid use disorders more than doubled between 2011 and 2016, from $394 million to $930 million. Five states with particularly high overdose mortality rates — West Virginia, Massachusetts, Ohio, Rhode Island, and Kentucky — have also seen especially rapid growth in Medicaid spending for these drugs; all of …
How much does Medicaid spend on Suds?
A new report finds spending on Medicaid-covered prescriptions for the treatment of opioid use disorder and opioid overdose increased dramatically between 2011 and 2016, according to NPR. The largest increase occurred after 2014.
How much does it cost to treat substance abuse?
As an olive branch to opioid-ravaged states, lawmakers have talked about giving states $45 billion to spend on opioid treatment over 10 years, most likely in the form of grant money. The original...
What is the cost of methadone treatment?
Medicaid beneficiaries age 18–64 have a higher rate of opioid use disorder than privately insured individuals, comprising about 12 percent of all civilian, non-institutionalized adults in this age group but about one-quarter of those with an opioid use disorder.
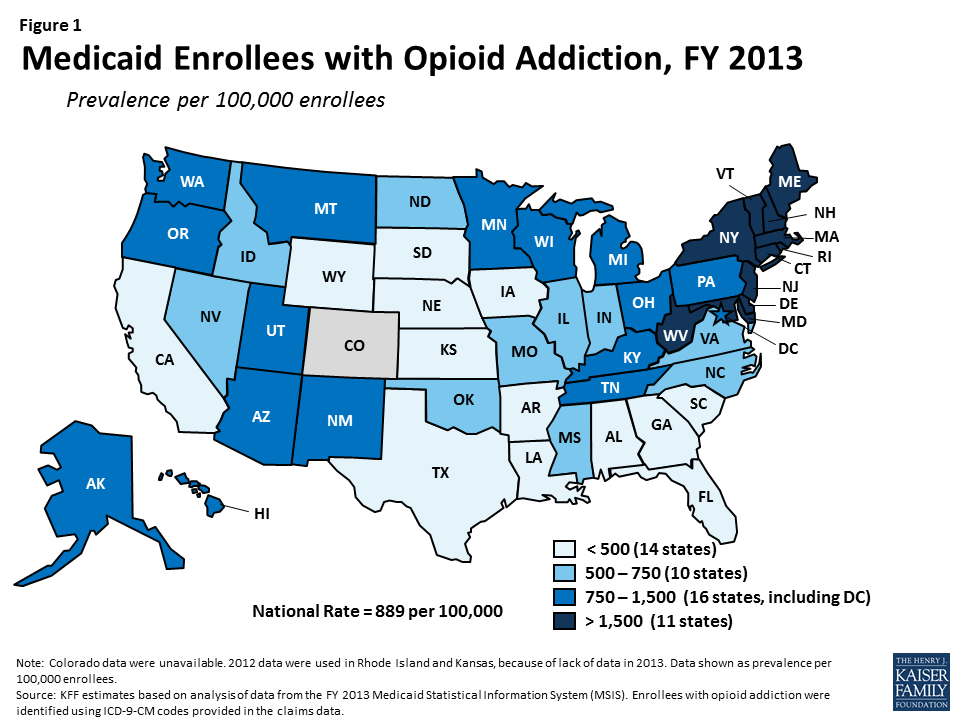
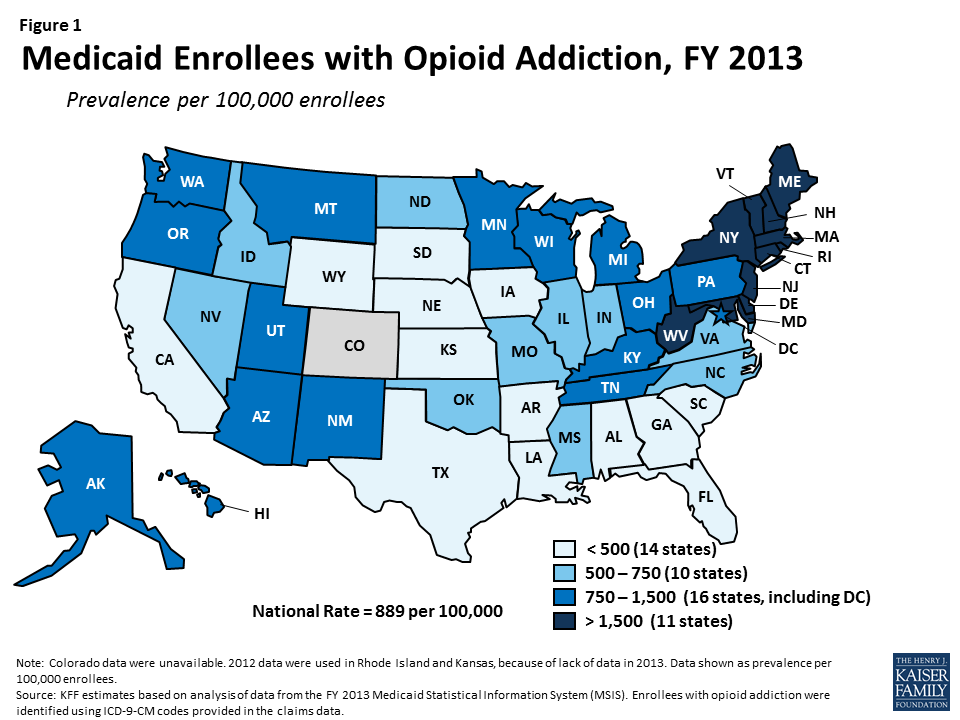
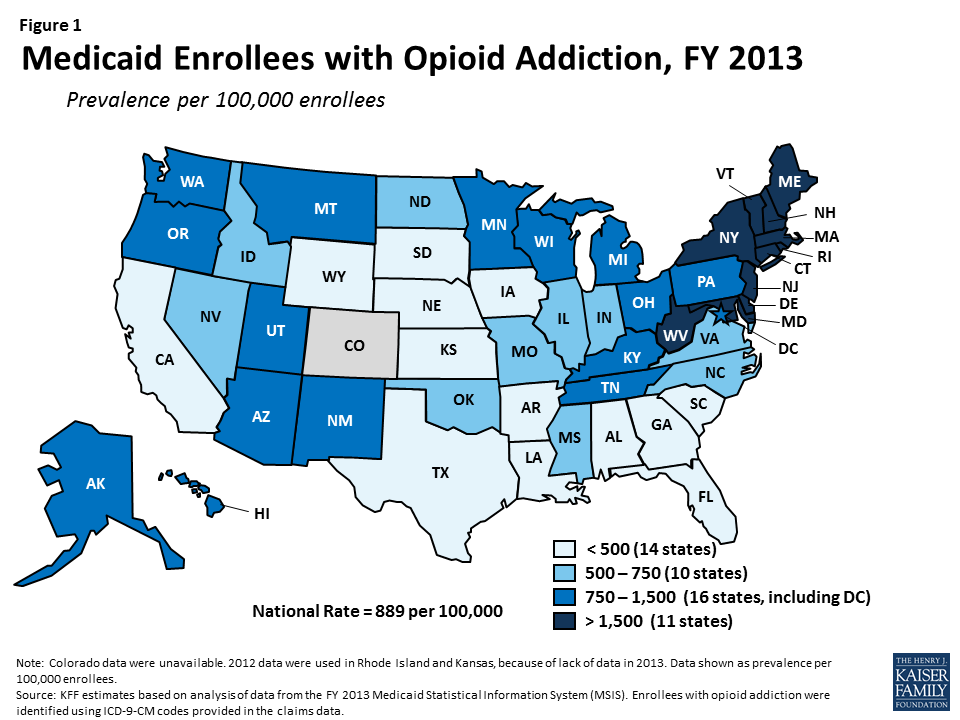
How many Medicaid enrollees have opioid addiction?
In FY 2013, there were 636,000 people enrolled in Medicaid with opioid addiction2, amounting to a prevalence of 889 per 100,000 (Table 1 and Figure 1). The number of Medicaid enrollees with opioid addiction ranged from a low in South Dakota of under 300 people to a high in New York of over 114,000 people.
How much does Medicaid spend on enrollees with opioid addiction?
Medicaid covers a broad range of services for people with opioid addiction, spending $9.4 billion on their care in FY 2013.
Looking Ahead
The opioid epidemic has led to substantial health complications, increased health care services utilization, and considerable societal costs. Medicaid has played a critical role in addressing the epidemic by facilitating access to addiction treatment services, including medication-assisted treatment.
How does Medicaid help with opioids?
State Medicaid programs cover substance use disorder treatment and supportive services to varying degrees. They are working to integrate care for physical health and treatment for substance use disorders across providers and with other social programs. They also are implementing programs to reduce opioid overprescribing in order to prevent opioid use disorder from developing in the first place. Many of these efforts are being undertaken in conjunction with other state and federal initiatives, such as the National Governors Association’s Compact to Fight Opioid Addiction and the Centers for Medicare & Medicaid Services (CMS) Opioid Misuse Strategy (CMS 2017a, NGA 2016).
Why are opioids not covered by medicaid?
Many Medicaid enrollees with an opioid use disorder are not receiving treatment, some due to barriers to care common in Medicaid and others due to circumstances unique to substance use disorders. Barriers common in Medicaid include lack of providers, diculty securing timely appointments, and lack of enabling services such as transportation and translation or interpretation services. As noted above, many states do not cover needed services. Barriers specific to substance use disorders include the stigma of having a substance use disorder (particularly if the substance is illicit or illegal), diculty understanding why treatment is needed, and physical and mental side effects of treatment that affect adherence and outcomes (Livingston et al. 2012, Mittal et al. 2012). Systems of care for substance use disorder treatment are frequently fragmented and poorly funded, which can create poor coordination among providers and gaps in the continuum of care. These are briefly discussed below.
What are some examples of comorbidities?
For example, comorbidities such as mental illness or misuse of other substances may interfere with a patient’s ability to seek care (e.g., they are too weak to travel, or these conditions interfere with adherence). In addition, other conditions may be the main focus of a patient’s treatment, with opioid use disorder being ignored or considered less critical to treat. For example:
How many people in the US had pain relievers in 2015?
In 2015, 2 million people (0.8 percent of civilian, non-institutionalized individuals age 12 and older in the U.S.) had a prescription pain reliever disorder, and some 12.5 million people (4.7 percent of individuals age 12 and older) had misused prescription pain relievers in the previous year (Bose et al. 2016, Hughes et al. 2016). Rates of prescription opioid use and misuse differed among population groups (Table 2-1).
What are the components of Medicaid?
Below, we describe three components that contribute to this success: screening and early intervention, naloxone use, and medication-assisted treatment.
Is opioid use disorder a moral weakness?
Opioid use disorder, although increasingly recognized as a medical illness, has historically been seen as a moral weakness or willful choice (Olsen and Sharfstein 2014, White 2009). Within the substance use disorder treatment community, many still believe that recovery should not involve the use of medications such as methadone or buprenorphine, and that treatment with these medications is simply substituting one addiction for another. As a result, providers of residential treatment may force patients receiving methadone or buprenorphine to taper off the medication as a condition of treatment. Even the language associated with drug treatment (“clean” or “dirty” urine samples, “clean” status associated with lack of using drugs) perpetuates the stigma associated with substance use disorder (Olsen and Sharfstein 2014). Heroin use disorder, because of its illegality, has particularly high stigma attached to it.
What are the regulations for Medicaid?
In designing effective treatment models, Medicaid ocials and clinicians frequently raise concerns about federal regulations at 42 CFR Part 2 , often referred to simply as Part 2, which are designed to protect patient privacy but may make it dicult to share information among providers. These regulations govern the confidentiality of substance use disorder records and originate in legislation from the 1970s that sought to address the stigma of substance use disorders and concerns that the people seeking treatment could be subject to criminal prosecution and other serious consequences such as loss of employment, housing, or child custody. The restrictions upon the disclosure and use of substance use disorder patient records currently apply to any federally funded individual or entity, other than a general medical facility, that, “holds itself out as providing, and provides, substance use disorder diagnosis, treatment, or referral for treatment.” It also applies to any identified unit within a general medical facility that holds itself out in the same way, as well as, “[m]edical personnel or other staff in a general medical facility whose primary function is the provision of substance use disorder diagnosis, treatment, or referral for treatment and who are identified as such providers” (42 CFR 2.11).
How does Medicaid help with opioids?
The Opioid Epidemic and Medicaid's Role in Facilitating Access to Treatment 1 Among nonelderly adults with OUD, those with Medicaid were more likely than those with other coverage to have received treatment in 2017. 2 Medicaid facilitates access to treatment by covering inpatient and outpatient treatment services, as well as medications and therapy prescribed as part of Medication-Assisted Treatment (MAT). 3 States use Medicaid Section 1115 waivers and other program authorities to expand treatment options for enrollees with OUD. 4 While additional states expanding Medicaid could increase coverage and access, for new work and premium requirements could impose barriers to obtaining and maintaining Medicaid coverage.
How many states have expanded Medicaid?
Additionally, as of May 2019, 36 states and Washington, D.C. have adopted Medicaid expansion, with enhanced federal funding, to cover adults with income up to 138% of the federal poverty level ($17,236 for an individual in 2019).
How many people died from opioids in 2017?
In 2017, nearly two million nonelderly adults had opioid use disorder (OUD) 1,2 and there were 47,600 opioid overdose deaths in the United States, more than double the number in 2007.
What is Medicaid Section 1115?
Medicaid facilitates access to treatment by covering inpatient and outpatient treatment services, as well as medications and therapy prescribed as part of Medication-Assisted Treatment (MAT). States use Medicaid Section 1115 waivers and other program authorities to expand treatment options for enrollees with OUD.
What is Medicaid for substance use disorder?
State Medicaid programs cover numerous substance use disorder treatment services that fit into several state plan categories, including outpatient treatment, inpatient treatment, prescription drugs, and rehabilitation services. The standard of care for OUD is medication-assisted treatment (MAT), which combines one of three medications (methadone, buprenorphine, or naltrexone) with counseling and other support services. 5 All state Medicaid programs cover at least one medication used as part of MAT and most cover all three of these medications. 6 State Medicaid programs also cover many counseling and other support services, delivered either as part of MAT or separately. Most of these services are delivered at state option and include detoxification, intensive outpatient treatment, psychotherapy, peer support, supported employment, partial hospitalization, and inpatient treatment.7
Does Medicaid cover OUD?
As with these other public health crises, Medicaid provides health coverage and access to necessary health care for those struggling with OUD. Additionally, as of May 2019, 36 states ...
How Many Medicaid Enrollees Have Opioid Addiction?
How Much Does Medicaid Spend on Enrollees with Opioid Addiction?
- Medicaid covers a broad range of services for people with opioid addiction, spending $9.4 billion on their care in FY 2013. Medicaid provides both addiction treatment services, such as inpatient detoxification, intensive outpatient treatment, and medication-assisted treatment, as well as other services for health conditions either associated with or independent from opioid addiction.3Man…
How Would The BCRA Affect States’ Ability to Address The Opioid Epidemic?
- Medicaid remains on the front lines for treatment of opioid addiction providing $9.4 billion in spending for enrollees with opioid addiction in 2013 and undoubtedly more today as the epidemic increases and coverage of the expansion population boosts Medicaid’s role. On July 13th 2017, the Senate released a revised discussion draft of the BCRA, whic...
Looking Ahead
- The opioid epidemic has led to substantial health complications, increased health care services utilization, and considerable societal costs. Medicaid has played a critical role in addressing the epidemic by facilitating access to addiction treatment services, including medication-assisted treatment. Medicaid has also facilitated access to other health services for enrollees with opioi…